Both BODE score (body mass index, degree of airflow obstruction, functional dyspnea, and exercise capacity) and serum C-reactive protein (CRP) are validated predictors of mortality in patients with chronic obstructive pulmonary disease (COPD). The aim of this study is to investigate the predictive value of combined serum CRP and BODE score for mortality in COPD patients.
Patients and methodsA cohort of 114 clinically stable COPD patients was assessed for predictors of longitudinal mortality. Variables included age, gender, current smoking status, pack-years, maximal inspiratory/expiratory pressure, BODE score (body mass index, degree of airflow obstruction, functional dyspnea, and exercise capacity), serum CRP, and fibrinogen. Predictors were assessed by Cox proportional hazards regression model. Survival was estimated by Kaplan–Meier method and log-rank test.
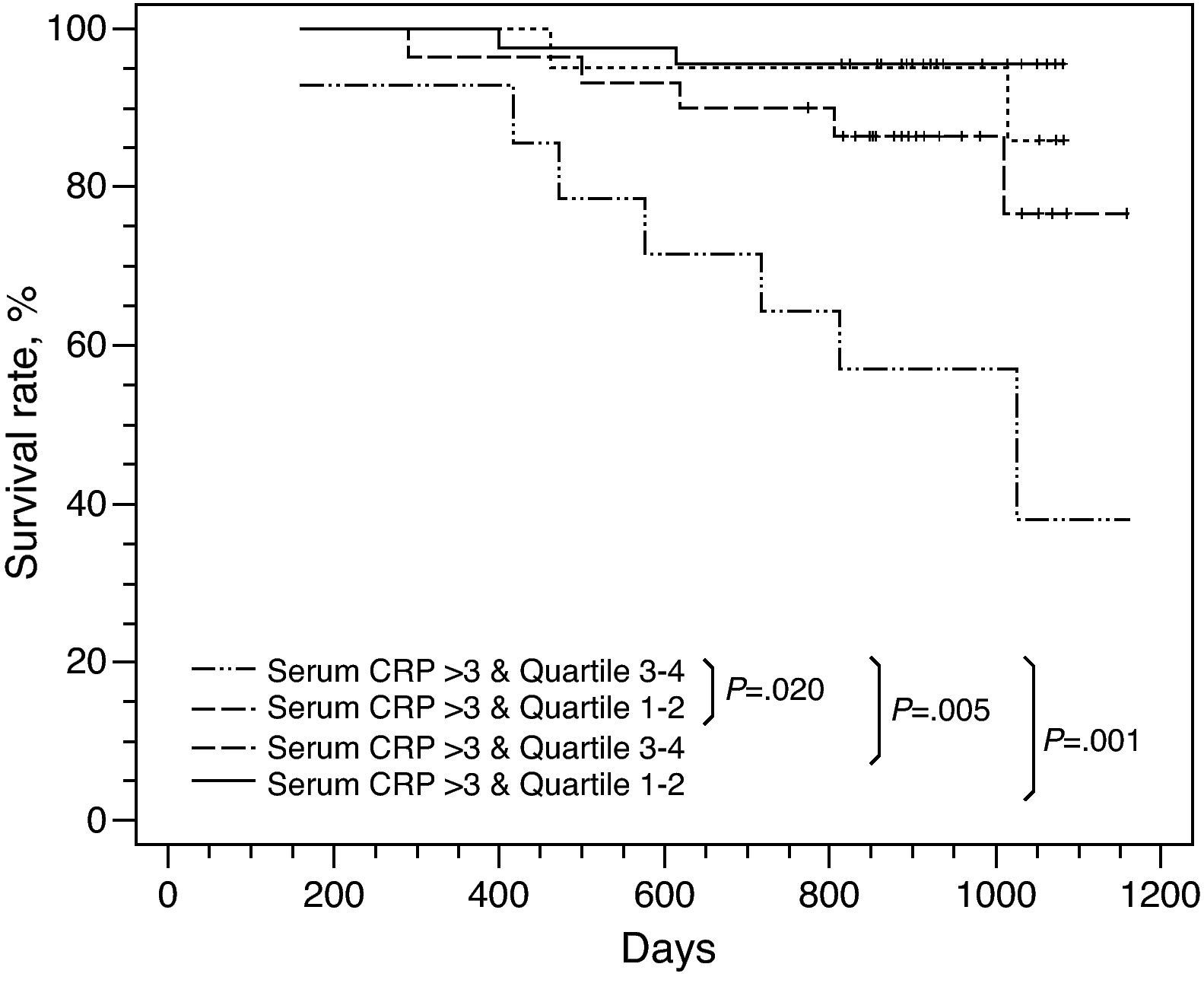
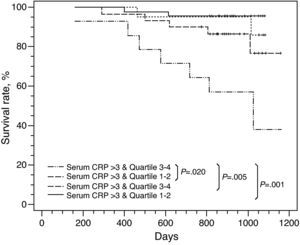
ResultsSerum CRP (P=.005; HR=1.042; 95% CI=1.019–1.066) and BODE score (P=.032; HR=1.333; 95% CI=1.025–1.734) were independent predictors of survival in the multivariate analysis. The cumulative survival rates of COPD patients were sorted from the worst to the best as following: serum CRP>3mg/l and quartile 3–4; serum CRP>3mg/l and quartile 1–2; serum CRP ≤3mg/l and quartile 3–4; serum CRP≤3mg/l and quartile 1–2 (P<.001).
