A 5-year-old boy was admitted to the emergency department for hyperthermia, weight loss, and gingivorrhagia.
Initial clinical examination revealed hyperthermia (39.3°C), normal blood oxygen saturation, pallor, and splenomegaly.
Laboratory tests showed bicytopenia, with decreased hemoglobin at 8.6g/dl (standards 11–14g/dl), platelets at 141G/L (190–560/L), and mild inflammatory syndrome with CRP at 53mg/L (<5mg/L).
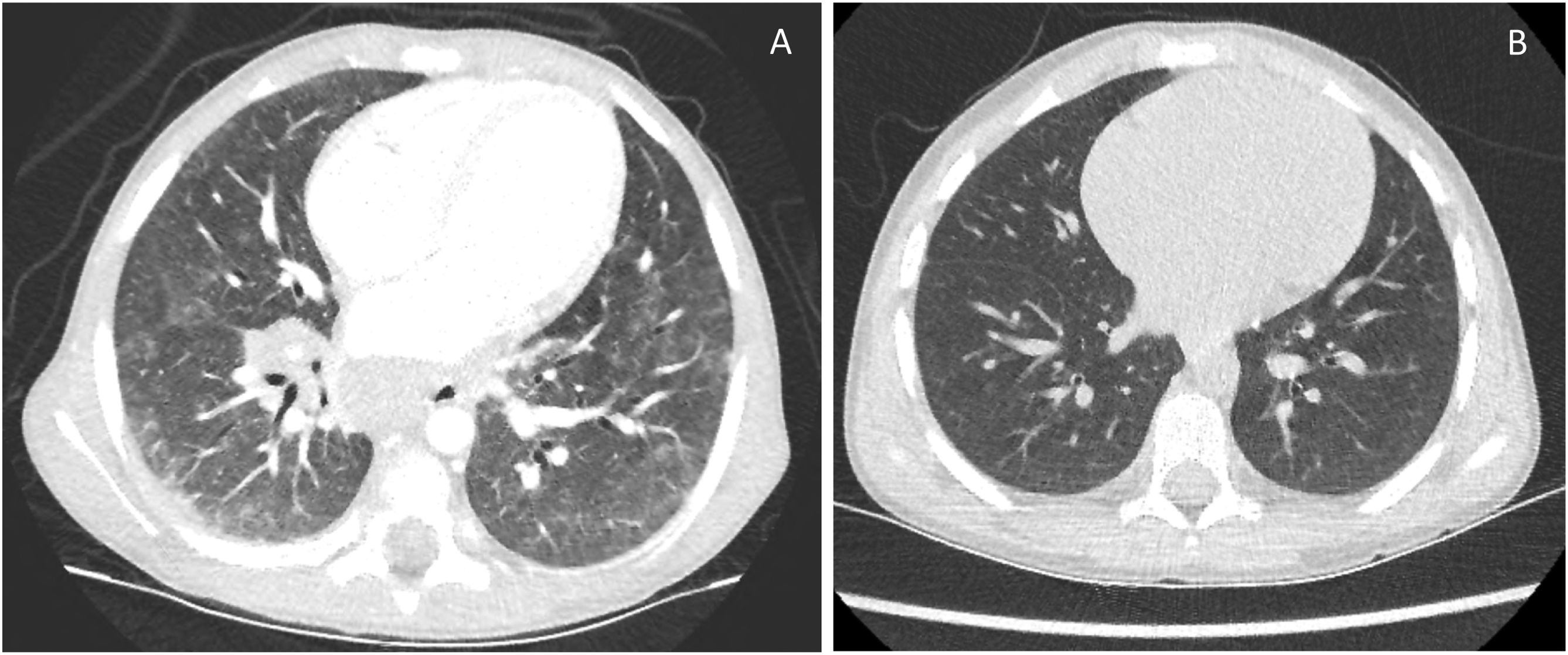
Further investigations were conducted with a thoracic and abdominal computed tomography scan which showed multiple cervical, mediastinal, hilar, and retroperitoneal adenomegalies, and a ground-glass aspect of both lung parenchyma (Fig. 1A).
The infectious investigations were negative, a myelogram was normal, whereas, the level of angiotensin-converting enzyme (ECA) was high.
Pathological examination of the cervical adenopathy, salivary gland biopsies, and bronchial biopsy showed granulomatous adenitis without necrosis. Bronchoalveolar lavage (BAL) revealed an inversion of the CD4/CD8 ratio.
The association of these clinical, anatomopathological, and biological abnormalities were consistent with sarcoidosis.
After excluding tuberculosis and lymphoma, oral corticosteroids were introduced at high doses, 1.5mg/kg for 1 month and then follow-up by progressive decrease.
Clinical, biological, and imaging plans (Fig. 1B) showed favorable outcomes immediately after treatment by steroids. Ten months after first clinical manifestations and after 9 months of corticosteroid treatment, the patient had no more manifestations of his disease.
The literature suggests that the clinical presentation of sarcoidosis varies depending on the age of children.1 For children less than 4 years of age, a triad of rash, uveitis, and arthritis is usually present, also named Blau syndrome. For older children, a multisystemic disease which is more similar to the adult presentation of the disease is present.2 In most frequent forms, pediatric sarcoidosis affects the lungs, the lymphatic system, and the liver, but other organs can be affected. In adults and children, the differential diagnosis had to be considered following the clinical presentation, especially infectious diseases, caused by mycobacteria or fungi, or neoplastic diseases such as lymphoma. The early onset form in children could lead to misdiagnosed juvenile rheumatoid arthritis.3 In front of a clinical general state alteration of a child with multiple adenopathies discovered by paraclinical examination, two main etiologies are lymphoma and tuberculosis. Although rare in children, sarcoidosis should be considered after elimination of both the most frequent diagnoses in this context. Treatment is quickly effective in a major part of cases and clinical evolution is most often favorable.
Conflict of interestNone.