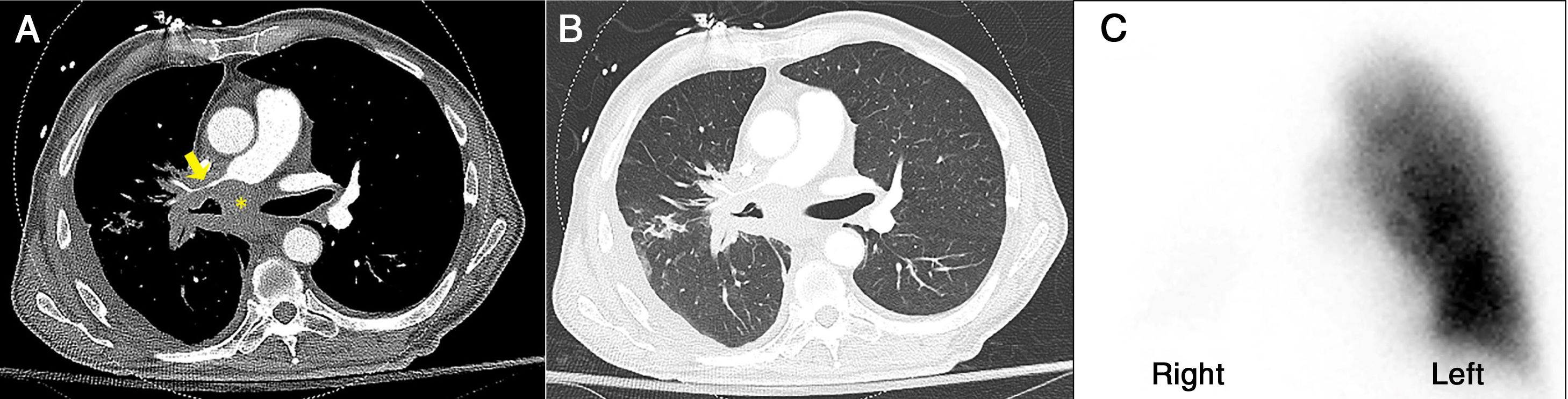
A middle-aged man with metastatic lung cancer and chronic obstructive pulmonary disease (COPD) presented with increasing dyspnea, wheezing, and cough for two weeks. On examination, he had irregularly irregular tachycardia, bilateral end-expiratory wheezes, and no peripheral edema. EKG revealed atrial fibrillation with rapid ventricular response. CT of the chest revealed no pulmonary embolism, a centrally obstructing right infrahilar soft tissue mass with narrowing of the right bronchus intermedius (Figs. 1A and B). Echocardiogram confirmed normal biventricular systolic function without pulmonary hypertension. Pulmonary was consulted for tracheobronchial intervention, but quantitative ventilation/perfusion study revealed minimal perfusion in the right lung (Figs. 1C). Following conservative medical therapy with amiodarone, inhaled bronchodilators and steroids for COPD exacerbation, patient gradually improved. Chemotherapy (carboplatin, pemetrexed) was continued. The patient expired 7 months later due to progressive disease.
Axial contrast-enhanced chest CT with mediastinal (A) and lung (B) windows shows conglomerate tumor (yellow asterisk) in the right hilar and subcarinal space with narrowing of the right bronchus intermedius and right distal main (yellow arrow) pulmonary artery. Quantitative lung perfusion scintigraphy (C) revealed nearly absent perfusion of right lung.
Quantitative lung scanning is a non-invasive procedure that provides prognostic information for postoperative pulmonary function.1 Unilateral absence of perfusion on ventilation/perfusion scan is rare, and literature is limited to case reports and small case series. Acquired conditions may include malignant fibrous histiocytoma, pulmonary artery tumors, bronchogenic carcinoma, pulmonary vein stenosis and massive pulmonary embolism.2 Bronchoscopic intervention is typically a palliative procedure in advanced lung cancer, and although it may have been technically feasible, compression of pulmonary vasculature and resolution of his acute symptoms would not support tracheobronchial intervention.
FundingThis research is supported in part by the National Institutes of Health through MD Anderson's Cancer Center Support Grant (CA016672).
Conflicts of InterestThe authors declare that no conflicts of interest exist.