ConclusionsSerum CRP and BODE score are independent predictors of survival in stable COPD patients. Combination of serum CRP and BODE score has higher predictive value in clinical practice.
Tanto la puntuación BODE (índice de masa corporal, grado de obstrucción del flujo aéreo, disnea funcional y capacidad de ejercicio) como la concentración sérica de proteína C reactiva (PCR) son variables pronósticas validadas de mortalidad en pacientes con enfermedad pulmonar obstructiva crónica (EPOC). El objetivo del presente estudio fue investigar el valor predictivo de la combinación de la concentración sérica de PCR y la puntuación BODE para la mortalidad en pacientes con EPOC.
Pacientes y métodosSe evaluó una cohorte de 114 pacientes con EPOC, clínicamente estables, en busca de las variables pronósticas de mortalidad longitudinal. Las variables incluyeron la edad, sexo, tabaquismo actual, paquetes-año, presión inspiratoria/espiratoria máxima, puntuación BODE (body mass index, degree of airflow obstruction, functional dyspnea, and exercise capacity), concentración sérica de PCR y fibrinógeno. Las variables pronósticas se evaluaron mediante un modelo de regresión de riesgos proporcionales de Cox. La supervivencia se estimó mediante el método de Kaplan–Meier y la prueba del log-rank.
ResultadosLa concentración sérica de PCR (P=0.005; CR=1.042; IC del 95%=1.019–1.066) y la puntuación BODE (P=0.032; CR=1.333; IC del 95%=1.025–1.734) fueron variables pronósticas independientes de la supervivencia en el análisis multivariante. Las tasas de supervivencia acumulativas de los pacientes con EPOC se clasificaron desde las peores hasta las mejores del modo siguiente: concentración sérica de PCR>3mg/l y cuartil 3–4; concentración sérica de PCR>3mg/l y cuartil 1–2; concentración sérica de PCR ≤3mg/l y cuartil 3–4; concentración sérica de PCR ≤3mg/l y cuartil 1–2 (P<0,001).
ConclusionesLa concentración sérica de PCR y la puntuación BODE son variables pronósticas independientes de la supervivencia en pacientes con EPOC estable. La combinación de la concentración sérica de PCR y la puntuación BODE posee el mayor valor predictivo en la práctica clínica.
Chronic obstructive pulmonary disease (COPD) is an inflammatory process characterized by progressive airflow limitation and the destruction of the parenchyma.1 This disease not only affects the lungs but may also produce substantial systemic effects.2 C-reactive protein (CRP) is an important systemic inflammation marker that reflects the total systemic inflammation load.3 It has been demonstrated that its concentration is high in patients with stable COPD4 and during exacerbations.5 It is also a prognostic variable for hospitalization and mortality in patients with chronic respiratory failure.6 An increase in its concentration can predict cardiovascular risk in patients with COPD.7 Two epidemiological studies8,9 have demonstrated that the increase in its concentration is independently associated with overall and cardiovascular mortality in patients with the disease and mild or moderate degrees of obstruction of the airways.
Celli et al.10 proposed the BODE index, a multidimensional parameter that includes body mass index (B), degree of airflow obstruction (O), functional dyspnea (D) and exercise capacity (E). It was reported to be better than forced expiratory volume in 1s (FEV1) to reflect the severity of COPD, and it is effective in the prediction of mortality in patients with the disease.10 In this population of patients, it has also been described that the BODE score is applicable for predicting an individual's need for hospitalization,11 determining the lung function changes of the follow-up during pulmonary rehabilitation12 and the transbronchoscopic application of one-way valves,13 predicting survival after lung volume reduction surgery14 and reflecting modifications of the disease.15
In clinical practice, it is foreseeable that the combination of the levels of serum CRP concentrations and the BODE score would be a better predictor for survival between patients with COPD, because serum CRP is an important systemic inflammatory marker and the BODE score is a clinical parameter of great use for patients with the disease. The objective of the present study was to determine the predictive value of CRP serum concentrations combined with the BODE score for mortality in patients with stable COPD.
