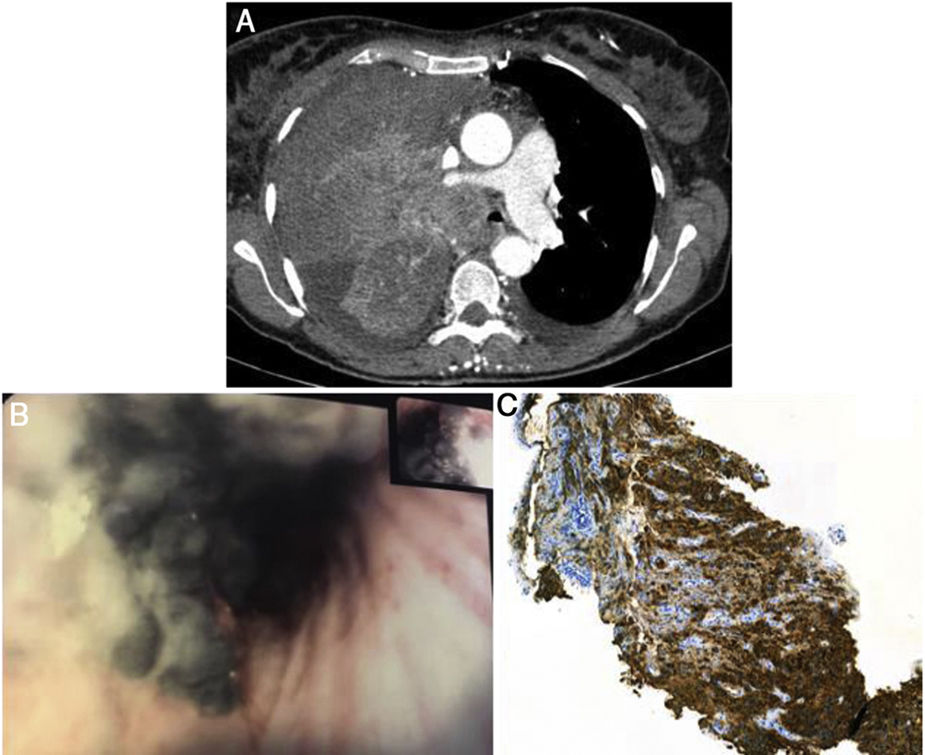
A 54-year-old, non-smoking woman presented with dry cough, asthenia and dyspnea for one month. Six years before, she had a history of left axillary malignant melanoma submitted to surgical treatment with sentinel lymph node biopsy - pathologic staging IB (T2aN0M0). The patient maintained an annual clinical and radiological surveillance, without relapse. On physical examination, she had decreased murmur in the right hemithorax and a palpable right supraclavicular adenopathy. Chest computed tomography showed a massive right upper lobe neoformation with 9cm×12cm (Fig. 1A) with invasion of the right upper lobe bronchus (RULB) and the right pulmonary artery, causing extrinsic compression of the brachiocephalic trunk. Flexible bronchoscopy revealed black pigmented endobronchial lesion, leading to nearly occlusion of the RULB entrance (Fig. 1B). Endobronchial biopsies were compatible with metastatic melanoma (Melan-A and HMB45 expression – Fig. 1C). Due to the progressive brachiocephalic trunk tumoral occlusion, she was referred for emergent palliative radiotherapy, but died shortly thereafter.
A: Chest computed tomography showed right upper lobe mass with 9cm×12cm, with invasion of RULB and the right pulmonary artery. B: Bronchoscopic examination revealed black pigmented endobronchial lesion, leading to partial occlusion of the RULB. C: Immunohistochemical analysis showed Melan-A and HMB45 expression in tumor cells.
Airway black pigmentation can be related with several etiologies such as environmental exposures, infections, iatrogenic and neoplastic causes. Regarding the latter, melanoma is one of the most frequently reported in literature. Pulmonary metastases of melanoma are often asymptomatic but are associated with a poor prognosis.1 This case illustrates the aggressiveness of melanoma even after a long disease-free period,1,2 so any new symptomatology requires a targeted investigation for tumor recurrence.