Mechanical ventilation is the most extensively employed life support intervention among patients with severe respiratory failure of different etiologies. In this context, consistent delivery of the most suitable tidal volume (VT) to the patient is critical to achieving personalized mechanical ventilation. Indeed, in addition to its contribution to minute volume for optimization of blood gas exchange, appropriate VT strategies are critical to avoid ventilator-induced lung injury in the general context of lung-protective ventilation1 and when specifically applying ultra-low tidal volume ventilation.2 Additionally, VT is required to compute respiratory system compliance or ventilatory ratio, useful indices in the classification of patient phenotype and estimation of prognosis.3,4
Whereas measuring the pressures characterizing mechanical ventilation (e.g., peak inspiratory or positive end-expiratory pressures) is direct and straightforward using pressure transducers, actual VT measurements are complex since several computations are required. First, correct calibration values are required for the flow measuring device (usually a pneumotachograph) according to the oxygen fraction being used. For instance, to avoid a 12.5% volume overestimation when changing ventilation from room air to oxygen, the ventilator should automatically correct for the change in pneumotachograph resistance caused by the changes in gas viscosity.5 Second, correction for the compressibility of the ventilator circuit is essential since a fraction of the inspiratory volume measured at the ventilator outlet is shunted by compression and thus not delivered to the patient. For a typical value of ventilator circuit compliance (2mL/cmH2O)6 and an inspiratory pressure of 25cmH2O, the volume of shunted air is 50mL (≈10% of the typical VT). Remarkably, changes in the circuit compliance (e.g. inadvertent modification of tubing or humidifier dimensions) must be taken into account for correction, otherwise, these may result in substantial VT errors. Third, correction of VT according to the gas physical conditions is also needed since the inspiratory volume primarily measured by the ventilator corresponds to the device temperature and humidity, which are different from those within the patient lung (37°C and 100% relative humidity). Indeed, there is a 12.3% increase in VT when comparing dry air at 20°C in a ventilator and the corresponding VT in the patient lung.7
Therefore, knowing the actual VT in the patient's lungs is contingent on the implementation of ventilator algorithms to compute the three aforementioned corrective steps, each potentially amounting to more than 10% variance in the actual vs. calculated VT. In many instances, the clinicians will be unaware of whether and how the ventilator algorithms operate because they are commonly proprietary and generally undisclosed, and their implementation and results may differ among manufacturers.8 In other situations, and regardless of the ventilator type being used, errors in measured VT occur even in a priori well-maintained devices9 and are particularly frequent in low- and middle-income countries (LMIC).10 Assessment of the actual VT values delivered by the ventilator can be carried out by commercially available systems specially designed for this purpose. However, such devices are based on measuring VT using a pneumotachograph and a built-in microprocessor. Therefore, they are relatively expensive and require periodic servicing/recalibration as indicated by their manufacturer's instructions, prompting their limited use in low-resource medical centers. Thus, having an inexpensive and straightforward procedure for verifying the VT delivered by the ventilator at the bedside would be very useful for regular checks and quality controls in both resource-rich and resource-poor ICUs. Moreover, such capability can be particularly helpful when alternative ventilators must be rapidly set up, such as during the critical months of the COVID-19 pandemic.
