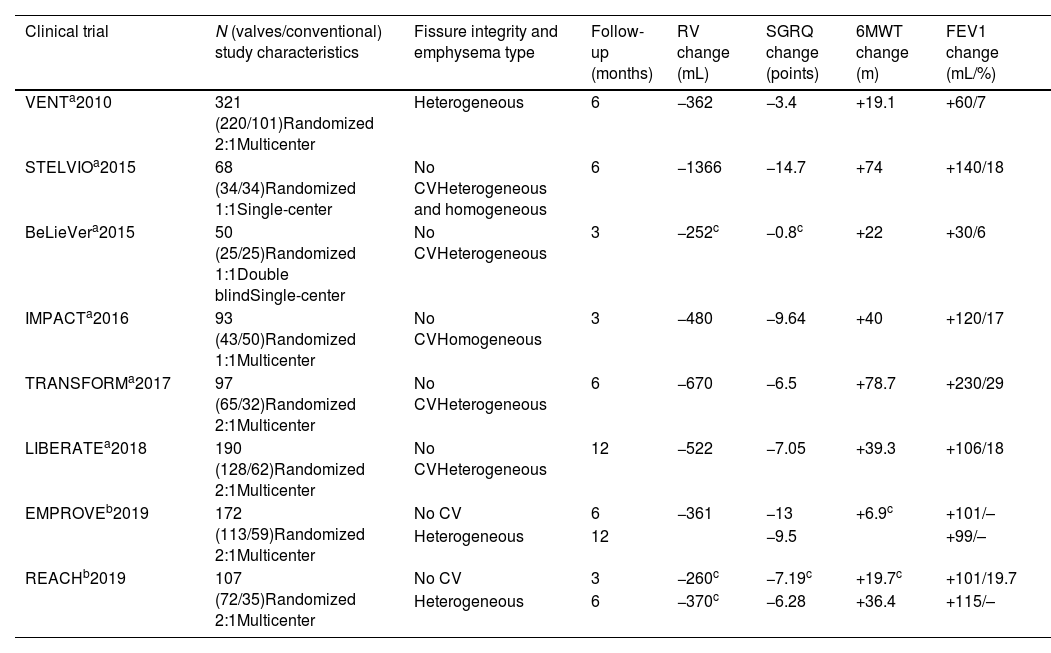
Patients with severe pulmonary emphysema associated with hyperinflation and incapacitating dyspnea now have access to therapy that can change their quality of life and the course of their disease. Our task as respiratory specialists is to identify, evaluate, and select patients who are likely to benefit from endoscopic lung volume reduction (ELVR), once all other therapeutic, pharmacological and non-pharmacological interventions have been exhausted (smoking abstinence, vaccination, physical activity, respiratory rehabilitation, oxygen therapy, and mechanical ventilation). International guidelines such as GOLD1 or GesEPOC2 include ELVR among the recommended treatment strategies. Indeed, the use of endoscopic valves as first-line treatment is a Grade A recommendation based on evidence from a large number of clinical trials3–10 (Table 1) that have evolved into follow-up cohort studies. All published studies have shown that ELVR using valves offers clinically significant benefits in lung function, exercise capacity, and quality of life that are maintained for up to 12 months. Hartman et al. also recently found that volume reduction is an independent survival factor after adjustment for age, gender, and disease severity in a cohort of patients with ELVR (73% with valves) versus conventional treatment.11
Published Clinical Trials.
