A 77-year-old man, current smoker (50pack/year) with history of hypertension, dyslipidemia, stage 5 chronic kidney disease with peritoneal dialysis and Crawford's type II thoracoabdominal aortic aneurysm (TAAA) diagnosed in 2016, who had undergone thoracic endovascular aortic repair (TEVAR) surgery with stent-grafts that required secondary endovascular interventions due to multiple endoleaks in 2018, 2020 and 2021.
The patient was admitted to the Emergency Department with frank hemoptysis about 50mL daily in the last 3 days. Over the last 6 months, he had intermittent dorsal and retrosternal thoracic pain with blood-streaked sputum once a day. No dyspnea, fever, trauma or syncope was reported.
On examination, the patient was conscious, eupneic with basal oxygen saturation of 96%, afebrile and hemodynamically stable (BP 138/72mmHg, HR 60bpm), rhonchi and bilateral hypophonesis in the respiratory auscultation.
Blood test showed low hemoglobin (11.9g/dL) and platelet (103,000) counts, normal coagulation profile and altered renal function (urea 93mg/dL and creatinine 6.48mg/dL).
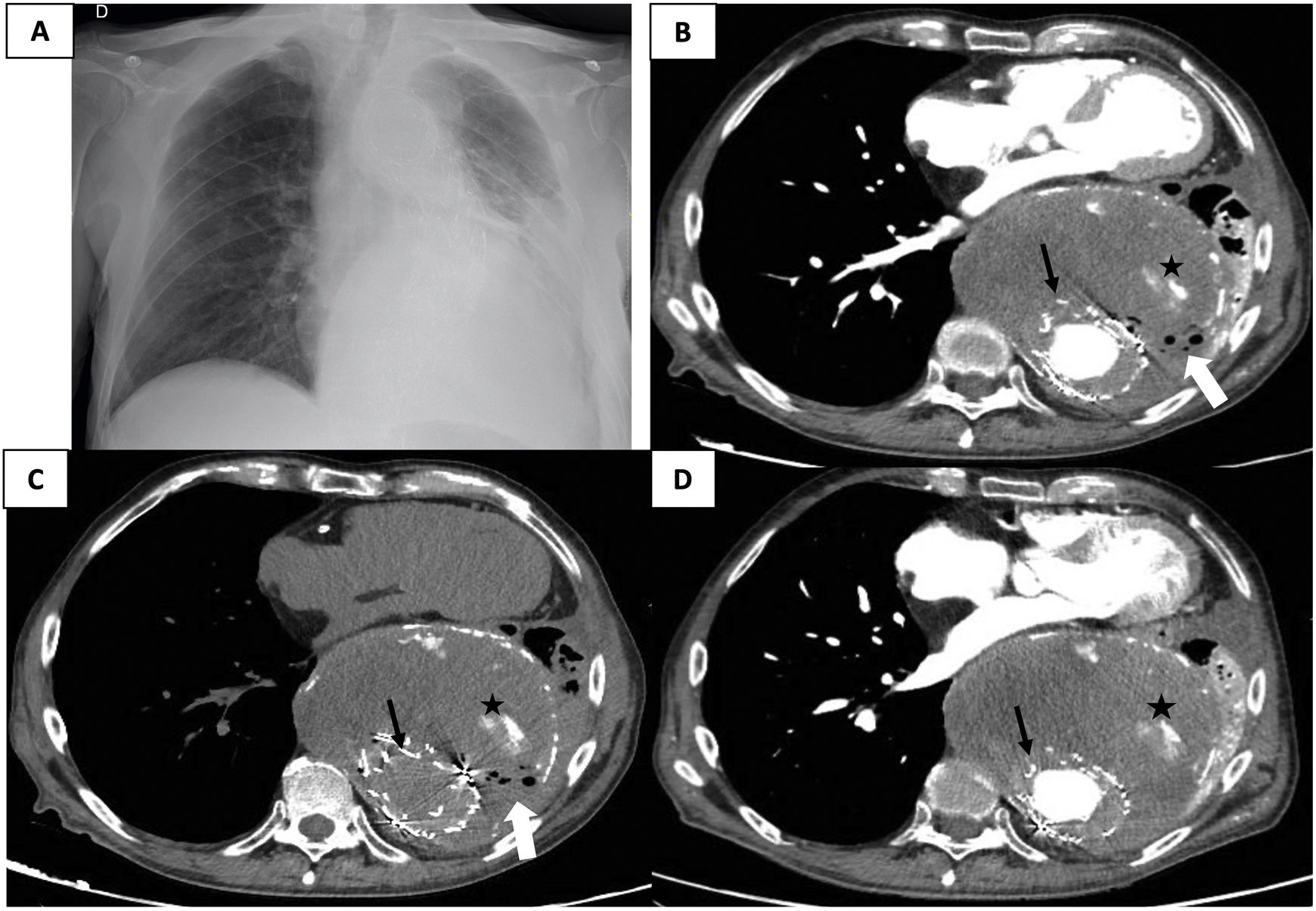
Chest X-ray showed mediastinal widening and a large retrocardiac opacity with significant volume loss of the left pulmonary base (Fig. 1A).
