Mucoepidermoid carcinoma of the lung (MEC) is a very rare tumor of low malignant potential. We present a case that occurred in a patient with bone marrow transplantation.
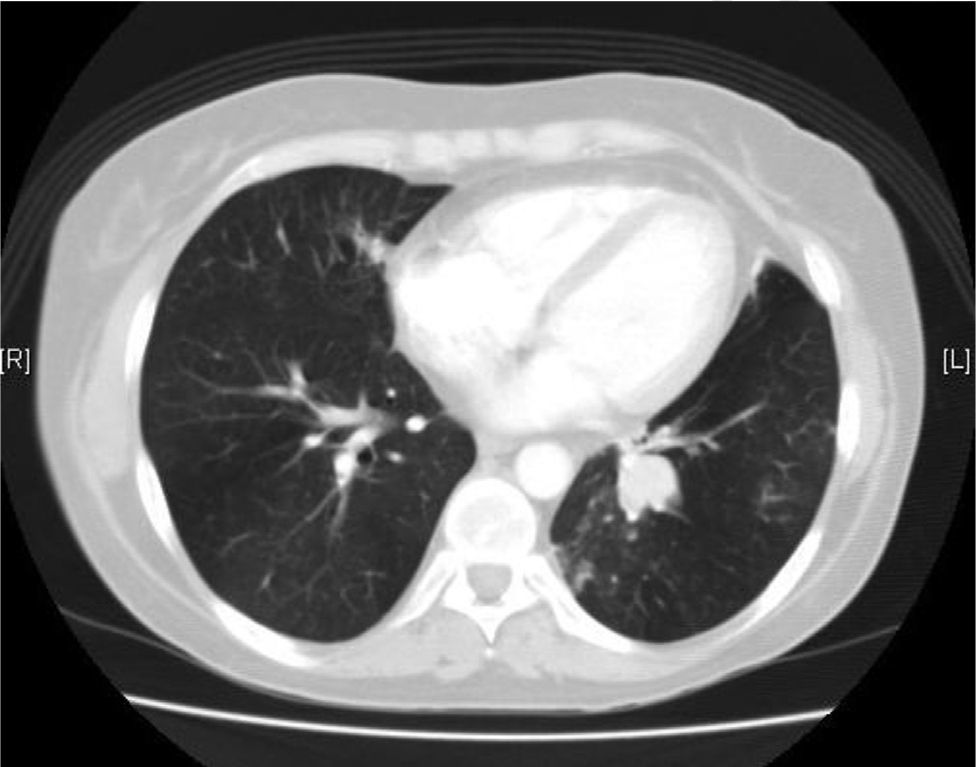
A 38-year-old female ex-smoker was diagnosed with acute leukemia and treated with chemotherapy, radiotherapy and subsequently received allogeneic bone marrow transplantation from an unrelated HLA-identical donor. After the procedure, she developed cutaneous and pulmonary graft-versus-host disease and repeated respiratory infections. She was admitted for hemoptysis of approximately 50cm,3 with no clinical symptoms of infection. She had very mild leukocytosis, mild hypoxemia and increased density in the left lower lobe. Chest CT scan revealed occupation of the segmental bronchi in the left lung base (Fig. 1). Bronchoscopy showed a highly vascularized endobronchial mass with whitish plaques. The biopsies did not reveal malignancy. After endobronchial laser resection, the biopsy was reported to be adenocarcinoma with mucinous areas, of pulmonary origin. Immunohistochemistry was positive for cytokeratin 7 (CK7) and carcinoembryonic antigen. Left lower lobectomy with mediastinal lymphadenectomy was performed by video-assisted thoracoscopy. A brown 3-cm endobronchial polypoid lesion with preserved bronchial epithelium lining was identified. There was involvement of the bronchial wall, but no extension beyond it. There was no infiltration into the lung parenchyma or vascular bundle. The growth pattern was glandular, with abundant mucoid material. No mitosis, nuclear pleomorphism, or necrosis were observed. Neoplastic cellularity was CK7-positive, while thyroid transcription factor-1 and chromogranin were negative, with isolated positivity for p63. The final diagnosis was low-grade endobronchial mucoepidermoid carcinoma, with a free surgical margin and hilar nodes with no neoplastic involvement. The patient continues to be followed up with regular visits, and no tumor recurrence has been detected to date.
MEC is an epithelial tumor with low malignant potential (5-year survival greater than 95%) composed of squamous, mucinous and intermediate cells. It usually originates in the salivary glands, but can be found in the lacrimal sac, sinonasal tract, larynx, thyroid and bronchi.1 MEC is rare (0.1–0.2% of all lung tumors) and over 50% of cases are detected in patients younger than 30 years.2 It is not related to tobacco smoking. Because of its typical endobronchial location, MEC may cause nonspecific symptoms of obstruction or infection. Peripheral lesions are usually infrequent and asymptomatic. Bronchoscopy is the most useful diagnostic test, although histological type may be difficult to establish. From a histological and immunohistochemistry point of view, MEC is similar to the neoplasm originating in the salivary glands.2 The degree of malignancy is based on the cellular activity and the presence of mitosis, and prognosis is determined by locoregional and distant invasion. MEC of high-grade malignancy usually occurs in older patients.3 The treatment of choice is surgery, and more conservative surgery may be performed in the case of lesions with low malignant potential when respiratory capacity is reduced.4 Adjuvant therapy is considered unnecessary, although some authors suggest radiotherapy and/or chemotherapy in the case of lymph node invasion or high-grade tumors.5 Follow-up is recommended due to the possibility of metastasis or relapse.1
Please cite this article as: Somiedo Gutiérrez MdV, Girón Moreno R, Moreno Balsalobre R. Tumor mucoepidermoide en paciente trasplantada de médula ósea. Arch Bronconeumol. 2014;50:125.