Calcific fibrous tumors are rare, benign tumors and can occur anywhere in the body. They were first diagnosed in 1988 by Rosenthal and Abdul-Karim.1 In 2002, the World Health Organization (WHO) classified these lesions as “calcific fibrous tumors” among bone and soft tissue lesions.2 Approximately 10% of calcific fibrous tumors have been identified in the pleura, and the name of the lesion was named “calcific tumor of the pleura” in 1996.3 Isomerism is a terminology meaning “mirror image” and describes the similarity of normally asymmetric left-right body parts. It is used synonymously with heterotaxy, but does not exactly correspond to each other in terminology. Heterotaxy or situs ambiguus is a disorder of the right-left distribution of the thoracic and abdominal organs that does not exactly correspond to the mirror image. Although the true incidence of heterotaxy is not known, some sources estimate it to be 1 in 8000–25,000 live births.4
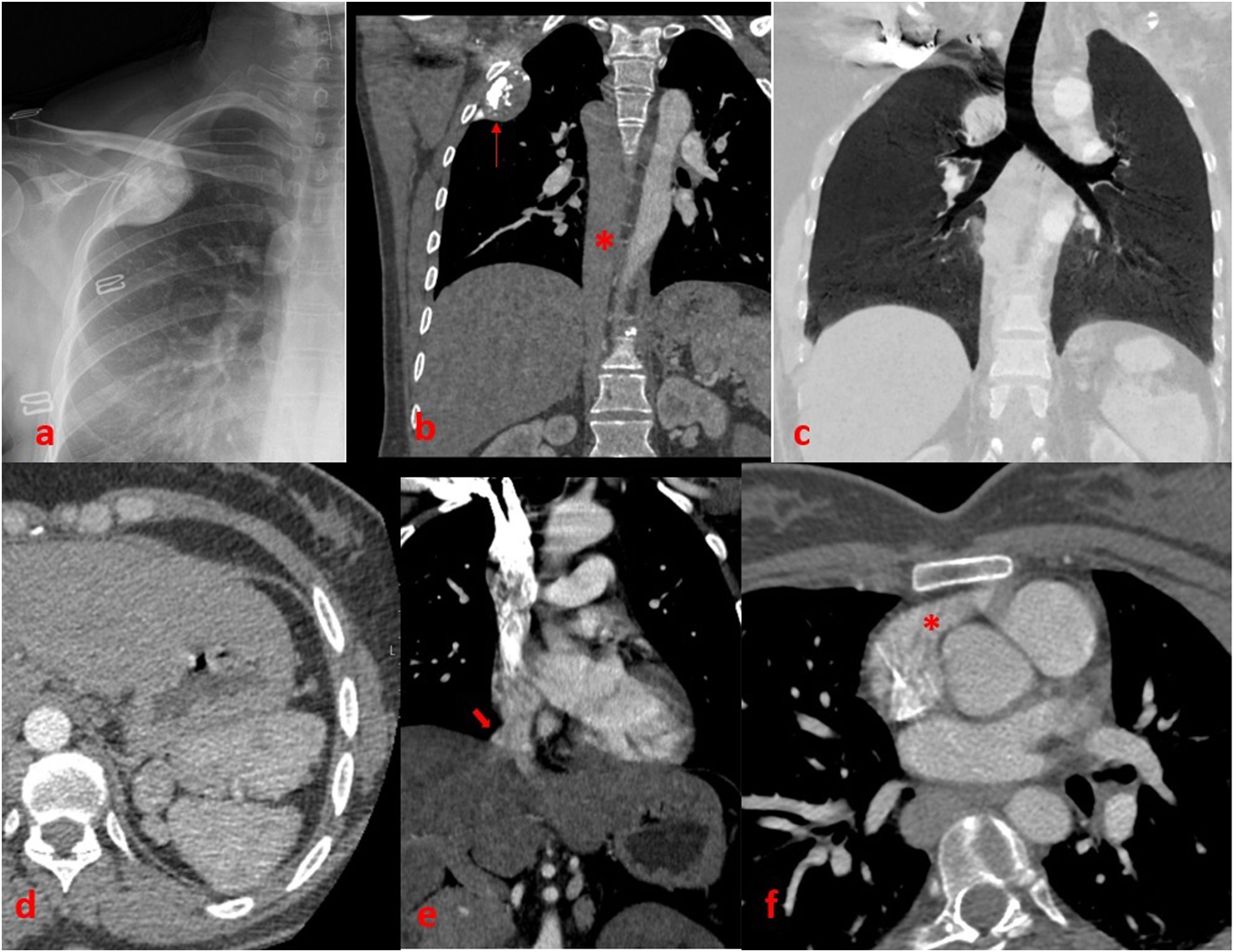
In the examination of the computed tomography (CT) images of a 40-year-old female patient with incidentally detected right apical mass in her chest X-ray; pleural-based calcified well-circumscribed lesion is observed adjacent to the upper lobe of the right lung. On CT, it is observed that the patient's azygos vein continues in the abdomen with the inferior vena cava. In addition, it is observed that the patient has 2 lung lobes in the right hemithorax and related 2 main bronchi branching from the trachea on both sides. In addition, the patient's hepatic veins open directly into the right atrium and multiple spleens compatible with polysplenia are observed in the patient. Annular pancreas is noticed in the abdominal sections of the patient. In addition, it is observed that the right atrial appendage has the morphology of the left atrial appendage (Fig. 1). Findings are consistent with left isomerism. Histopathologically confirmed that the lesion originating from the pleura was a calcific fibrous tumor of the pleura.
(a) Lung X-ray. A well-defined pleural-based calcified mass in the upper zone of the right lung. (b) Coronal CT section in mediastinal window. The mass is observed in soft tissue density with a calcified pleural base (red arrow). In addition, it is observed that the inferior vena cava continues in the thorax as the azygos vein (red asterisk). (c) Coronal MinIP image. Two hypoarterial main bronchi branching from the trachea are observed. (d) Polyplenism is observed in the left upper quadrant of the abdomen. (e) Opening of hepatic veins directly into the left atrium is observed. (f) Right atrial appendage is observed in left atrial appendage morphology (red asterisk).
Calcific fibrous tumors were included in the group of lung and pleural tumors by WHO in 2015. These lesions are often asymptomatic and often observed in the lower thoracic cavity. They rarely involve the apical pleura. In our case, apical pleural involvement is observed. It is difficult to make a differential diagnosis of these lesions with imaging findings. Left isomerism is a subtype of heterotaxy and is also known as polysplenia syndrome. In this syndrome, continuation of multiple spleen, azygos or hemiazygos veins with inferior vena cava, bilateral hypoarterial bronchus, bilateral bilobular lung, bilateral pulmonary/left atrium and intestinal malrotation are observed. In our case, the thoracic parts of these findings were observed.
Two rare entities were observed independently of each other in the same patient.
Authors’ contributionsAuthor contribution study design: Hüseyin Alper Kızıloğlu. Data collection: Hüseyin Alper Kızıloğlu. Literature research: Hüseyin Alper Kızıloğlu. Drafting manuscript: Hüseyin Alper Kızıloğlu.
Availability of data and materialsThe data are available from the author upon reasonable request.
Consent for publicationWritten informed consent was obtained from the patient for the publication of this case report and any accompanying images. The data presented in this case report do not allow identification of the patient.
FundingNo funding was obtained for this study.
Conflict of interestThe author declares that there is no conflict of interest.