Tuberculosis (TB) is a major public health problem caused by infection with Mycobacterium tuberculosis, or rarely with certain other species of Mycobacterium.1 Worldwide, TB causes more deaths than any other infectious disease and World Health Organization (WHO) TB data for 2015 indicated there were 10.4 million new cases and 1.8 million deaths.2
In Europe, the incidence of TB has decreased at an average rate of 5.0% per year since 2001, and Europe has the lower TB burden comparing to other continents.3,4 The same has happened in Portugal with a steady decrease of the incidence in the last years. However, Portugal had the highest incidence rate and prevalence among western European countries in 2015.5
Despite abundant epidemiological data, no studies, to the best of our knowledge, have yet examined the clinical, geographic, and epidemiologic burden of TB hospitalizations in Portugal and their changes over time, instead other European countries, like Spain,6 France and Italy.7 Our purpose was to identify the characteristics of patients hospitalized with TB in the public hospitals of mainland Portugal between 2000 and 2015.
This retrospective observational study used data from the nation-wide hospitalization database of Portugal, provided by the Central Administration of Health System of the Portuguese Ministry of Health (ACSS, IP). These data include administrative and clinical data of hospitalization episodes in mainland Portuguese public hospitals over a period of sixteen years (discharges between 2000 and 2015). Data from private hospitals is not part of this database. The records of all inpatients with a principal or secondary diagnosis of TB (coded as 010.xx – 018.xx) were examined. Principal diagnosis represents the clinical condition responsible for the hospitalization and secondary diagnosis describes those conditions that coexists at the time of admission, or develops subsequently, and that affect the patient care for the current episode. Each hospitalization and readmission was considered an independent episode. The anonymity of all patients was maintained during the analysis of the database.
For each hospitalization episode, the following variables were analyzed: sex, birth date, comorbidities (e.g. HIV co-infection), length of stay (LoS), patient residence, and discharge status. There were no age restrictions, and patients were divided into 6 age groups (≤5 years; 6–15 years; 16–25 years; 26–45 years; 46–65 years, and >65 years). Birth date was unavailable for one episode. TB hospitalization rate per 100,000 people and mortality indicators [in-hospital death and in-hospital premature death, in-hospital mortality rate and Potential Years of Life Lost (PYLL)] were calculated.
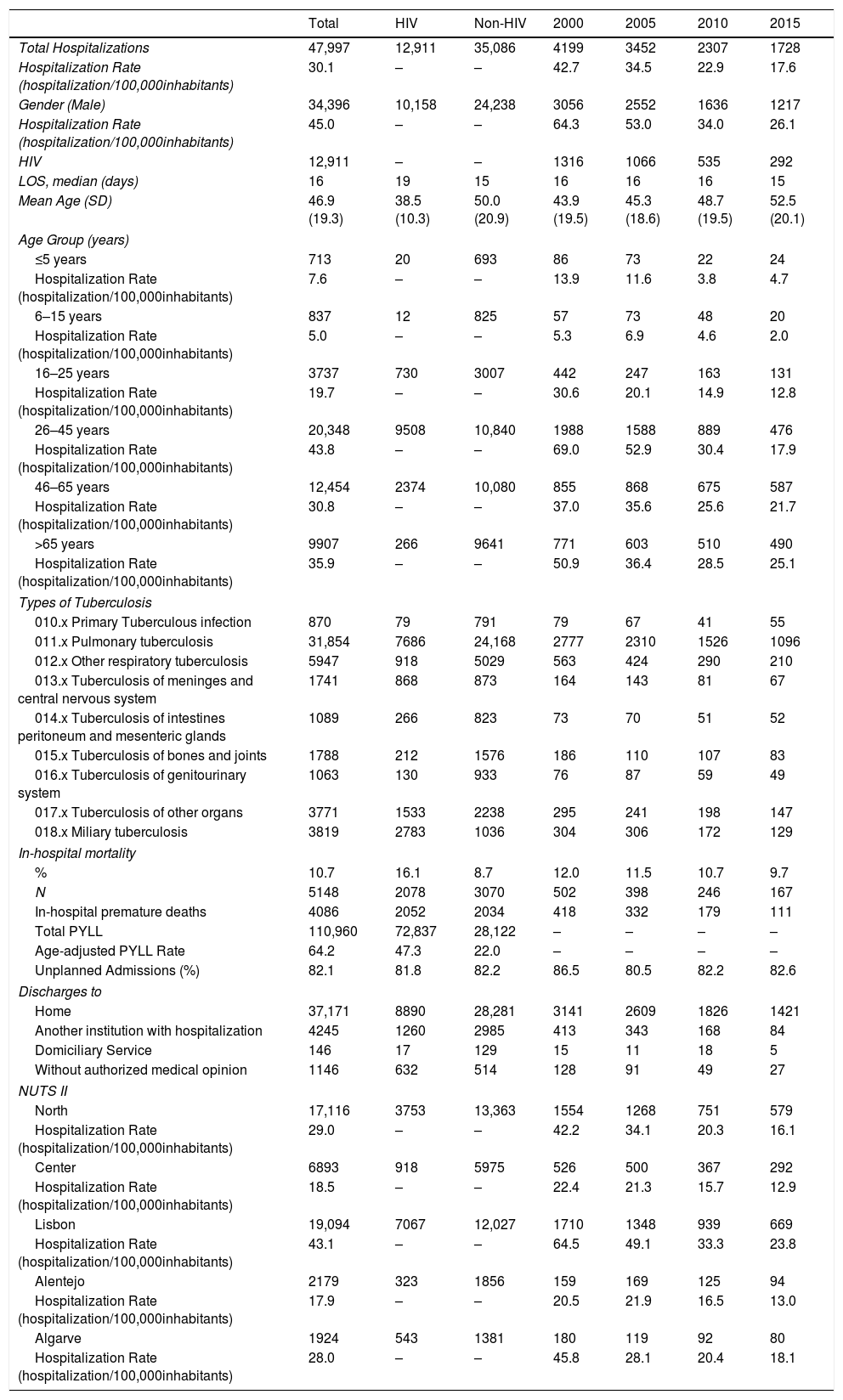
There were 47,997 hospitalizations for TB in the public hospitals of mainland Portugal from 2000 to 2015 (Table 1), with 58.7% (n=28,171) for principal TB episodes and the other 41.3% for secondary diagnosis. HIV infection (n=48.3%), pneumonia (except that caused by tuberculosis or sexually transmitted disease) (n=5.5%) and chronic obstructive pulmonary disease and bronchiectasis (n=2.1%) are the most common secondary diagnosis for TB hospitalization.
Clinical and demographic characteristics of TB hospitalizations in Portugal, between 2000 and 2015.
| Total | HIV | Non-HIV | 2000 | 2005 | 2010 | 2015 | |
|---|---|---|---|---|---|---|---|
