The identification of bilateral ground-glass opacifications on thoracic computed tomography (CT) in the COVID-19 ongoing pandemic, supports the diagnosis of SARS-CoV-2 infection. Although COVID-19 pneumonia may present with this typical imaging pattern, it is important to highlight that even in an acute clinical setting this pattern it is a non-specific imaging finding and other conditions such as pulmonary oedema, non-infectious pneumonitis and infectious interstitial pneumonia by other pathogens need to be considered.1,2
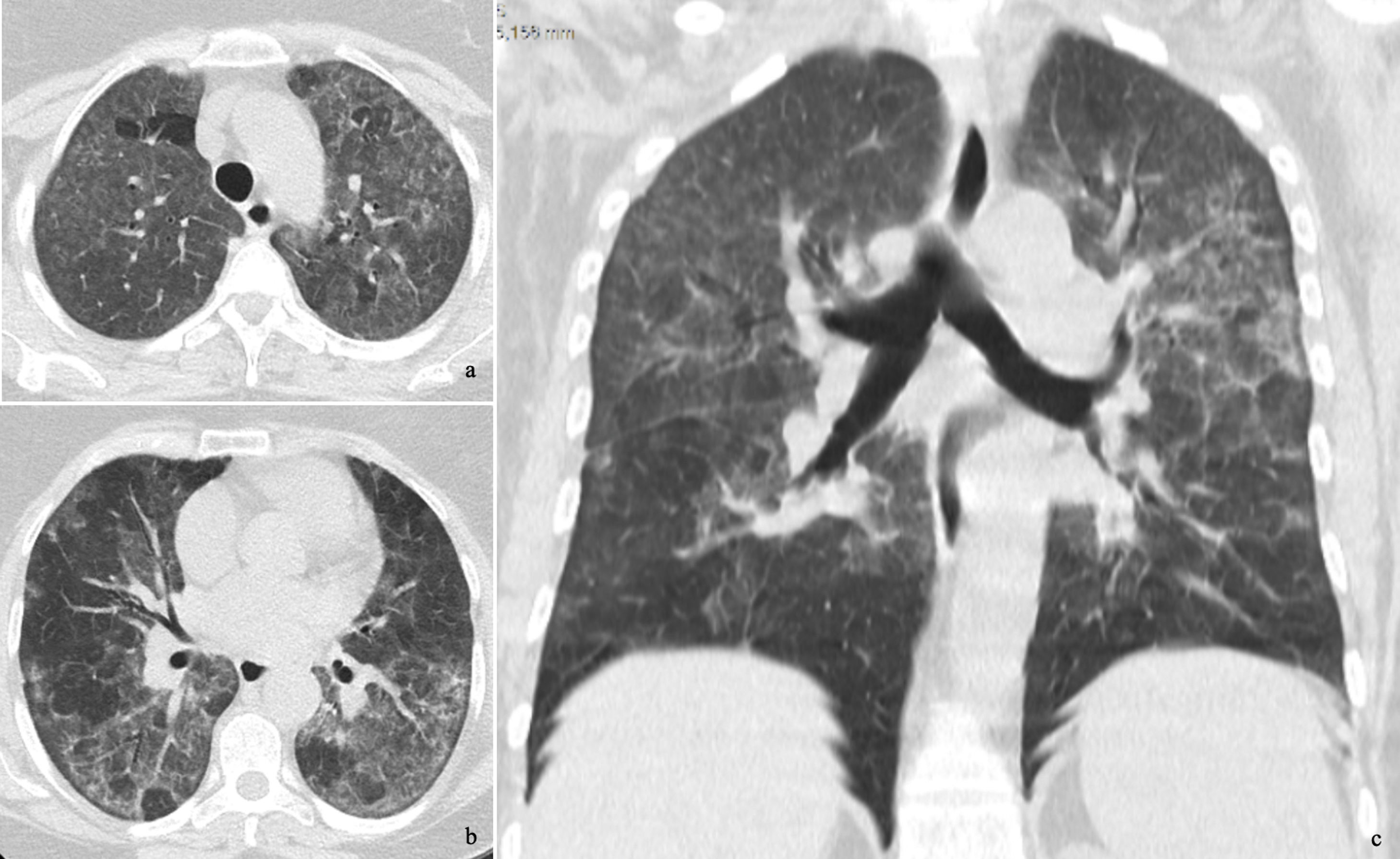
We report the case of a 69-year-old woman who presented to our department in April 2020, during COVID-19 pandemic. On admission, the patient described a 10 day history of progressive dyspnoea and chest pain. There was a 11% of weight loss and occasional wrist and ankle arthralgia, without myalgia, fever or cough. Relevant clinical history included hypertension, allergic rhinosinusitis and psoriasis (on cyclosporine treatment, discontinued in 2018). On physical exam she had tachypnoea, inspiratory crackles in the lung bases and a peripheral oxygen saturation (SpO2) of 89%. Laboratory findings revealed normal white blood cell count, an increased high-sensitivity C-reactive protein (3.70mg/dL N.R.<0.5mg/dL), lactate dehydrogenase (308U/L >250U/L) and erythrocyte sedimentation rate (60mm/h <20mm/h) with procalcitonin value within the reference range (0.09ng/mL <0.5ng/mL). Immunological and microbiological studies (including a swab test for RT-PCR SARS-CoV-2) were negative. Chest radiography showed diffuse bilateral symmetric ill-defined air-space opacities. Chest CT displayed diffuse bilateral ground-glass opacities with lobular spared areas (mosaic attenuation pattern), ill-defined centrilobular ground-glass nodules and mild interlobular thickening, however without the characteristic distribution of COVID-19 (Fig. 1).
The patient was admitted with the presumptive diagnosis of SARS-CoV-2 pneumonia, based on a high probability diagnosis’ score,3 pending a second negative nasopharyngeal swab test for RT-PCR SARS-CoV-2.
On a more detailed clinical history, the patient acknowledged to have a budgerigar at home for about one year. Flexible bronchoscopy showed diffusely friable mucosa. Bronchoalveolar lavage fluid cell count was consistent with alveolitis (28% alveolar macrophages, 42% lymphocytes, 24% neutrophils and 6% eosinophils, with a CD4/CD8 ratio of 2). A diagnosis of Bird Fancier's Lung was confirmed by strongly positive precipitins to budgerigar. The patient initiated inhaled steroids with rapid symptomatic improvement and was discharged home with rest SpO2 of 98%. The budgerigar was removed from the patient's environment and she became totally asymptomatic after a short steroid treatment.4,5
Hypersensitivity pneumonitis (HP) is an immunologically non-IgE-mediated lung disease due to the repetitive inhalation of antigens. Most cases are secondary to residential environmental exposure, particularly birds. Given the time length to onset of symptoms, the causal epidemiological link is often initially unrecognized. The clinical symptoms and imaging findings are nonspecific and may mimic COVID-19 in the ongoing pandemic. Nevertheless, other medical conditions may present with a similar clinical and radiographic findings. In the pandemic time of COVID-19, the presence of alveolar infiltrates urges to consider the hypothesis of this infection. Atypical clinical findings and negative swabs compel us to exclude other etiologies, being of the utmost importance a thorough clinical history.
FundingNone.
Conflict of interestNone.