(A) Posteroanterior chest X-ray findings: mediastinal widening due to thoracic aortic aneurysm (TAA) with tracheal deviation to the right and a large retrocardiac opacity with significant volume loss of the left pulmonary base. (B) Contrast-enhanced thoracic computed tomography angiography (CTA) showed a TAA with aortic stent-graft (black-thin-arrow), a large aneurysmal sac (163mm×140mm (TxPA)) with a mural thrombus in it, an atherosclerotic plaque and irregular high attenuation areas within the aneurysmal sac suggesting calcium deposits (black star) similar to previous studies with no evidence of endoleaks and a left lung consolidation with atelectasis. Presence of air bubbles within the thrombosed aneurysm with a suspicious aortobronchopulmonary fistula lesion (white arrow). (C) Non-contrast CTA was useful to distinguish between endoleaks and calcifications within the aneurysmal sac. The high attenuation areas (black star) remained the same with the non-contrast and contrast-enhanced CTA suggesting calcifications. (D) 3 months earlier contrast-enhanced CTA to show the stability of the volume of the TAA, aneurysmal sac, calcifications and left lung atelectasis. No evidence of endoleaks or aortobronchopulmonary fistula.
CTA showed a TAAA with stent-grafts, a bulky aneurysmal sac with a large thrombus and calcium deposits in it and a left lower lung atelectasis (Fig. 1B, C) that were similar to prior studies and no evidence of endoleaks (Fig. 1D). However, a new finding was the presence of air bubbles within the thrombosed aneurysmal sac that suggested a communication with the bronchial tree (Fig. 1B, C).
Regarding treatment, surgical procedures were dismissed due to the unacceptable mortality, failure of previous procedures and patient's poor functional status. The patient and his family were conscious of the fatal prognosis without surgery. Conservative management was adopted with the withdrawal of antiplatelet medication and a course of antibiotic to treat the possible superinfection of the left lung atelectasis. The patient was discharged from hospital with a palliative care management at home.
