Domiciliary oxygen therapy (DOT) is a treatment that requires a high level of cooperation from patients due to the time it takes every day. A high level of non-compliance has been determined among patients receiving DOT. The aim of our study was to assess the level of non-compliance and the influence of active tobacco consumption on compliance.
Material and methodsPatients were monitored in the home using direct and indirect methods, to assess both compliance and tobacco consumption.
ResultsThe level of non-compliance detected by indirect methods was 22.6%, and 66.3% by direct methods. Tobacco consumption determined by indirect methods was 5.8%–8%, depending on the method used, and 16.2% when CO in exhaled air ≥10ppm was established as an indicator of tobacco use. The group of smokers complied with oxygen therapy for a significantly fewer number of hours per day (P<.001) than non-smokers.
ConclusionsThere is a high level of therapeutic non-compliance and a significant percentage of patients receiving DOT continue to smoke. Compliance must be monitored, and the correct use of DOT must be emphasized. Additional efforts should also be made to help smokers with DOT to stop smoking, since continued smoking impacts negatively on therapeutic non-compliance.
La oxigenoterapia crónica domiciliaria (OCD) es un tratamiento que exige una colaboración muy importante por parte de los pacientes debido al elevado número de horas que debe realizarse. Se conoce que existe un elevado nivel de incumplimiento entre los pacientes con OCD. El objetivo de nuestro estudio ha sido valorar el nivel de incumplimiento y la influencia del consumo de tabaco activo sobre el mismo.
Material y métodosSe ha realizado un control en el domicilio de los pacientes utilizando métodos directos e indirectos, tanto para valorar el nivel de cumplimiento como el de consumo de tabaco.
ResultadosEl nivel de incumplimiento detectado por métodos indirectos es del 22,6%, y por métodos directos es del 66,3%. El consumo de tabaco determinado por métodos indirectos es del 5,8% o del 8% dependiendo del método utilizado y del 16,2% cuando se establece un nivel de CO en aire exhalado ≥10ppm como indicativo de fumador. El grupo de fumadores realiza un número de horas/día de oxigenoterapia significativamente menor (p<0,001) que los no fumadores.
ConclusionesExiste un elevado nivel de incumplimiento terapéutico y un porcentaje importante de pacientes con OCD continúa fumando. Es preciso vigilar el cumplimiento, insistiendo en la necesidad de realizar bien la OCD, y se debe realizar también un esfuerzo añadido para ayudar a los fumadores con OCD a dejar de fumar, ya que mantener el consumo de tabaco contribuye a un mayor incumplimiento terapéutico.
Long-term domiciliary oxygen therapy (LTOT) is a widely used intervention, although the supporting evidence, based on classic studies such as the Nocturnal Oxygen Therapy Trial (NOTT)1 and the Medical Research Council (MRC)2 trials conducted in the 1980s in COPD patients, is scant and outdated, and the recommendations of these studies have been extended to other diseases that involve hypoxemia. The criteria for indicating this therapy have not been modified by subsequent studies and reviews, nor has new evidence been established,3 and some authors have suggested that the data supporting some indications are limited.
This generalized application of recommendations has also been accompanied by clinical practices in which the initial freedom of prescription has led to some confusion, most often in the form of clinical errors such as incorrect prescriptions and inadequate follow-up, and therapeutic incompliance, understood in a broad sense,4 resulting in misuse of resources and unjustified healthcare expenditure. We have been aware of this problem for many years5–8; however it has recently acquired greater relevance following calls to curb healthcare spending. In other words, it has become more of a management problem than a healthcare issue, although some authors have now begun to question the magnitude of the problem.9
We are a working group with expertise in conducting both local and multicenter home-based LTOT monitoring studies. In view of the growing importance of home respiratory therapies in general and LTOT in particular, we hypothesized that it would be of interest to conduct a new study investigating these factors in order to help define the current state of the problem.
ObjectiveLTOT requires a great deal of patient collaboration due to the number of hours of treatment needed every day if the expected benefits are to be obtained. The degree of adherence to treatment in these patients and the variables that might influence their compliance must be determined. We believe that much of therapeutic non-compliance is associated with the personal characteristics of the patient or the treatment prescribed. The aim of our study was to assess therapeutic adherence among patients receiving LTOT in a health area and the possible influence of active smoking on compliance.
Materials and MethodsPatientsTwo possible sample selection strategies were considered: a representative sample from the 954 patients who had received LTOT during the month of September 2016 in the health area, or the entire population of patients receiving LTOT during this period; we decided to pursue the latter approach. The study population, then, consisted of all patients who had received LTOT during the month of September 2016 in the healthcare area, a sample of 954 patients in total. Of these, 5 refused to participate in the study, so the final sample size was 949 patients. This was an experimental, cross-sectional study, performed between September 20 and October 7, 2016.
