A 67-year-old woman, non-smoker, was diagnosed in June 2018 with acute myeloid leukemia, treated with chemotherapy and haploidentical hematopoietic stem cell (HSCT) transplantation.
Prior to transplantation, the patient developed Klebsiella bacteremia associated with a central venous catheter that was resolved with ceftriaxone and catheter withdrawal. In the microbiological study, a serum galactomannan assay was positive, while chest CT screening for pulmonary aspergillosis was normal and subsequent serum galactomannan assays were negative.
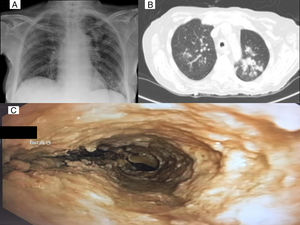
Transplantation took place in February 2019. Immunosuppressive treatment included cyclophosphamide, cyclosporine, and mycophenolate, and the patient received infectious prophylaxis with trimethoprim-sulfamethoxazole, acyclovir, and voriconazole, which was replaced by isavuconazole due to liver toxicity (Fig. 1).
Mycophenolate was discontinued 1 month after HSCT due to persistent residual disease. This loss of immunosuppression led to the development of graft-versus-host disease, which was treated with high-dose methylprednisolone (2 mg/kg/day). During down-dosing, the patient developed respiratory infection with radiological infiltrate in the left upper lobe (LUL). Bronchoscopy was requested, and the endobronchial image was highly suggestive of Aspergillus pseudomembranous tracheobronchitis (Fig. 1). This a case of opportunistic infection, probably favored by corticosteroid therapy.1 The patient received treatment with intravenous amphotericin B and voriconazole, but her progress was poor and she died a few days later.2
Please cite this article as: Pina-Maiquez I, García-Lujan R, Revuelta-Salgado F, Margallo-Iribarnegaray J, Miguel-Poch E. Traqueobronquitis aspergilar. El valor diagnóstico de la imagen endoscópica. Arch Bronconeumol. 2021;57:226.