Materials and MethodsStudy DesignWe carried out a prospective study to select clinically stable COPD patients and register their characteristics in order to identify the prognostic longitudinal mortality variables. The variables included age, sex, current tobacco use, pack-years, maximal inspiratory pressure, maximal expiratory pressure, severity of COPD, modified Medical Research Council dyspnea scale (MMRC), body mass index, diffusion capacity, 6-minute walk test (6MWT), serum CRP concentration, serum fibrinogen concentration and BODE score.
Study SubjectsThe study was approved by the Research Committee of the Chang Gung Memorial Hospital, which also provided financing. A total of 125 patients were consecutively selected with variable COPD severity from April 2005 to July 2006 from the Division of Pulmonary Medicine outpatient clinic, Chang Gung Memorial Hospital-Kaohsiung Medical Center, a hospital with 2300 primary-care beds and a tertiary reference center in Taiwan (China). These patients underwent spirometry and lung volume determinations in accordance with the recommendations published by the American Thoracic Society and according to standard references.16 Each recruited COPD patient was over the age of 40 and had been a heavy smoker, with smoking histories of at least 10 pack-years. The diagnosis of COPD was established based on anamnesis, physical exploration and the spirometric data of the patient indicative of a post-bronchodilator FEV1 (forced expiratory volume in 1s)/forced vital capacity (FVC) ratio of less than 0.7, with a reversibility by means of inhaled bronchodilator of FEV1<15%.1
In the selected patients, other causes of airway limitation were excluded, such as pulmonary tuberculosis, bronchial asthma, bronchiectasis and heart failure, identified by reviewing chest radiographies and medical files. We also excluded those patients with diagnosis of cardiovascular disease, such as coronary artery disease, peripheral vasculopathy or cerebral vascular disease. After 6 weeks of appropriate treatment, the patients with clinically stable COPD were included; for these patients, the BODE index was calculated and serum CRP concentrations determined. The patients who experienced an exacerbation in their COPD (fever, increase in purulent sputum or dyspnea) or hospitalizations for any reason during the 6-week treatment period were excluded from the study. After their inclusion, the patients were seen approximately every 3 months based on the medical histories and the computerized information. If a patient was lost to follow-up at our hospital, the research assistant communicated with the patient or his/her family and acquired information regarding mortality in a telephone interview. The final data of the study were collected on 7 August 2008. During the follow-up period, the mortality due to any cause was used as an analyzed variable.
CRP DeterminationFasting blood samples were obtained while the patients were at rest and before carrying out any other test. The CRP concentrations were determined with a high-sensitivity immunoanalysis. The analytical sensitivity of this analysis was 0.1mg/l, and the determination range was 0.1–20mg/l. We divided the COPD patients into two subgroups with an initial cut value for the CRP concentration >3mg/l or ≤3mg/l because, in studies published about cardiovascular medicine17,18 and in the COPD cohort described by Dahl et al.,9 it has been previously demonstrated that this value is a determinant for patient survival.
Evaluation With the BODE IndexEach patient was assigned a BODE score, which was calculated using an empirical model as has previously been described.10 The body mass index (BMI) was calculated as the weight of the patient in kilograms divided by height in meters squared.1 The degree of airflow obstruction was determined by means of FEV1,19 dyspnea was determined using the MMRC dyspnea scale20 and exercise capacity was determined with the distance walked in 6minutes (6MWT).21 For each value of FEV1, MMRC dyspnea scale and 6MWT, each patient received points that varied from 0 to 3; for the body mass index, each patient received 0 or 1 point.10 The points for each component of the BODE index were added, and the score varied between 0 and 10 points for each patient. In addition, the BODE score was classified in quartiles as previously described: quartile 1 included patients with a score of 0–2; quartile 2, 3–4 points; quartile 3, 5–6 points; and quartile 4, 7–10 points.10
Statistical AnalysesThe continuous variables are presented as means±standard deviation and the categorical variables are presented as absolute numbers and percentages. The relationship between the BODE quartile and the patients with a serum concentration of CRP >3mg/l and ≤3mg/l was analyzed by means of a non-parametric test. The difference in the BODE scores between patients with a serum CRP concentration >3mg/l and ≤3mg/l was evaluated using the Student's t-test. In order to identify the most significant prognostic factors for survival and calculate the hazard ratios (HR) for mortality and the 95% confidence intervals (CI), we used a Cox proportional hazards regression model. The variables whose P values were <.05 in the univariate analysis were also analyzed in a multivariate analysis. Survival was estimated by means of the Kaplan–Meier method with a log-rank test. A two-tailed P value<.05 was considered statistically significant. The statistical analyses were done using the SPSS program (version 13.0; SPSS Inc., Chicago, IL, United States).