Inclusion criteria were treatment with LTOT during the study period and signed informed consent agreeing to participate. The only exclusion criterion was refusal to participate in the study, and therefore, refusal to sign the informed consent form.
Methods of Evaluating Therapeutic ComplianceBoth direct and indirect methods were used. The direct methods were readings taken from the counter clock on the supply source by Air Liquide technicians, and CO in exhaled air, determined using a Bedfont Micro Smokerlyzer®, with a CO range of 0–500ppm. Both determinations were performed in the patient's home. The indirect method was a questionnaire (Fig. 1) with simple, unambiguous questions about both compliance and tobacco consumption, and first-hand observation of signs of smoking (cigarettes, ashtrays, cigarette butts, etc.).
Statistical StudyAll the results collected in each patient's data collection sheet (Fig. 1) were entered in an Excel worksheet, and then processed using the statistical program SPSS 23.
First, the frequencies of the qualitative variables and basic statistics of the quantitative variables were analyzed. To verify the possible relationship between quantitative variables, a comparison of means was made using the Student t-test (assuming normal distribution of the samples), and the Mann–Whitney test (non-parametric). The analysis was based on whether the patient complied or did not comply with their treatment.
For the analysis of the possible relationships between qualitative variables, we used contingency tables and the Chi-square test. A correlation analysis was performed to check for any relationship between the different quantitative variables.
ResultsThe high level of acceptance of the study on the part of the patients is of note, since only 5 (0.5%) refused to participate. Of the sample studied, 49.1% were men and 50.4% women. Mean age was 82±10.2 years, with a range of between 35 and 104. In total, 46.5% lived in rural areas and 53.5% in an urban environment; 90.9% of the patients lived with others and 8.5% lived alone. Mean time since starting oxygen therapy was 3.3 years.
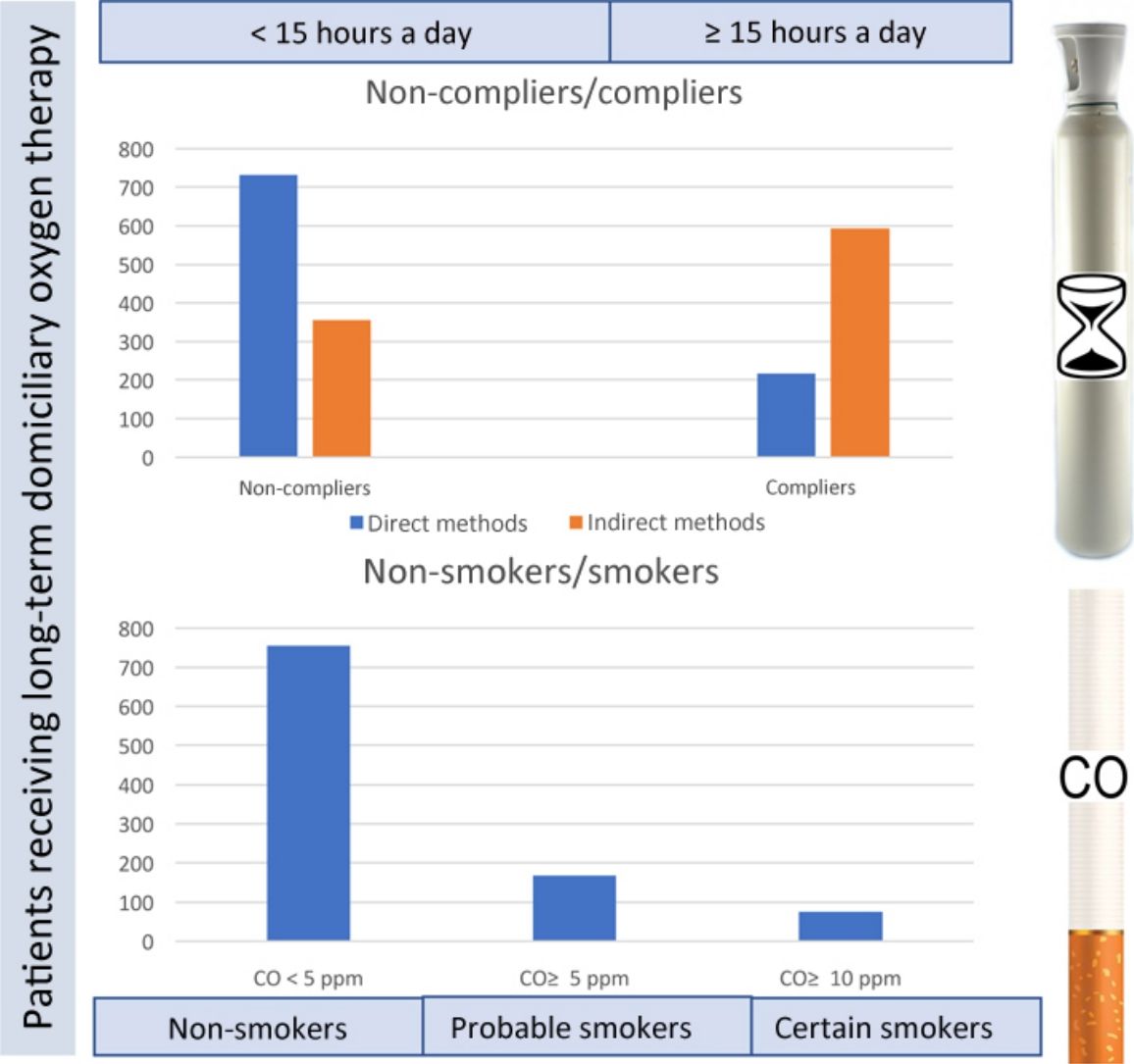
Analysis of Therapeutic ComplianceThe degree of compliance was assessed using the self-administered questionnaire and from the supply source clock counter readings; compliers were patients who had received treatment for 15 or more hours per day. Results are shown in Table 1.