| Clinical trial | N (valves/conventional) study characteristics | Fissure integrity and emphysema type | Follow-up (months) | RV change (mL) | SGRQ change (points) | 6MWT change (m) | FEV1 change (mL/%) |
|---|---|---|---|---|---|---|---|
| VENTa2010 | 321 (220/101)Randomized 2:1Multicenter | Heterogeneous | 6 | −362 | −3.4 | +19.1 | +60/7 |
| STELVIOa2015 | 68 (34/34)Randomized 1:1Single-center | No CVHeterogeneous and homogeneous | 6 | −1366 | −14.7 | +74 | +140/18 |
| BeLieVera2015 | 50 (25/25)Randomized 1:1Double blindSingle-center | No CVHeterogeneous | 3 | −252c | −0.8c | +22 | +30/6 |
| IMPACTa2016 | 93 (43/50)Randomized 1:1Multicenter | No CVHomogeneous | 3 | −480 | −9.64 | +40 | +120/17 |
| TRANSFORMa2017 | 97 (65/32)Randomized 2:1Multicenter | No CVHeterogeneous | 6 | −670 | −6.5 | +78.7 | +230/29 |
| LIBERATEa2018 | 190 (128/62)Randomized 2:1Multicenter | No CVHeterogeneous | 12 | −522 | −7.05 | +39.3 | +106/18 |
| EMPROVEb2019 | 172 (113/59)Randomized 2:1Multicenter | No CV | 6 | −361 | −13 | +6.9c | +101/– |
| Heterogeneous | 12 | −9.5 | +99/– | ||||
| REACHb2019 | 107 (72/35)Randomized 2:1Multicenter | No CV | 3 | −260c | −7.19c | +19.7c | +101/19.7 |
| Heterogeneous | 6 | −370c | −6.28 | +36.4 | +115/– |
The main characteristic of these patients is dyspnea that interferes with activities of daily living. The underlying mechanisms of this type of dyspnea are complex, but the role of pulmonary hyperinflation (PH) in the pathophysiology of dyspnea and poor exercise tolerance has been known for years.12 PH consists of a static component resulting from parenchymal destruction and loss of elastic recoil combined with a dynamic component which occurs when patients inhale air before achieving full exhalation. For this reason, the thorax of these patients is distended and their diaphragm is flattened from an attempt to compensate for chronic obstruction and static PH. In a situation of increased ventilatory demand, during exercise for example, the muscle fibers are shortened to the maximum, making it difficult to fully exhale, thus leading to excessive fatigue at the onset of exercise.
The aim of ELVR with valves is to decrease excess volume in order to reduce static PH, thus relieving dynamic PH and thereby improving pulmonary mechanics and, therefore, dyspnea. For this reason, the lung areas that show the most destruction and, as such, the most involvement and greatest volumes of trapped air are selected. Unidirectional valves are placed to induce lobar atelectasis in the segmental bronchi of the selected lobe. At this point, the most important factors to consider are collateral ventilation and complete fissures, as the absence of the former and the presence of the latter are essential for the success of the treatment. In fact, appropriate patient selection, i.e. those with excess trapped air and no collateral ventilation, is the most important predictive factor for successful treatment. Upper, middle, and/or lower lobes with either homogeneous or heterogeneous emphysema can be treated, but the lobe to be treated must be independent of the contiguous ipsilateral lobe.
Quantitative analysis using specific software (StratX®, PulmonX Inc., Redwood City, CA, USA) based on thoracic computed tomography results provides data on the destruction of emphysema at −910 and −950 Hounsfield units and on fissure integrity expressed as a percentage. Because the absence of collateral ventilation is essential to achieve the desired objective, when it cannot be entirely ruled out based on an analysis of fissure integrity, it must be validated in vivo using the CHARTIS® system (PulmonX Inc., Redwood City, CA, USA).13 The CHARTIS® pulmonary evaluation system requires bronchoscopy and consists of a catheter with an occlusion balloon and a flow and pressure sensor at its distal tip that occludes the treatment lobe for no more than 5min in order to confirm the absence of flow through the shared fissure, a key characteristic of lobar atelectasis.
The most frequent complication of valve placement is pneumothorax (26%) resulting from a change in pressure in the contiguous lobe following collapse of the target lobe.8 It is treated in the same way as regular pneumothorax. The most feared complication is persistent air leak following pneumothorax, a situation that would require valve removal. For this reason, it seems advisable in certain circumstances to treat a lobe sequentially to avoid abrupt displacement of the untreated lobe.14 Pneumothorax may also be avoided by performing chest ultrasound before treatment to visualize any displacement of the pleura in order to rule out pleural adhesions. Selective and sequential treatment of the segmental bronchi with valves may decrease the number or severity of episodes of pneumothorax. Despite this risk, the safety of valve treatment is acceptable.
Valve treatment has been shown to be beneficial in a group of patients with few other therapeutic alternatives, but the drawback is that only patients with complete fissures and no collateral ventilation are candidates for this intervention. Studies reversing incomplete fissures using endoscopic instillation of small amounts of synthetic polymer in the segment adjacent to the fissure are currently ongoing.15 Good results have also been reported with video-assisted thoracoscopic repair of incomplete fissures and subsequent valve placement.16 These lines of investigation offer hope to a large number of patients with emphysema and collateral ventilation.
ELVR with valves has a place in the general therapeutic arsenal for pulmonary emphysema. It is a useful option and one that has a promising future. The next challenges will be to determine the appropriate time of referral, improve methods for selecting the lobe to be treated, correctly define cut-off points for fissure integrity, investigate methods to repair incomplete fissures, gain further insight into the predictive risk of pneumothorax, and even explore the possibility of bilateral treatment.
Conflict of interestsThe authors state that they have no conflict of interests.