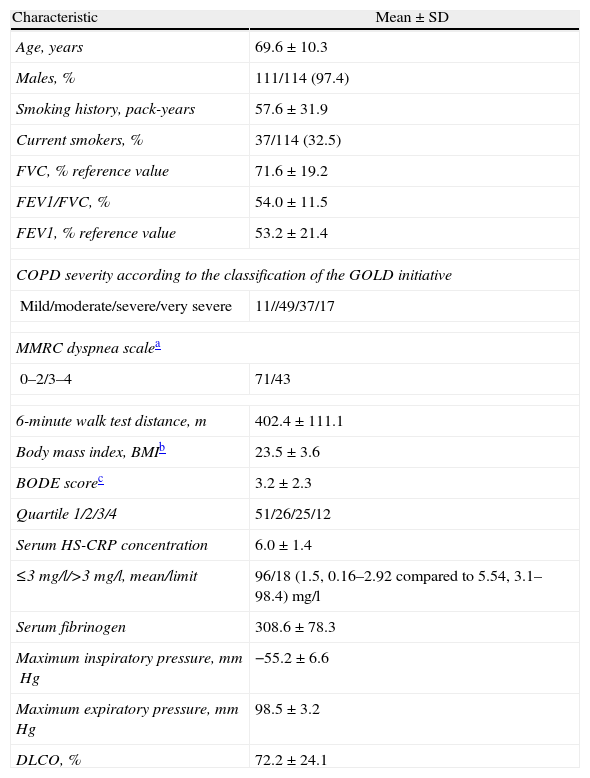
ResultsCharacteristics of the Study ParticipantsWe initially selected 125 patients for the present study. However, 6 of them were excluded due to the exacerbation of the symptoms or to hospitalization during the initial 6-week observational period. Out of the 119 cases included in the study, we could not obtain information about the mortality in 5 because they had either changed residence or telephone, or due to the lack of cooperation of the patient or his/her family. Therefore, in the final analysis we include a total of 114 patients. Table 1 shows the characteristics of the study participants.
Characteristics of the 114 Patients With Clinically Stable Chronic Obstructive Pulmonary Disease.
| Characteristic | Mean±SD |
| Age, years | 69.6±10.3 |
| Males, % | 111/114 (97.4) |
| Smoking history, pack-years | 57.6±31.9 |
| Current smokers, % | 37/114 (32.5) |
| FVC, % reference value | 71.6±19.2 |
| FEV1/FVC, % | 54.0±11.5 |
| FEV1, % reference value | 53.2±21.4 |
| COPD severity according to the classification of the GOLD initiative | |
| Mild/moderate/severe/very severe | 11//49/37/17 |
| MMRC dyspnea scalea | |
| 0–2/3–4 | 71/43 |
| 6-minute walk test distance, m | 402.4±111.1 |
| Body mass index, BMIb | 23.5±3.6 |
| BODE scorec | 3.2±2.3 |
| Quartile 1/2/3/4 | 51/26/25/12 |
| Serum HS-CRP concentration | 6.0±1.4 |
| ≤3mg/l/>3mg/l, mean/limit | 96/18 (1.5, 0.16–2.92 compared to 5.54, 3.1–98.4) mg/l |
| Serum fibrinogen | 308.6±78.3 |
| Maximum inspiratory pressure, mmHg | −55.2±6.6 |
| Maximum expiratory pressure, mmHg | 98.5±3.2 |
| DLCO, % | 72.2±24.1 |
FVC, forced vital capacity; FEV1, maximum expiratory volume in 1s; COPD, chronic obstructive pulmonary disease; BODE, body mass index, degree of airflow obstruction, functional dyspnea and exercise capacity; MMRC, modified Medical Research Council dyspnea scale; 6MWT, 6-minute walk test; DLCO, carbon monoxide diffusion capacity; HS-CRP, high-sensitivity C-reactive protein; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
There were no significant differences in the BODE scores between patients whose serum CRP concentrations were ≤3mg/l and those in whom it was >3mg/l (3.11 compared with 3.34; P=.62). The non-parametric analysis also did not demonstrate a correlation between the BODE quartile and the serum concentration of CRP (P=.87).