If the clock counter reading is considered the best way to verify compliance, it should be noted that only 37.2% of the entire sample were compliers, while 62.3% were non-compliers. The number of non-compliers detected by direct methods was significantly higher, suggesting that only 48.4% of those considered compliers are truthful.
To create a profile of the compliant patient, we studied the possible relationships between the remaining variables and real compliers, understood as patients whose equipment counter data showed adherence to LTOT for at least 15h a day (355 patients). With regard to personal variables, no correlation was found between compliance and sex, age, urban or rural environment, or living alone or accompanied. Other variables studied were those associated with treatment characteristics (length of time since initiating treatment and supply system). Both are independent variables and do not influence compliance.
Analysis of Smoking HabitsSmoking in patients receiving LTOT is contraindicated and may be considered a factor of non-compliance per se. Indirect methods (questionnaire and the presence of signs of smoking in the patient's home) and direct methods (determination of CO in exhaled air) were used to assess the number of smokers.
A total of 459 patients (48.4%) stated in response to the smoking questionnaire that they were smokers or former smokers, and of these, 27 (5.8%) stated they continued to smoke, with an average consumption of 11±8.6cigarettes/day. Four admitted smoking even while receiving oxygen. Based on the first-hand observations made by supply company staff, signs of smoking were detected in the home of 37 patients (8%) of this same group, but not in the remaining 92%. Indications of smoking were found in the homes of all the declared current smokers (ashtrays and cigarette butts); while it obviously cannot be ascertained whether they belonged to the patient or to family members, it seems unlikely that the latter would smoke in front of a patient receiving LTOT. These differences were statistically significant (P<.001). The probability of finding no evidence and the patient being a non-smoker is 122 times greater.
We used the data obtained by indirect methods to study the possible correlations between smoking and patient-dependent factors. The average age of the group of smokers was 67.1±1.5 years versus 83.1±9.6 in the non-smokers group (P<.001). A statistically significant correlation (P=.009) with sex was also found: 74% of smokers were men and 25% women, and the probability of being (or having been) a smoker is 2.9 times greater among men. With regard to place of residence, 70.4% of smokers live in urban areas and 29.6% live in rural areas; while the proportion of smokers is greater in the urban environment, the difference is not statistically significant (P=.077).
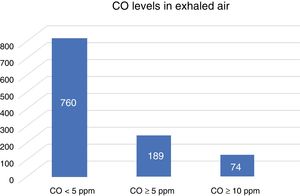
Co-oximetry was performed in all study patients, smokers and non-smokers alike, as a direct method of determining tobacco use. Mean values are shown in Table 2. The concentration of CO in exhaled air ranged between 0 and 40ppm. This wide variation may be explained by the fact that the overall study population includes non-smokers, former smokers, and current smokers. Obviously, we found a direct correlation between self-declared current smokers and those in whom signs of consumption and CO in exhaled air were detected (P<.001).
An analysis was made of patients, whether self-declared smokers or not, who had CO levels ≥5ppm, who could be considered likely smokers, and patients with CO ≥10ppm, who are considered smokers. The frequencies are shown in Table 3 and in the graph in Fig. 2. None of the patients who claimed to be never smokers had levels of CO ≥5ppm.
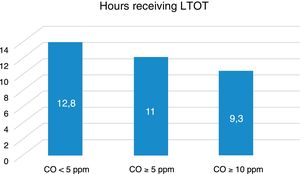
We also studied possible correlations between CO and patient-dependent factors, but only found a correlation between CO data and the age of the patients (P=.009). Testing the possible correlations between CO values and factors dependent on the characteristics of the oxygen treatment revealed significant correlations only between CO and the hours of use of oxygen therapy. Patients with CO <5ppm received treatment for an average of 12.8h/day; those with CO ≥5ppm received 11h a day (P<.001); and those with CO ≥10ppm received 9.3h a day (P<.001), as can be seen in Fig. 3.
