Archivos deBronconeumología recently published a case report by Gómez-Seco et al.,1 which informed us of the presence of an entity that has been unknown in our setting until now: anthracostenosis or anthracofibrosis. In this letter, we describe a new clinical case in Spain with particularities similar to the other 3 previously mentioned cases.
Our patient is a 66-year-old woman from a rural area, a non-smoker, with no known history of tuberculosis or exposure to coal, although she had been inhaling wood fire smoke throughout her life. The patient had previously been diagnosed with middle lobe syndrome, and in 2002 she underwent lobectomy of the middle lobe due to recurrent pneumococcal infections.
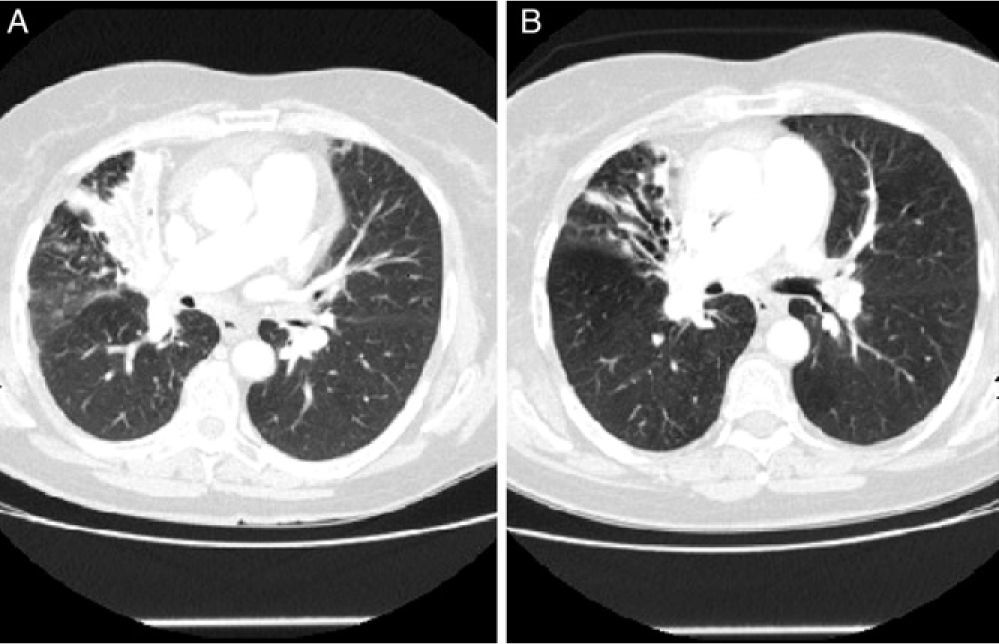
The patient was sent to our department in 2011 with chronic dry cough. Chest radiography revealed right hilar enlargement and atelectasis-partial condensation of the anterior segmental bronchus of the right upper lobe (RUL). Said findings were confirmed by chest CT, which also demonstrated bronchiectasis in the RUL and a right paratracheal adenopathy measuring 2cm (Fig. 1A). Given the suspicion for bronchial carcinoma, bronchoscopy was performed, which showed a middle lobe lobectomy stump with no signs of neoformation and an extensive black patch at the entrance of the bronchus of the left upper lobe. Due to an important amount of bleeding, only one biopsy sample could be taken. The tissue sample contained bronchial mucosa with macrophages in the lamina propria and black cytoplasmic pigment, with no signs of malignancy. The rest of the segmental bronchi of both lungs were impassable due to stenosis, especially in the adjoining airways near the black patch toward the culmen and the lingula. Isoniazid-resistant Mycobacterium tuberculosis was isolated in bronchial secretions.
The patient was treated for 6 months with ethambutol, pyrazinamide, and rifampicin. Afterwards, follow-up CT showed partial resolution of the infiltrate in the anterior segmental bronchus of the RUL with normalization of the size of the adenopathy (Fig. 1B). The endoscopic appearance was unchanged despite the treatment received. New bronchial suction and bronchoalveolar lavage samples confirmed the eradication of the Koch bacillus.
Anthracostenosis or anthracofibrosis was first described in 1998 by Chung et al.2 as an entity that is different from coal workers’ pneumoconiosis. It is most frequent in non-smoker women aged between 60 and 70 who live in rural areas of Asia and sub-Saharan Africa. Its etiopathogenesis has not completely been defined, and several hypotheses have been postulated that are not mutually exclusive. The two main hypotheses regarding triggering agents are the inhalation of smoke from incomplete biomass combustion and pulmonary tuberculosis (TB).1–4 In the former hypothesis, although the ciliary movement eliminates the majority of inhaled particles, there are always residual quantities of accumulated remains at the subdivision points of the airways that activate the alveolar macrophages and alter the cellular immune response, favoring infections.3 The second hypothesis relates anthracostenosis with TB: it is believed to be an exaggerated immune response to M. tuberculosis antigens, with lymph node infarction in the chains adjacent to the bronchi and toward which their caseous content would drain if they ruptured, generating fibrosis.2,3 Bronchoscopy is the main diagnostic test used, and bronchial stenosis should be observed at several levels with patches of anthracotic pigmentation of the bronchial mucosa.3 A proper differential diagnosis should rule out bronchogenic carcinoma and go beyond mere endobronchial tuberculosis (with focal affectation of a single segment or lobe and without patchy distribution).3
Until the publication of the series of 3 cases by Gómez-Seco et al.1 in April 2012, no cases of anthracostenosis had been reported in Spanish patients. This fourth case described in our country is of particular interest due to the conjoint presence of the two main hypothetical triggering factors: exposure to wood-fire smoke and TB. It is important not to forget the fact that wood is still extensively used as a fuel source in Western countries, both in rural settings as well as in low-income urban areas, and it is a risk factor for respiratory diseases such as TB, chronic obstructive pulmonary disease, pneumonia, and cancer.4
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Sacristán Bou L, et al. Antracoestenosis con exposición a humo de biomasa y presencia de Mycobacterium tuberculosis. Arch Bronconeumol. 2013;49:85–6.