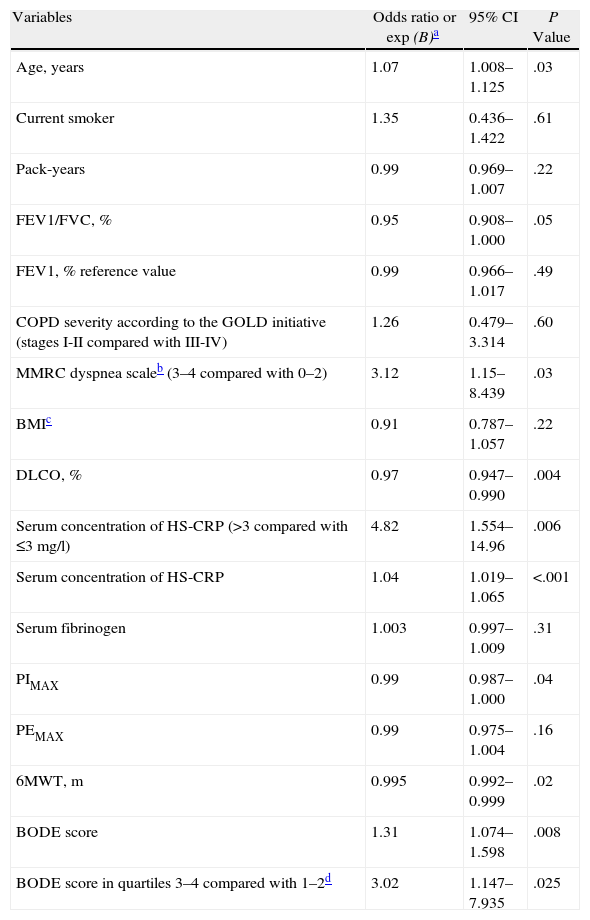
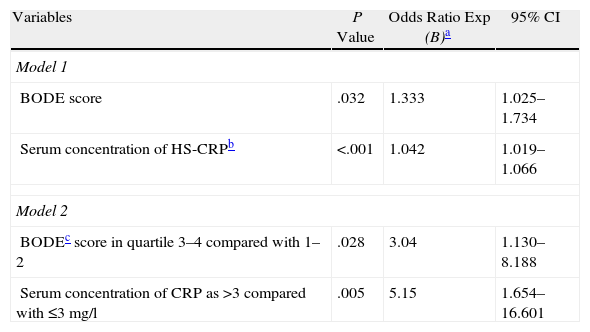
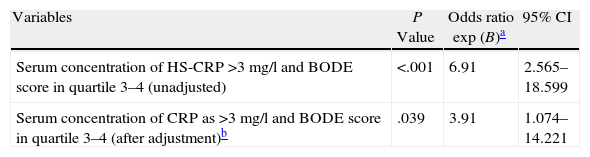
Predictive Variables for Survival in Patients With Chronic Obstructive Pulmonary DiseaseIn the univariate analysis, it was demonstrated that parameters such as age, FEV1/FVC, MMRC dyspnea scale, 6MWT, serum concentration of CRP, carbon monoxide diffusion capacity (DLCO), maximum inspiratory pressure (PIMAX) and BODE scores were significantly associated with mortality (Table 2). However, despite treating the serum concentration of CRP with either total data or divided by categories, or treating the BODE score as either a continuous variable or divided in quartile categories, the multivariate analysis demonstrated that the serum CRP concentration and the BODE scores were independent prognostic variables for mortality (Table 3). A serum CRP concentration >3 simultaneous with a BODE score in quartile 3–4 predicted a greater mortality than any of the two factors alone or in the absence of both in patients with clinically stable COPD (Table 4).
Univariate Analysis of the Prognostic Factors of Patients With Chronic Obstructive Pulmonary Disease.
| Variables | Odds ratio or exp (B)a | 95% CI | P Value |
| Age, years | 1.07 | 1.008–1.125 | .03 |
| Current smoker | 1.35 | 0.436–1.422 | .61 |
| Pack-years | 0.99 | 0.969–1.007 | .22 |
| FEV1/FVC, % | 0.95 | 0.908–1.000 | .05 |
| FEV1, % reference value | 0.99 | 0.966–1.017 | .49 |
| COPD severity according to the GOLD initiative (stages I-II compared with III-IV) | 1.26 | 0.479–3.314 | .60 |
| MMRC dyspnea scaleb (3–4 compared with 0–2) | 3.12 | 1.15–8.439 | .03 |
| BMIc | 0.91 | 0.787–1.057 | .22 |
| DLCO, % | 0.97 | 0.947–0.990 | .004 |
| Serum concentration of HS-CRP (>3 compared with ≤3mg/l) | 4.82 | 1.554–14.96 | .006 |
| Serum concentration of HS-CRP | 1.04 | 1.019–1.065 | <.001 |
| Serum fibrinogen | 1.003 | 0.997–1.009 | .31 |
| PIMAX | 0.99 | 0.987–1.000 | .04 |
| PEMAX | 0.99 | 0.975–1.004 | .16 |
| 6MWT, m | 0.995 | 0.992–0.999 | .02 |
| BODE score | 1.31 | 1.074–1.598 | .008 |
| BODE score in quartiles 3–4 compared with 1–2d | 3.02 | 1.147–7.935 | .025 |
FEV1, maximum expiratory volume in 1s; COPD, chronic obstructive pulmonary disease; BODE, body mass index, degree of airflow obstruction, functional dyspnea and exercise capacity; CI, confidence interval; MMRC, modified Medical Research Council dyspnea scale; 6MWT, 6-minute walk test; DLCO, carbon monoxide diffusion capacity; HS-CRP, high-sensitivity C-reactive protein; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
Multivariate Analysis of the Prognostic Factors of Patients With Stable Chronic Obstructive Pulmonary Disease.
