The surgical extraction of the third molar is the most frequently carried out procedure in oral surgery.1 Common complications include pain, bleeding, infection, perforation of the maxillary sinus and nerve injury.2 Pneumomediastinum and subcutaneous emphysema are considered to be exceptional, and we therefore present the case of a patient who developed such complications.
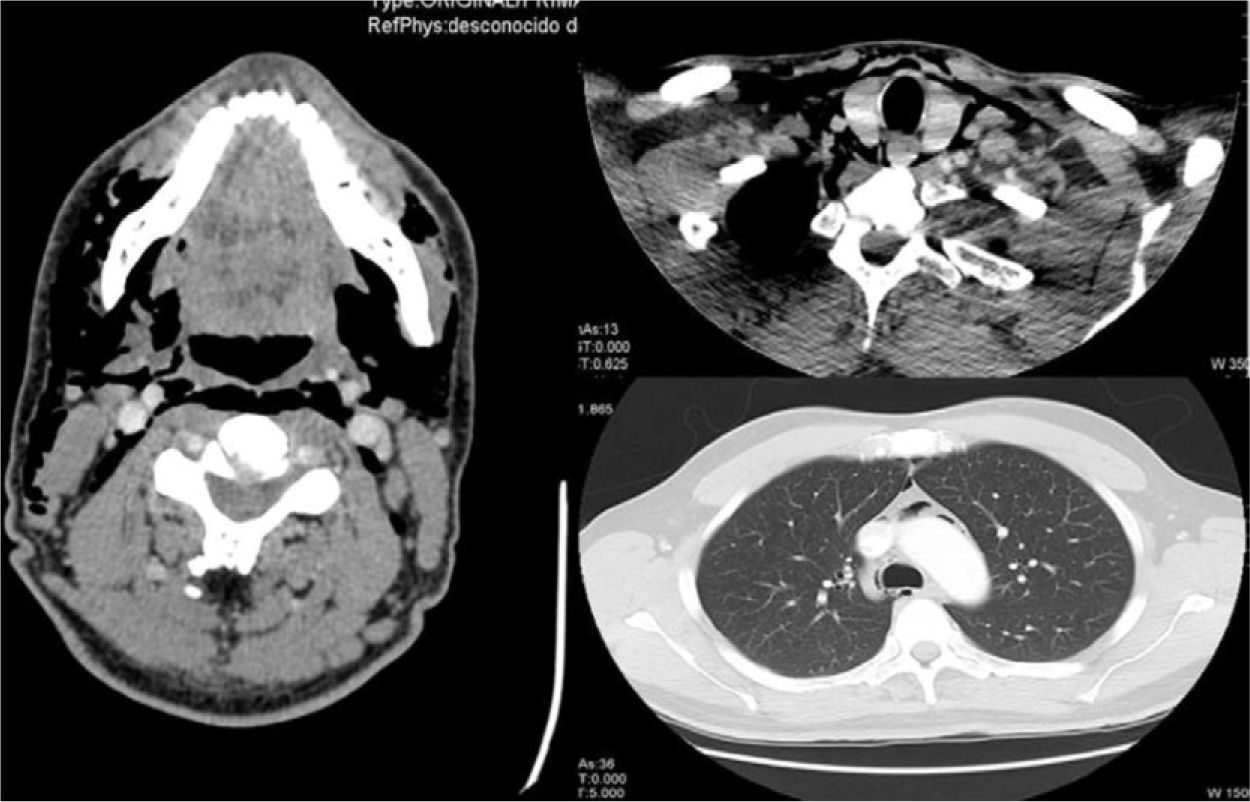
A 30-year-old patient came to the emergency department due to crepitations in the face, neck and thorax after the extraction of the right mandibular third molar the previous day. The patient referred no dyspnea, pain or tumefaction. Upon exploration, the patient was hemodynamically stable, with an oxygen saturation of 100% and evident subcutaneous emphysema on the right side of the face, laterocervical region and right side of the upper thorax. Work-up was normal; cervical and thoracic radiography showed important subcutaneous emphysema and pneumomediastinum, and computed tomography (CT) was done (Fig. 1). The patient was admitted to hospital for prophylactic antibiotics and observation. The evolution was favorable, with a progressive reduction in the emphysema, with no apparent complications, and the patient was therefore discharged four days later.
Cross-sectional CT images of the mandibular, inferior cervical and superior mediastinal areas. There is observed widespread emphysema that dissects the bilateral cervical muscle planes and affects the parapharyngeal and prevertebral spaces, floor of the mouth, submandibular space and posterior cervical space, reaching the mediastinum and causing pneumomediastinum. These findings are asymmetrical and more evident on the right side.
Subcutaneous emphysema as a complication of oral surgery is infrequent (in a prospective study of 100 complications due to molar extraction, there were no patients with this pathology).2 It is produced by the entrance of air in the facial planes of the face and neck through the area of the wisdom tooth extraction. Factors that predispose patients to emphysema have been described, the most frequent of these being the use of a drill3 (with air and water turbines) in up to 80% of cases, which introduces pressurized air at up to 16mmHg. The roots of the first, second and third molars are directly connected with the sublingual and submandibular space. Meanwhile, the sublingual space is connected to the pterygomandibular, parapharyngeal and retropharyngeal spaces. Under pressure, the air enters through the molar roots to the retropharyngeal space, which is connected to the mediastinum. The symptoms may vary depending on the quantity of air, its location and the presence or absence of infection. Thus, we may find anywhere from a simple, self-limiting, subcutaneous emphysema that is practically asymptomatic to, if deeper planes are dissected, pneumomediastinum, pneumothorax or pneumopericardium that, when associated with infection, can cause cellulitis, Lemierre syndrome and mediastinitis.3,4 The majority of patients, however, are paucisymptomatic, like our patient. On physical examination, there are characteristic crepitations to palpation of the thoracic and cervical regions, and Hamman's sign may also be present3 (synchronic crunching with heartbeats), while there may be hypoventilation in the lung fields and deviation of the trachea if there is pneumothorax. The differential diagnosis is established with angioedema, anaphylactic reaction, hematoma and cellulitis.3,5 The diagnosis is radiological, using simple radiography in order to demonstrate the presence of air and CT to rule out associated collections. Emergency surgical decompression is required if there is cardiovascular collapse or obstruction of the airway, but this is uncommon. If the patient is asymptomatic, conservative treatment is recommended, with hospitalization under observation and prophylactic antibiotics in order to rule out the development of an infection. This is necessary because the use of non-sterile air and water during molar extraction has been described as a risk factor for infection.6 In most cases, the subcutaneous emphysema will begin to disappear in 3–5 days. It is important to advise patients to avoid high intraoral pressures as this could increase the introduction of air into the cervical area.
We conclude that the development of subcutaneous emphysema and pneumomediastinum during wisdom tooth extraction is a very uncommon complication, but that it should be kept in mind if an air turbine is used.
FundingThis article has been partially financed by the FFIS (Fundación para la Formación e Investigación Sanitaria de la Región de Murcia, Grupo FFIS-008).
Conflicts of InterestThe authors declare having no conflicts of interest.
Please cite this article as: Guillén-Paredes P, et al. Neumomediastino asintomático tras extracción cordal. Arch Bronconeumol. 2012;48:217–8.