| Total Hospitalizations | 47,997 | 12,911 | 35,086 | 4199 | 3452 | 2307 | 1728 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 30.1 | – | – | 42.7 | 34.5 | 22.9 | 17.6 |
| Gender (Male) | 34,396 | 10,158 | 24,238 | 3056 | 2552 | 1636 | 1217 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 45.0 | – | – | 64.3 | 53.0 | 34.0 | 26.1 |
| HIV | 12,911 | – | – | 1316 | 1066 | 535 | 292 |
| LOS, median (days) | 16 | 19 | 15 | 16 | 16 | 16 | 15 |
| Mean Age (SD) | 46.9 (19.3) | 38.5 (10.3) | 50.0 (20.9) | 43.9 (19.5) | 45.3 (18.6) | 48.7 (19.5) | 52.5 (20.1) |
| Age Group (years) | |||||||
| ≤5 years | 713 | 20 | 693 | 86 | 73 | 22 | 24 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 7.6 | – | – | 13.9 | 11.6 | 3.8 | 4.7 |
| 6–15 years | 837 | 12 | 825 | 57 | 73 | 48 | 20 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 5.0 | – | – | 5.3 | 6.9 | 4.6 | 2.0 |
| 16–25 years | 3737 | 730 | 3007 | 442 | 247 | 163 | 131 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 19.7 | – | – | 30.6 | 20.1 | 14.9 | 12.8 |
| 26–45 years | 20,348 | 9508 | 10,840 | 1988 | 1588 | 889 | 476 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 43.8 | – | – | 69.0 | 52.9 | 30.4 | 17.9 |
| 46–65 years | 12,454 | 2374 | 10,080 | 855 | 868 | 675 | 587 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 30.8 | – | – | 37.0 | 35.6 | 25.6 | 21.7 |
| >65 years | 9907 | 266 | 9641 | 771 | 603 | 510 | 490 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 35.9 | – | – | 50.9 | 36.4 | 28.5 | 25.1 |
| Types of Tuberculosis | |||||||
| 010.x Primary Tuberculous infection | 870 | 79 | 791 | 79 | 67 | 41 | 55 |
| 011.x Pulmonary tuberculosis | 31,854 | 7686 | 24,168 | 2777 | 2310 | 1526 | 1096 |
| 012.x Other respiratory tuberculosis | 5947 | 918 | 5029 | 563 | 424 | 290 | 210 |
| 013.x Tuberculosis of meninges and central nervous system | 1741 | 868 | 873 | 164 | 143 | 81 | 67 |
| 014.x Tuberculosis of intestines peritoneum and mesenteric glands | 1089 | 266 | 823 | 73 | 70 | 51 | 52 |
| 015.x Tuberculosis of bones and joints | 1788 | 212 | 1576 | 186 | 110 | 107 | 83 |
| 016.x Tuberculosis of genitourinary system | 1063 | 130 | 933 | 76 | 87 | 59 | 49 |
| 017.x Tuberculosis of other organs | 3771 | 1533 | 2238 | 295 | 241 | 198 | 147 |
| 018.x Miliary tuberculosis | 3819 | 2783 | 1036 | 304 | 306 | 172 | 129 |
| In-hospital mortality | |||||||
| % | 10.7 | 16.1 | 8.7 | 12.0 | 11.5 | 10.7 | 9.7 |
| N | 5148 | 2078 | 3070 | 502 | 398 | 246 | 167 |
| In-hospital premature deaths | 4086 | 2052 | 2034 | 418 | 332 | 179 | 111 |
| Total PYLL | 110,960 | 72,837 | 28,122 | – | – | – | – |
| Age-adjusted PYLL Rate | 64.2 | 47.3 | 22.0 | – | – | – | – |
| Unplanned Admissions (%) | 82.1 | 81.8 | 82.2 | 86.5 | 80.5 | 82.2 | 82.6 |
| Discharges to | |||||||
| Home | 37,171 | 8890 | 28,281 | 3141 | 2609 | 1826 | 1421 |
| Another institution with hospitalization | 4245 | 1260 | 2985 | 413 | 343 | 168 | 84 |
| Domiciliary Service | 146 | 17 | 129 | 15 | 11 | 18 | 5 |
| Without authorized medical opinion | 1146 | 632 | 514 | 128 | 91 | 49 | 27 |
| NUTS II | |||||||
| North | 17,116 | 3753 | 13,363 | 1554 | 1268 | 751 | 579 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 29.0 | – | – | 42.2 | 34.1 | 20.3 | 16.1 |
| Center | 6893 | 918 | 5975 | 526 | 500 | 367 | 292 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 18.5 | – | – | 22.4 | 21.3 | 15.7 | 12.9 |
