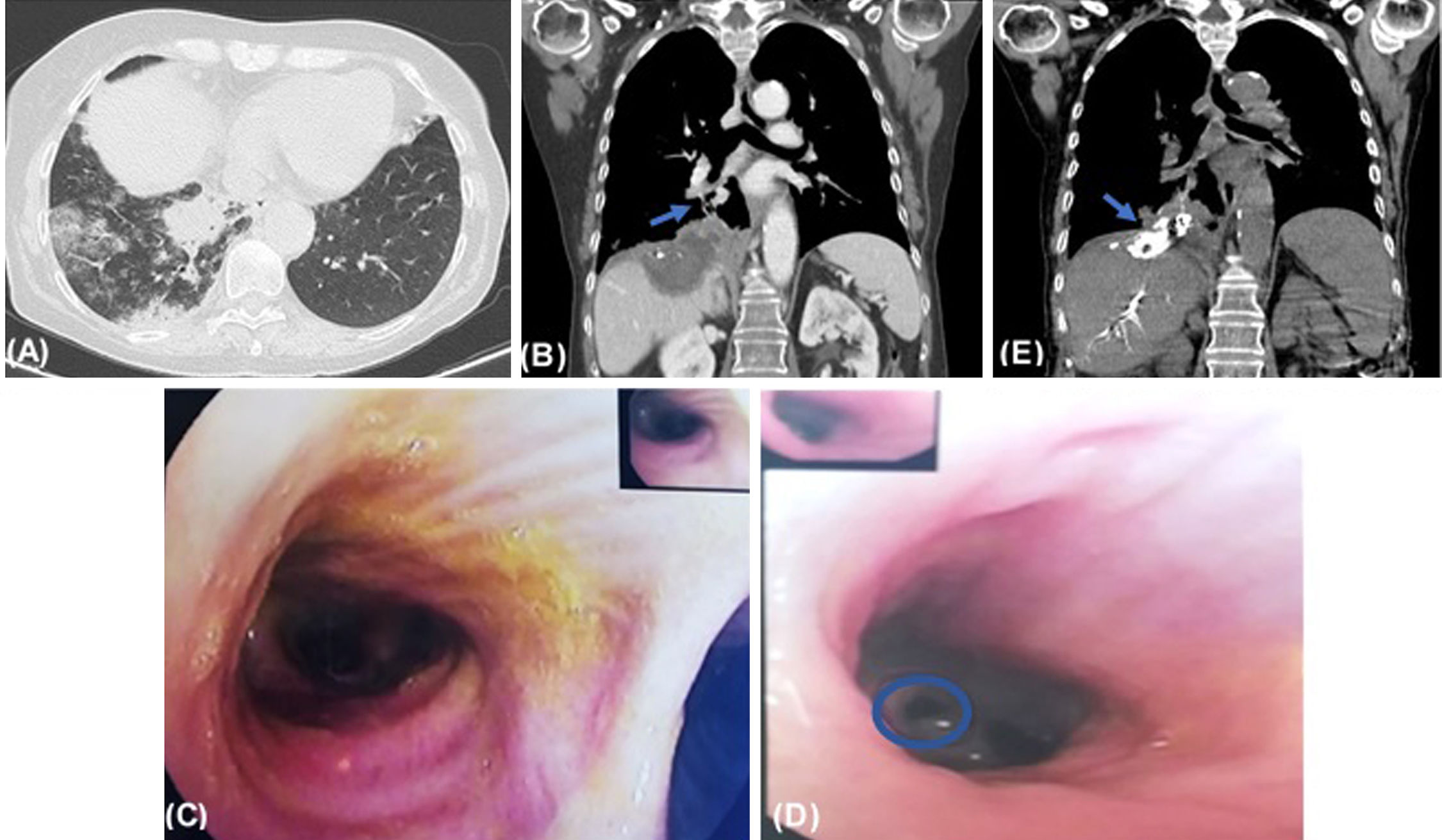
64-Year-old female presented at emergency department with several days-evolution of cough, yellowish sputum and fever. She had history of colon cancer with lung and hepatic metastases, submitted to multiple surgeries and chemotherapy. Thoracoabdominal-CT scan revealed a new right subphrenic collection contiguous with diaphragm, consistent with an abscess, and multiples focal hepatic lesions, one extending to right lung base, with multiple ground glass opacities (Fig. 1A and B). Therefore, the patient started antibiotic treatment and performed CT-guided percutaneous drainage of subphrenic collection, macroscopically compatible with bile. Bronchofibroscopy showed mucosa inflammation of medial basal segment of right lower lobe bronchus, from where yellowish secretions flowed (Fig. 1C and D), confirming biliobronchial fistula (BBF). Despite considering to close BBF through bronchofibroscopy, due to its peripheral location, embolization of fistulous track through percutaneous transhepatic cholangiography was performed, confirmed in post-procedure CT (Fig. 1E). The patient partially recovered and refused other treatments, being under palliative care.
(A) Axial thoracoabdominal-CT image shows ground glass opacities on right lower lobe. (B) Coronal thoracoabdominal-CT image shows new right subphrenic collection contiguous with diaphragm, consistent with an abscess; multiples focal hepatic lesions, one extending to right lung base, with a fistulous track (arrow). (C) Bronchofibroscopy revealed yellowish secretions in all bronchial tree. (D) Bronchofibroscopy revealed mucosa inflammation of medial basal segment of right lower lobe bronchus, from where yellowish secretions flowed, confirming fistulization site (circle). (E) Coronal CT image performed after embolization of the fistulous track shows the presence of high-attenuation embolization material (metallic coils and cyanoacrylate glue) in the right subphrenic space extending into the thorax (arrow).
BBF is a rare condition characterized by communication between biliary duct and bronchial tree, causing bilioptisis.1,2 It can be congenital or secondary to trauma, biliary duct obstruction or hepatic disease as tumor invasion. Recurrent pulmonary infections can occur.2 There are several treatment options, from conservative drainage to more invasive through bronchofibroscopy or cholangiography, with variable results.1,2