| Variables | P Value | Odds Ratio Exp (B)a | 95% CI |
| Model 1 | |||
| BODE score | .032 | 1.333 | 1.025–1.734 |
| Serum concentration of HS-CRPb | <.001 | 1.042 | 1.019–1.066 |
| Model 2 | |||
| BODEc score in quartile 3–4 compared with 1–2 | .028 | 3.04 | 1.130–8.188 |
| Serum concentration of CRP as >3 compared with ≤3mg/l | .005 | 5.15 | 1.654–16.601 |
BODE, body mass index, degree of airflow obstruction, functional dyspnea and exercise capacity; HS-CRP, high-sensitivity C-reactive protein; CI, confidence interval
The BODE score was subdivided additionally into quartiles in the following manner, quartile 1, 0–2 points; quartile 2, 3–4 points; quartile 3, 5–6 points, and quartile 4, 7–10 points.2
Combination of a Serum Concentration of CRP>3 and a BODE Score in Quartile 3–4: Predictive Value for Mortality in Patients With Stable Chronic Obstructive Pulmonary Disease.
| Variables | P Value | Odds ratio exp (B)a | 95% CI |
| Serum concentration of HS-CRP >3mg/l and BODE score in quartile 3–4 (unadjusted) | <.001 | 6.91 | 2.565–18.599 |
| Serum concentration of CRP as >3mg/l and BODE score in quartile 3–4 (after adjustment)b | .039 | 3.91 | 1.074–14.221 |
BODE, body mass index, degree of airflow obstruction, functional dyspnea and exercise capacity; HS-CRP, high-sensitivity C-reactive protein; CI, confidence interval.
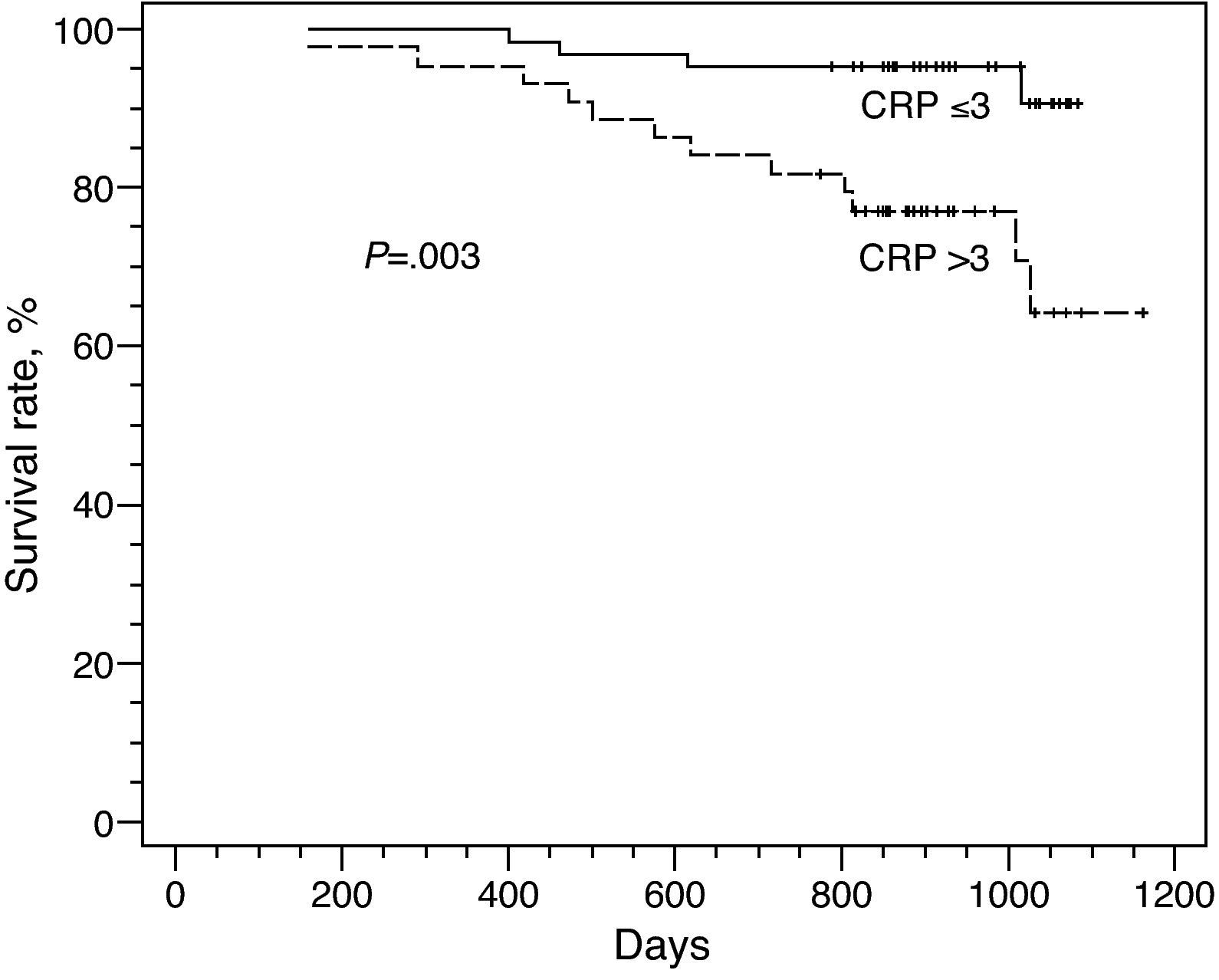
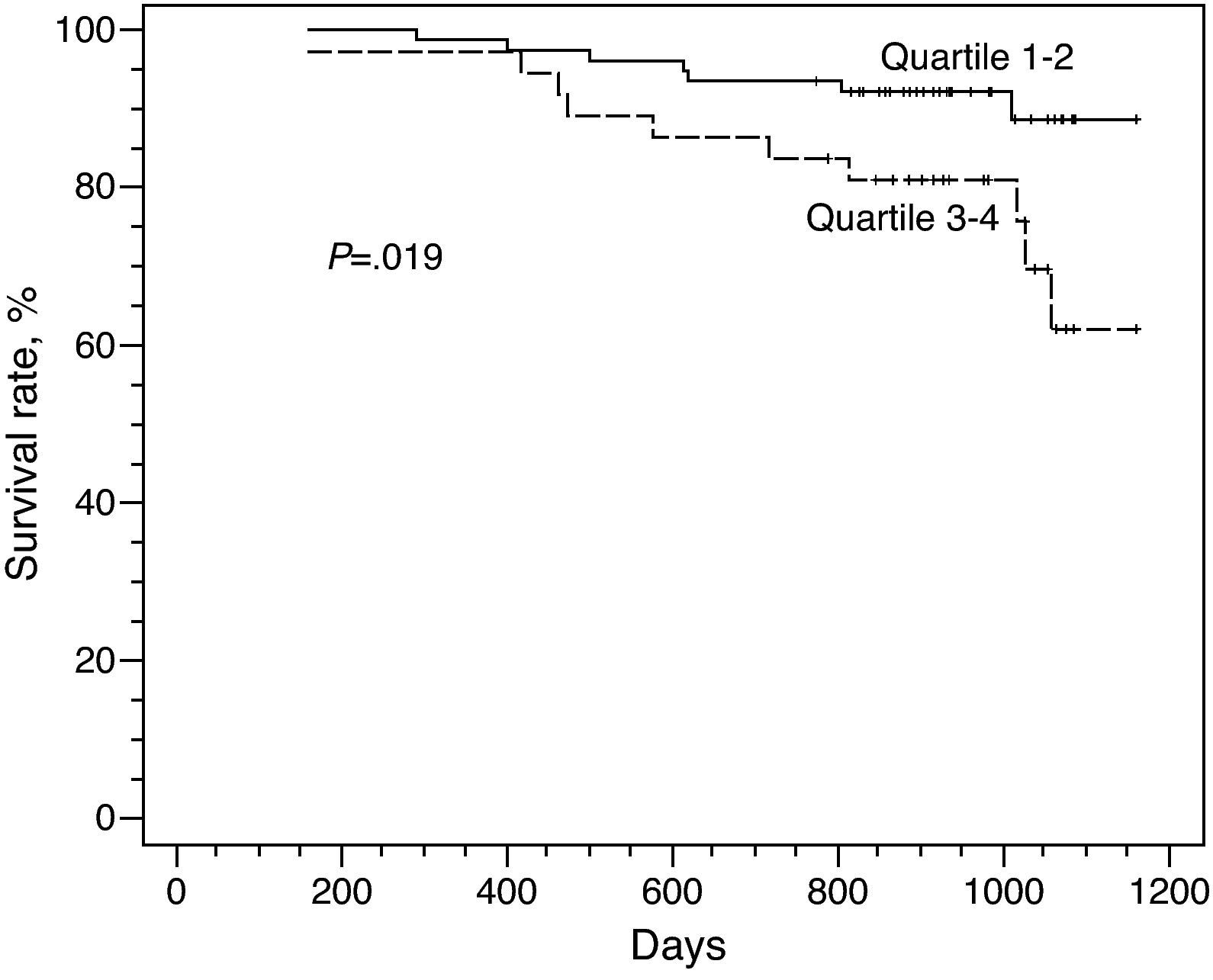
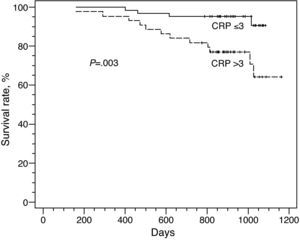
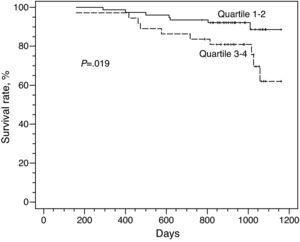
During the periods of the present study, 17 (14.9%) patients died (17/114). In patients with clinically stable COPD and a serum CRP concentration >3mg/l, we identified a lower accumulative survival rate than in those with a value ≤3mg/l (P=.003) (Fig. 1). In the subgroup with a concentration of CRP >3mg/l, there was a mortality rate of 27% (12/44) during the study period. In comparison, in the group with values ≤3mg/l, the mortality rate was 6.3% (4/63). In patients with a BODE score in quartile 3–4, there was a lower accumulative survival rate than in those with a BODE score in quartile 1–2 (P=.02) (Fig. 2). In the subgroup of quartile 3–4, there was a mortality rate of 27% (10/37) during the study period. In comparison, the mortality rate