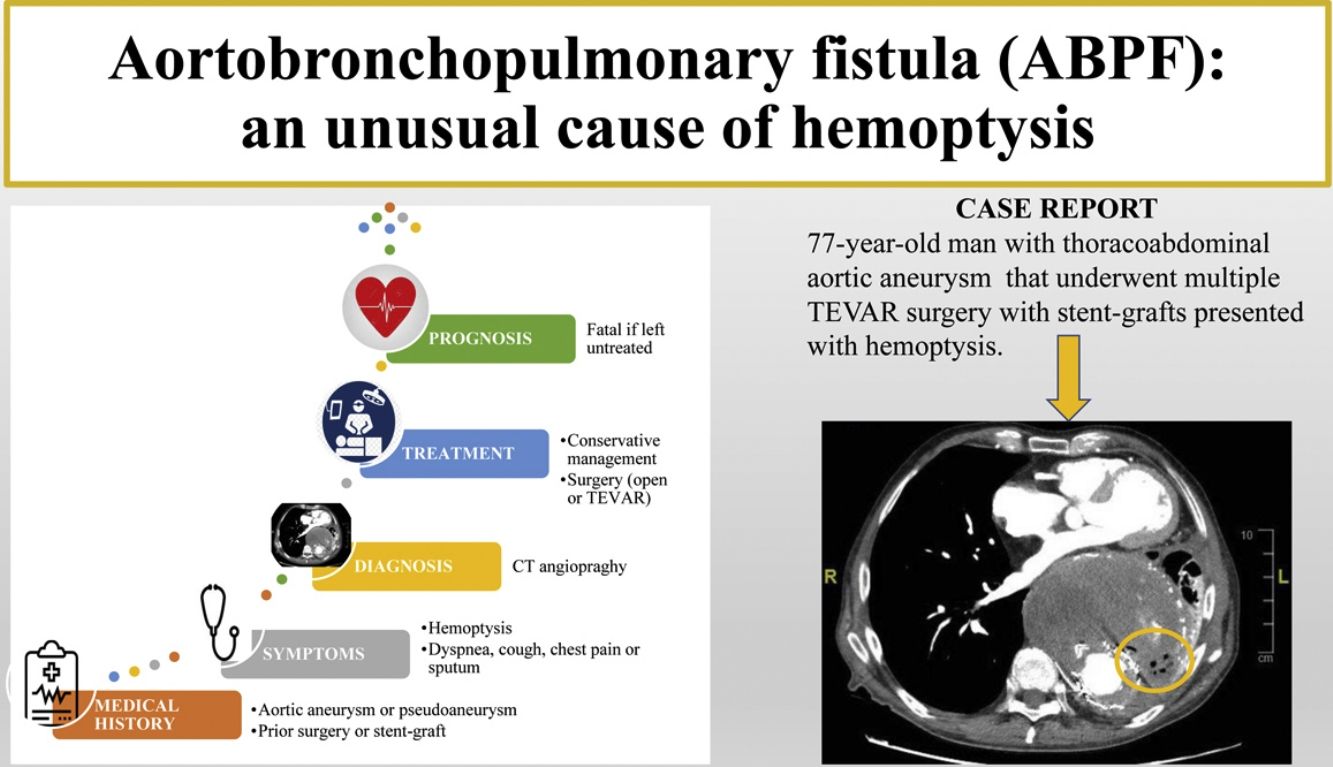
An aortobronchopulmonary fistula (ABPF) is a formation of an abnormal communication between the aorta and the bronchial tree or the lung parenchyma. Nowadays, the most common etiologies are postsurgical and patients with descending atherosclerotic TAA or pseudoaneurysms.1,2
Before 1970, aneurysms caused by tuberculosis, mycotic infections and syphilis were the leading causes.1,3 Other etiologies have been reported such as spontaneous fistulas without aneurysm, associated with congenital heart disease (aortic coarctation or ductus arteriosus), foreign body or trauma.1,2
The pathophysiology behind ABPF seems to be the constant pulsating aneurysm or compression that erodes the lower respiratory tract.1,4 Other mechanisms are inflammatory response due to infection or foreign body reaction (suture material or stent-grafts) causing a pathological adherence to the lung tissue that leads to a fistula.2
ABPF is a rare but potentially fatal condition if left untreated. The diagnosis should be suspected in patients with hemoptysis and TAA. The most common symptom is hemoptysis that could be intermittent and minor due to clot formation, or massive. Other symptoms are dyspnea, cough, chest pain and sputum. The ABPF is an uncommon cause of hemoptysis,1,2 most commonly involving the left lung and descending thoracic aorta due to their narrow anatomical distance.2
Diagnosis is difficult and clinical suspicion is key, because CT angiography usually identify the aneurysm but rarely locate the fistula.3 However, suggestive signs are present like air bubbles within the thrombosed aneurysm, among others.5 Surgery, either open or TEVAR, remains the treatment of choice.1,5
FundingNo funding related to this article.
Conflict of interestNone declared.