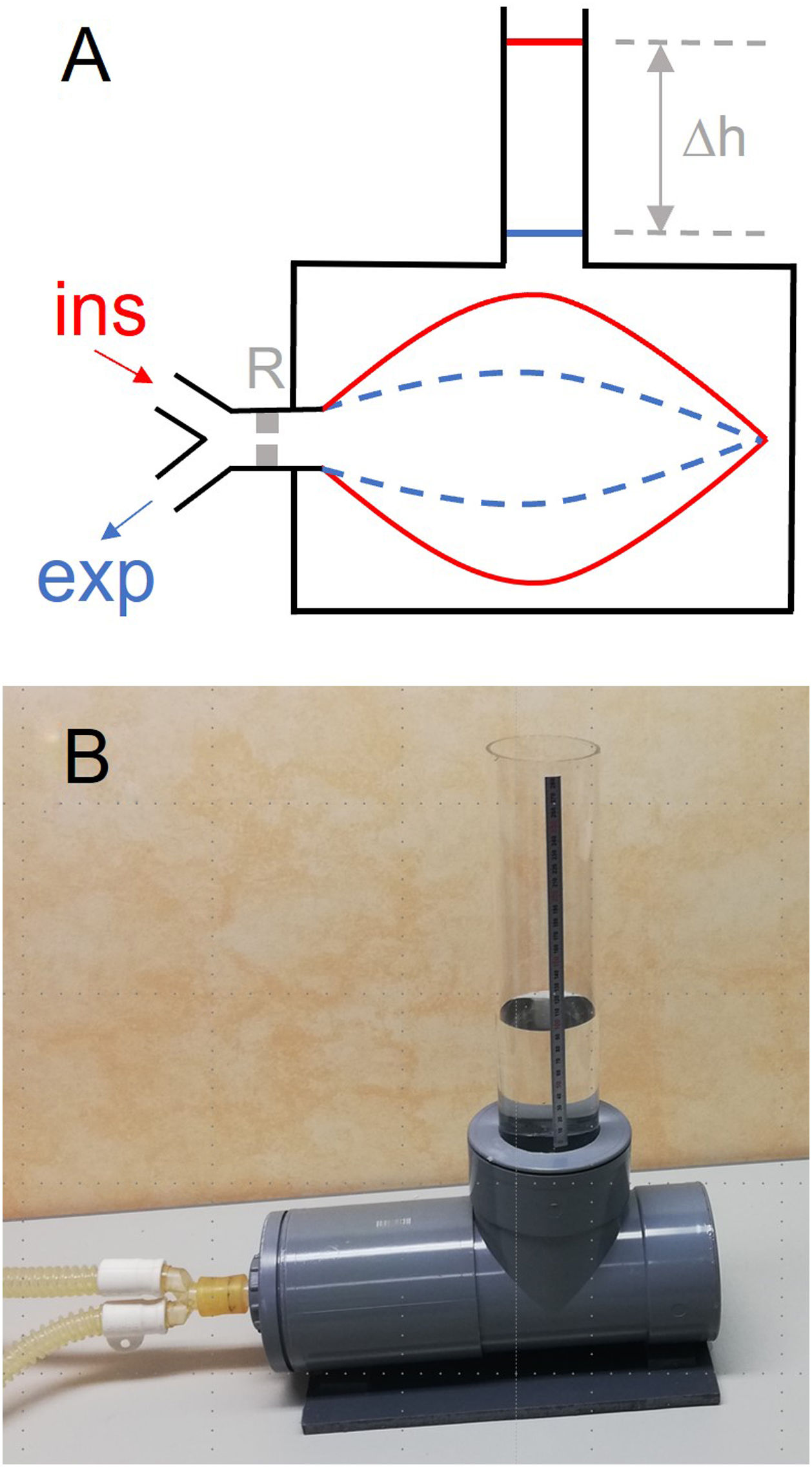
We herein describe an inexpensive and straightforward procedure that can be readily followed by clinical staff who are not experts in instrumentation techniques. Notably, the method does not require additional electronic sensors or complex devices. It directly measures the VT applied by the ventilator, thereby avoiding all the corrections and uncertainties associated with flow measurement and its attendant correction algorithms. As shown in Fig. 1A, a resistance and bag simulating a patient (test lung) is enclosed in a water-filled rigid-wall chamber. The VT applied by the test ventilator is measured from the difference in water levels (Δh) along the ventilator cycle, for instance during end-inspiration and end-expiration pauses. Indeed, VT=S·Δh, where S is the internal section of the vertical tube to measure h. The VT measured by water displacement is the VT applied by the ventilator to the simulated patient, measured at the conditions of the ventilator air, i.e., room temperature and humidity (0% for dry air from a compressed air supply or room humidity for turbine-based ventilators). This actual VT is the reference value to be compared with the VT measured by the ventilator.