of the subgroup of quartile 1–2 was 9.1% (7/77). The accumulative survival rates of the COPD patients were classified from the worst to the best in the following manner: serum CRP concentration >3mg/l and quartile 3–4; serum CRP concentration >3mg/l and quartile 1–2; serum CRP concentration ≤3mg/l and quartile 3–4; serum CRP concentration ≤3mg/l and quartile 1–2 (P<.001) (Fig. 3). The mortality rates of the COPD subgroups during the study period were likewise classified: serum CRP concentration >3mg/l and quartile 3–4; serum CRP concentration >3mg/l and quartile 1–2; serum CRP concentration ≤3mg/l and quartile 3–4; serum CRP concentration ≤3mg/l and quartile 1–2 were 7/14 (50%); 5/30 (16.7%); 2/11 (9.5%) and 2/45 (4.4%), respectively.
The accumulative survival rates of the patients with COPD were classified from the worst to the best in the following manner: serum CRP concentration>3mg/l and quartile 3–4; serum CRP concentration>3mg/l and quartile 1–2; serum CRP concentration≤3mg/l and quartile 3–4; serum CRP concentration≤3mg/l and quartile 1–2 (P<.001).
The results of the present longitudinal study revealed that serum CRP concentrations and the BODE score are independent prognostic variables for mortality in patients with stable COPD. The accumulative survival rates of the COPD patients were classified from the worst to the best in the following manner: serum CRP concentration >3mg/l and quartile 3–4; serum CRP concentration >3mg/l and quartile 1–2; serum CRP concentration ≤3mg/l and quartile 3–4; serum CRP concentration ≤3mg/l and quartile 1–2 (P<.001). This indicates that the use of the concentration of this reactive and the BODE score combined produced a greater predictive value for mortality in these patients than either parameter alone.
The concentration of CRP is also related to the presence of airflow obstruction.22 de Torres et al.23 found a significant relationship between the concentration and other clinical variables in patients with the disease. Their results demonstrated that the concentration correlated with various clinical parameters, including FEV1, FVC, CI/CPT, classification of COPD severity based on the GOLD initiative, BODE score, PaO2 and 6MWT in a multivariate analysis. However, only these