We read with great interest the well-written scientific letter by Hamada et al.,1 who reported the case of a 79-year-old man presenting a large lung abscess associated with a pulmonary artery pseudoaneurysm (PAP). He was treated by embolization of the pulmonary artery and showed complete resolution of the PAP and abscess in follow-up examinations. We would like to report the case of a 52-year-old man who presented to the emergency department with a 30-day history of fever, malaise, and weight loss. He also reported episodes of hemoptysis. A chest X-ray showed consolidation in the right upper lobe associated with cavitation and an air-fluid level. Contrast-enhanced chest computed tomography revealed extensive necrotic consolidation and a contrast-enhanced nodule inside the consolidation, related to a peripheral pulmonary artery (Fig. 1A and B), suggesting the diagnosis of PAP. The patient's sputum was negative for acid-fast bacilli. He was referred for fiberoptic bronchoscopy with bronchoalveolar lavage. Cultures were negative for tuberculosis, but positive for Klebsiella pneumoniae. Treatment with intravenous antibiotics (ceftriaxone) was implemented, and the patient responded to therapy.
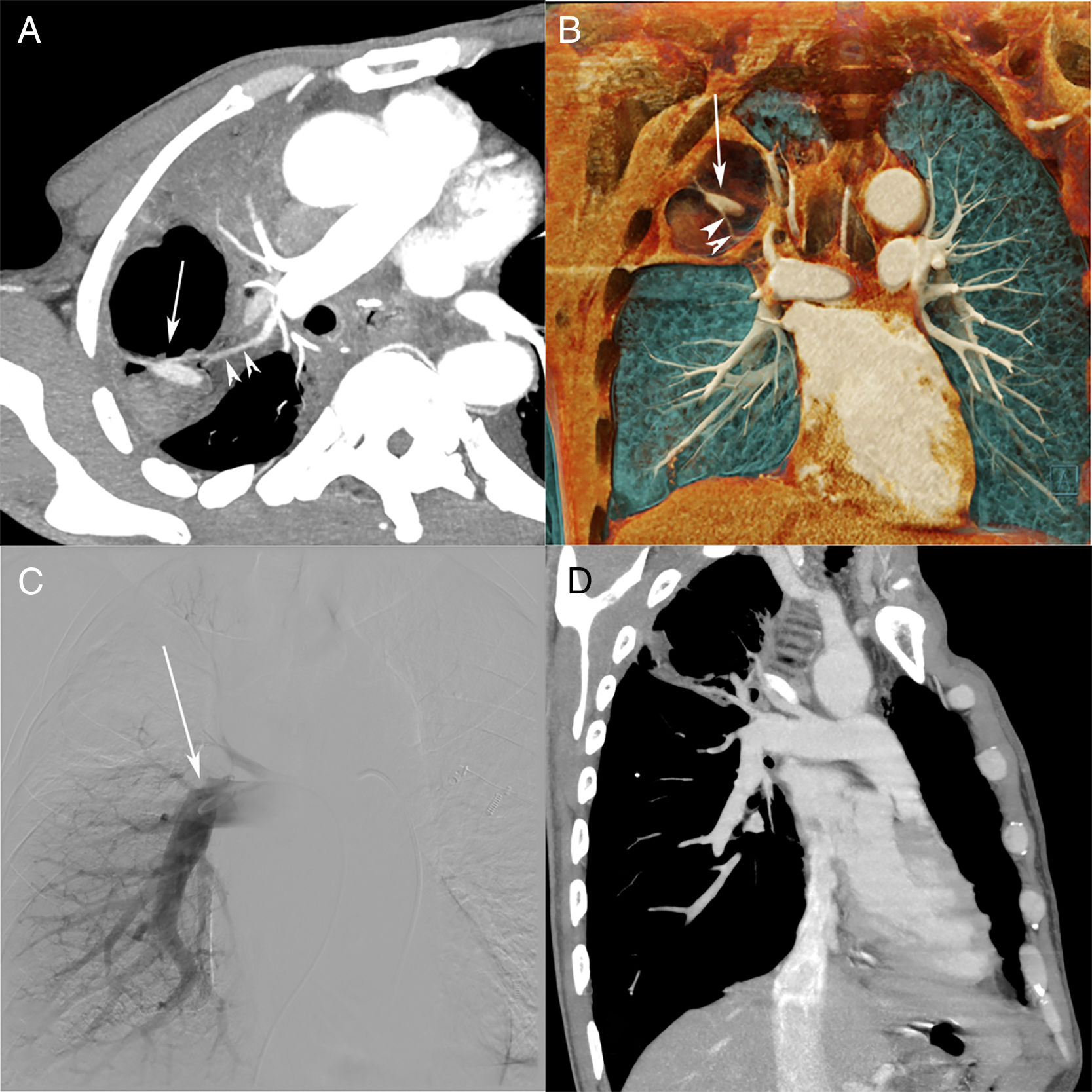
(A) Computed tomography (CT) pulmonary angiography (reconstruction with maximum intensity projection) showing a cavitated consolidation in the right upper lobe, with a highly enhancing nodule inside the cavity (arrow). Note also the relationship of the feeding vessel (arrowheads) to the pulmonary artery pseudoaneurysm (PAP; arrow). (B) Three-dimensional coronal reconstruction clearly depicts the PAP (arrow) and feeding vessel (arrowheads). (C) Pulmonary angiography performed 1 week after CT shows oligemia in the right upper lobe, with no opacification of the feeding vessel or PAP. A follow-up CT pulmonary angiography (D) demonstrated complete occlusion of the vessel and PAP, and partial resolution of the cavity.
However, a new expressive episode of hemoptysis led to a more aggressive approach, and a catheter angiogram with embolization was performed 1 week later. On angiography, the feeding vessel did not enhance (Fig. 1C), and selective catheterization was impossible. Bronchial and collateral angiography was also negative, suggesting thrombosis of the feeding vessel and PAP. The patient was discharged after computed tomography pulmonary angiography (CTPA) demonstrated complete occlusion of the vessel and PAP, and partial resolution of the cavity (Fig. 1D). The patient recovered uneventfully, with no evidence of bleeding during 1 year of follow-up.
PAP is a rare and potentially life-threatening condition, with mortality rates of up to 50%. About one-third of PAP cases have infectious causes. Other important causes are direct trauma and neoplasms. Commonly cited pathogenic organisms include pyogenic bacteria, Mycobacterium tuberculosis, and fungi. Although some authors have cited Klebsiella sp. as a causal agent of PAP, we found no paper presenting actual cases in which these bacteria caused PAP. Hemoptysis is the most common presenting symptom. Nevertheless, PAP is often underdiagnosed, even in hemoptysis settings, as most PAPs are small (about 1cm) and they may not be present in the acute phase of pulmonary abscess.1–5
CTPA with multiplanar reconstruction is the most important method for the diagnosis of PAP and its underlying cause. PAP can be identified as avidly enhancing nodules located in the walls of cavities or consolidations. Catheter angiography has been widely replaced by CTPA, being reserved for when intervention is planned. With catheter angiography, study of both the pulmonary and systemic circulations of the thorax is important.1–5 Hamada et al.1 commented that although most cases of PAP are treated with pulmonary artery embolization or surgical resection, spontaneous regression and resolution with antibiotic therapy have been documented in the literature. Our patient showed spontaneous resolution of the PAP after the clinical treatment of pneumonia. In conclusion, PAP should be included in the differential diagnosis of hemoptysis in patients with pulmonary infection.