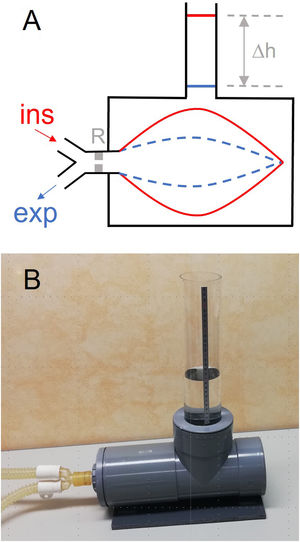
(A) Diagram of the method described for directly measuring the tidal volume (VT) delivered by a mechanical ventilator. A lung test, consisting of an orifice-type resistor (R) and a compliant bag enclosed in a water chamber open to the atmosphere through a vertical tube, is connected to the inspiratory and expiratory lines of the mechanical ventilator. The VT introduced into the bag induces an increase in the height (Δh) of water level in the tube, from end-expiration (blue) to end-inspiration (red). (B): Example of low-cost implementation of the measuring setting. The chamber was made with 15-cm diameter PVC drainpipe fittings. One of the cylinder bases was a screw cap to allow replacing the bag. The transparent vertical tube has an internal diameter of 7.4cm (section: 43.01cm2), hence VT (in mL)=43.01 x h (in cm).
As a practical example particularly interesting for potential users in LMIC, Fig. 1B shows a low-cost chamber implementation made using 15-cm diameter PVC tubing components that are widely available in hardware stores. In practical terms, the test lung (Fig. 1A) simply plays the role of an arbitrary patient impedance subjected to ventilation. As the method described herein is aimed at comparing the VT measured by the ventilator with its actual value measured by water displacement, the specific resistance and compliance of the simulated patient are not relevant provided they are within realistic boundaries, making it easy to choose among different options. For instance, we included a low-cost setting consisting of an orifice-type resistance (12.1cmH2Os/L at 0.3L/s; like in the Siemens-190 test lung) and a common 2-L anesthesia bag. Since the walls of this type of bag virtually do not exert elastic pressure for typical VT values (<2cmH2O up to 1.5L), the effective compliance of the simulated patient is very close to the compliance (C) corresponding to the increasing pressure (ΔP=ρ·g·Δh; ρ=1g/mL, and g=9.8m/s2) applied by water to the external wall of the bag as h increases during inspiration. Specifically, as ΔV=S·Δh, C=ΔV/ΔP=S/(ρ·g). In the setting of Fig. 1B, S=43.01cm2 and hence C=43.8mL/cmH2O, a figure within the range of respiratory compliance in adult patients.3 As it is readily apparent, the dimensions of the setting in Fig. 1B can be reduced if the aim is focused on assessing VT in pediatric ventilators. Interestingly, the precision in measuring volume emerges as being inversely proportional to section S of the vertical tube. Assuming the 1-mm resolution in the common ruler for assessing h in the setting in Fig. 1B, resolution in VT measurement is 4.3mL, which corresponds to 0.43% and 0.86% for maximum and typical VT values of 1000 and 500mL, respectively. Such precision is by far sufficient to detect any potential real-life errors when VT is measured by mechanical ventilators.8–10 The practical suitability and usefulness of the simple method proposed herein should be assessed in future studies evaluating mechanical ventilators by comparison with gold standard volume sensors.
In conclusion, we describe the concept and implementation of a simple and inexpensive method to measure the tidal volume delivered by a mechanical ventilator. As the procedure is straightforward and does not require complex equipment, clinical staff can perform such estimates in the ICU at the patient's bedside. The method can help verify the accuracy of VT in otherwise well-serviced settings and can be a realistic and easily implementable quality control procedure in LMIC regions where routine maintenance of medical devices is not necessarily widely available.