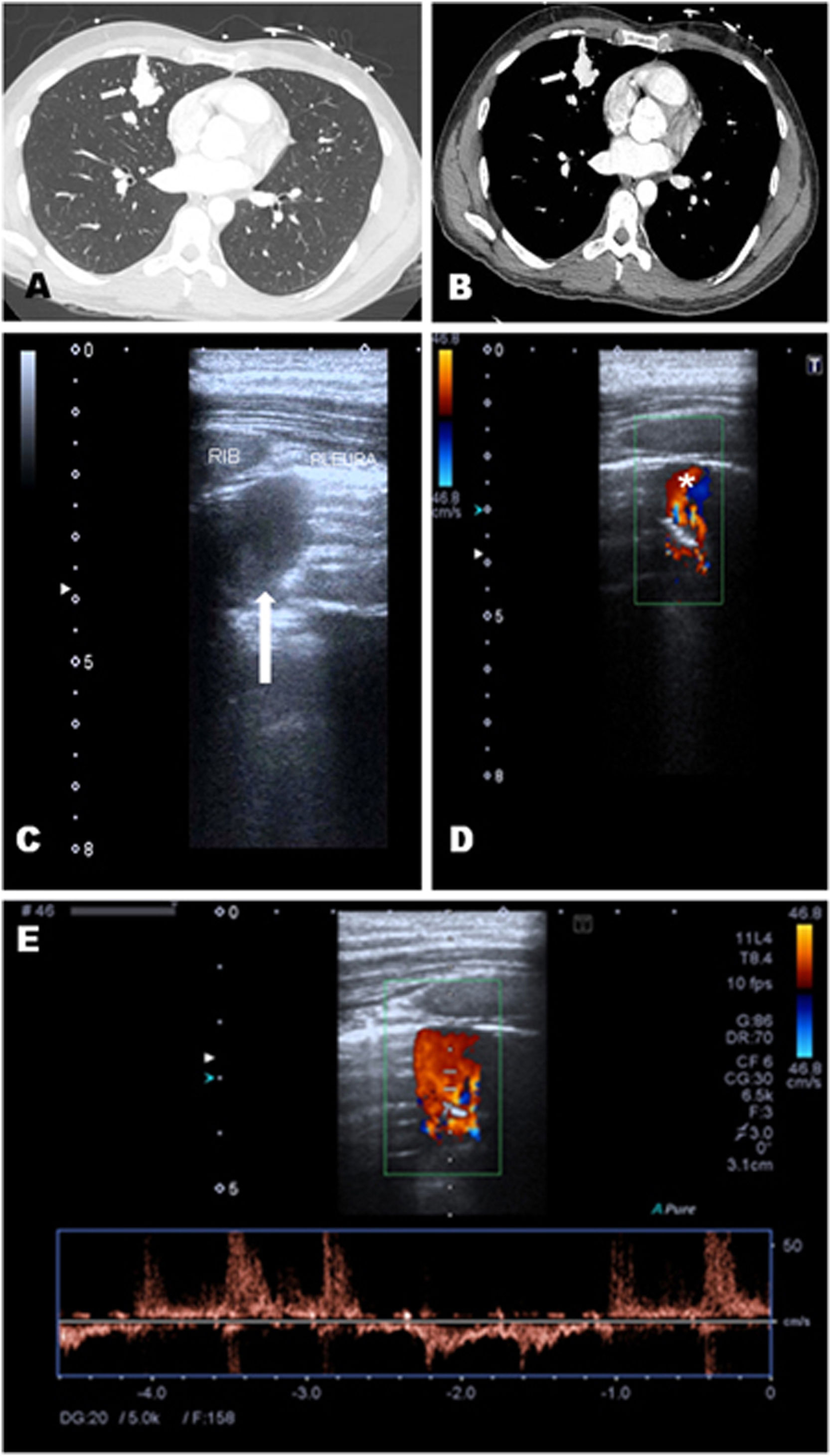
A-33-year-old man, with family history of Rendu–Osler–Weber syndrome, presented with seizures. Brain tomography showed a parietal brain lesion, and chest tomography reported a hyperdense nodular image in the right middle lobe. Lung point of care ultrasound (POCUS) was performed, and a round hypoechoic image with anterograde and retrograde flows was shown (Fig. 1), which moved with the ventilatory pattern. CT pulmonary scan revealed a dilated vascular structure in a coiled arrangement in the right middle lobe with multiple pulmonary arterial branches directly communicating with the pulmonary veins, compatible with complex pulmonary arteriovenous malformation (PAVM). Brain biopsy revealed a brain abscess, so antibiotics were started. Later, he was referred for angioembolisation.
Lung CT revealed a dilated vascular structure in the right middle lobe close to the pleura (A and B, white arrow), compatible with PAVM. Pulmonary echography showed a right parasternal hypoechoic image with an intraluminal hyperechoic area, compatible with thrombosis (C, white arrow). Doppler mode revealed a ‘mosaic-pattern’ indicative of mixing of arterial and venous blood consistent with PAVMs (D). Here, the anterograde and retrograde flow form a “ying-yang sign” (asterisk). Pulsed doppler image demonstrated arterial and venous flows (E).
PAVMs are rare, abnormal low resistance vascular structures that connect a pulmonary artery to a pulmonary vein, resulting in an intrapulmonary right-to-left shunt. The preferred screening test for PAVM is transthoracic contrast echocardiography, while thin section CT scanning is the imaging of choice to diagnose a PAVM.1 However, under certain circumstances, lung POCUS can demonstrate PAVMs. Pulmonary ultrasound perform with a good acoustic window can detect vascular malformations close to pleura, or only partially embedding the parenchyma.2 POCUS is a useful tool to rule out differential diagnosis of pulmonary images.
Authors’ contribution- •
MME wrote the manuscript.
- •
SAN helped with the concept.
- •
LPM edited the manuscript.
Informed consent was obtained from the individual participant included in the study.
FundingAuthors received no financial support for this study.
Conflict of interestThe authors declare that they have no conflict of interest.