DiscussionLack of therapeutic compliance is a widespread phenomenon which affects all types of patients, diseases and treatments, and is the main cause of treatment failure. The multiple factors that determine whether a patient complies or not with treatment are classified as patient-, disease-, and treatment-related factors, and socioeconomic and health system factors.10 Most of these converge in chronic respiratory diseases, which account for the largest group of patients receiving LTOT and those with the greatest degree of non-compliance. COPD,11 after depression, is the disease with the lowest levels of compliance.10
Concern about the problem of compliance in COPD is nothing new. The literature reports highly diverse rates of non-compliance, ranging from 4.2% in the study published in 1978 by Jones et al.12 to 80% in the Antadir study.13 Non-compliance figures have also been published in Spain, ranging from 10% in a study reported by Escarrabil et al.14 in 1985 to 51% reported by Solé et al.5 in 1992. In 2000, Cienfuegos et al.6 reported a rate of non-compliance of 60.5%.
These differences are possibly due to the fact that each study used very different methods to measure compliance, which undoubtedly influences the results. In our study, the rate of non-compliance was 26% when only the survey method was used, but when a direct method was used, the rate was 62.13%, similar to the figures published by Cienfuegos et al.6 This confirms that it is essential to use direct methods to obtain reliable information, since patients are not always truthful about their habits. It is also important that these studies are conducted in patients’ homes, based on surprise visits to avoid false responses. Patients trust the employees of the supplier companies who visit their homes on a regular basis, making them exceptional allies in the conduct of these studies. One study conducted in homes in a health area of Spain in 19918 found a 32.2% rate of compliance, while another multicenter study15 found much higher percentages (79%). Once again, the differences are attributable to the methodology used. In our study, applying the treatment for less than 15h a day was considered non-compliance, as recommended by the different guidelines.
Active smoking is a contraindication for the prescription of LTOT, and can be considered a factor of therapeutic non-compliance, according to the criteria established by the responsible health administrations. In real clinical practice, however, clinicians usually only advise patients against smoking during LTOT, or warn that smoking could lead to suspension of LTOT, a measure that is rarely imposed. However, the proportion of active smokers among these patients is high. In 2000, Cienfuegos et al.6 reported a prevalence in Spain of 11%. In another article published in 2010, Jiménez-Ruiz et al.7 reported a rate of 5.7%.
Given the supposition that smokers receiving oxygen therapy would, in principle, smoke very little, and in order to increase the sensitivity, we decided to establish 2 cut-off points: one at ≥10ppm, which corresponds to certain smokers, and another at ≥5ppm, corresponding to likely smokers. An overall analysis of co-oximetry values shows that 19.9% of the patients have values ≥5ppm, but if the cut-off is set at ≥10ppm, the percentage falls to 7.8% of the total sample.
The truly remarkable finding is that within the sample of current or former smokers, 167 patients who claimed to be former smokers had values ≥5ppm. At this cut-off point, there is a direct correlation between CO values and smoking (P<.001). The likelihood of having values of less than 5ppm is 19.8 times greater in non-smokers. When the cut-off point was set at ≥10ppm in the group who claimed not to smoke, 57 patients had values ≥10ppm, corresponding to certain smokers. At this cut-off point, there is a direct correlation between CO values and smoking (P<.001). The likelihood of having values <10ppm is 25.7 times greater in non-smokers.
A final factor we examined is whether the group of smokers are poorer treatment compliers (in terms of the number of hours a day receiving LTOT). We found that patients with higher values of CO were worse treatment compliers, when both CO >5ppm and CO >10ppm cut-off points were used. This allowed us to conclude that, in addition to their smoking habit, smokers used LTOT fewer hours per day, constituting 2 reasons for treatment failure.
The real benefits of home oxygen, in terms of quality of life and survival according to the degree of respiratory failure,15 remain controversial. However, the fact that many patients receiving LTOT continue to smoke should compel clinicians to step up efforts to help patients quit, and to monitor compliance with LTOT recommendations,16 particularly as patients who continue to smoke receive fewer hours of oxygen per day.
FundingThis study has been carried out without external funding, with the collaboration of the company Air Liquide in collecting field data.
Conflict of InterestsThe authors declare that they have no conflict of interests with Air Liquide or with the contents of this manuscript.
Please cite this article as: Barrueco-Otero E, Bartol Sánchez M, Pérez Rodríguez J, González Ruiz JM, Barrueco Ferrero M. Cumplimiento de la oxigenoterapia crónica domiciliaria. Influencia del consumo de tabaco. Arch Bronconeumol. 2019;55:368–372.