| Lisbon | 19,094 | 7067 | 12,027 | 1710 | 1348 | 939 | 669 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 43.1 | – | – | 64.5 | 49.1 | 33.3 | 23.8 |
| Alentejo | 2179 | 323 | 1856 | 159 | 169 | 125 | 94 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 17.9 | – | – | 20.5 | 21.9 | 16.5 | 13.0 |
| Algarve | 1924 | 543 | 1381 | 180 | 119 | 92 | 80 |
| Hospitalization Rate (hospitalization/100,000inhabitants) | 28.0 | – | – | 45.8 | 28.1 | 20.4 | 18.1 |
The overall hospitalization rate during this time was 30.1/100,000/year, and this number decreased by 58.8% during the study period (2000: 42.7/100,000; 2015: 17.6/100,000).
Individuals 26–45 years old had the highest overall hospitalization rate (43.8/100,000/year; Table 1), and the hospitalization rate in this group decreased by 74.1% during the study period (2000: 69.0/100,000; 2015: 17.9/100,000). The overall hospitalization rate was greater for males (45.0/100,000/year) than females (16.4/100,000/year). Moreover, the hospitalization rates declined over time for both sexes (males: 64.3/100,000 in 2000 to 26.1/100,000 in 2015; females: 22.4/100,000 in 2000 to 9.9/100,000 in 2015) (Table 1).
Pulmonary TB (011.x) was the most common type of TB (66.4%), followed by other respiratory TB (012.x) (12.5%). Primary TB infection (010.x) accounted for only 1.8% of all admissions (Table 1).
A total of 12,911 TB patients were HIV co-infected (26.9% of all TB hospitalizations) (Table 1). In males, simultaneous HIV and TB accounted for 78.7% of all TB admissions.
The in-hospital mortality rate was 10.7%, corresponding to 5148 in-hospital deaths (Table 1). A total of 38.7% of these cases (1991 episodes) presented with TB as the main diagnosis and 78.6% were males (4,046 episodes). The in-hospital mortality rate was higher in the elderly (>65 years old).
We also examined the geographic distribution of TB hospitalizations using the NUTS II classification (Table 1). Lisbon had the highest rate of TB hospitalizations, followed by the North. Lisbon and Porto had the highest age-standardized TB hospitalization rates, 46.0/100,000 and 38.4/100,000, respectively. Moreover, during the 16 year study period, all districts had declining hospitalization rates, except for Castelo Branco, which had an increase of 20% between 2000 and 2015 (2000: 36.8/100,000; 2015: 41.3/100,000). Castelo Branco had the highest TB hospitalization age-standardized rate in Portugal in 2015.
Interestingly, we also found a trend for decreasing TB hospitalizations over time. Up until 2007, the TB hospitalization rate was close to or a bit higher than the TB notification rate, and clearly higher than the TB incidence rate. However, after 2007, the TB hospitalization rate decreased more rapidly than the notification and incidence rates. This suggests a change in the criteria used for TB hospitalization.
These results highlight that TB continues to be a major public health problem in Portugal that requires more attention. Further studies should focus on the criteria used for TB hospitalization and its impact on outcome, and the reason for the high TB hospitalization rate in Castelo Branco.
The authors would like to thank the Portuguese Ministry of Health's Authority for Health Services (Administração Central do Sistema de Saúde I.P. – ACSS) for providing access to national hospitalizations data.
We would also like to thank H. Gonçalves, for the elaboration of the maps.