last two parameters were associated with CRP concentration in the multivariate linear regression analysis. de Torres et al.24 also compared the clinical parameters of COPD patients with initial CRP values >3mg/l or ≤3mg/l in another study with a different population, and they did not find any significant differences in FEV1, FVC, CI/CPT, GOLD stage, MMRC scale or BODE score.24 In a later study, only BMI and PaO2 were significantly different between groups with CRP >3mg/l and ≤3mg/l in the univariate analysis. The population of this latter study included patients with moderate or very severe COPD from two pulmonology clinics at two hospitals, which represented a difference from the previous study. Therefore, the correlation between the serum CRP levels and the clinical parameters is conflictive. In the present study, the serum CRP values did not correlate with the BODE scores, not even in the subgroup of patients with levels of FEV1<50% of the reference value or FEV1≥50% of the reference value. The univariate and multivariate analyses also showed that CRP and the BODE score were significant factors for the survival of these patients. This indicates that the correlation between both parameters was not significant in the population of the present study.
CRP is a circulating pentraxin largely, although not exclusively, produced by the hepatocytes as part of an acute phase response.3 The in vitro studies have demonstrated that it can activate the classic complement cascade, up-regulate adhesion molecules and chemoattractive cytokines and induce the synthesis of inflammatory cytokines, such as interleukin (IL)-8 and IL-6, which together amplify the initial inflammatory signal and propagate the chronic inflammatory processes.3 Serum CRP is usually considered an important prognostic variable for cardiovascular mortality. Nevertheless, contradictory findings have been published about whether its concentration is associated with the survival of COPD patients. The results of the de Torres et al. study24 demonstrated that the concentration is not associated with survival in patients with moderate or very severe disease compared with other prognostic clinical parameters, such as the BODE index, MMRC scale, 6MWT, percentage of the FEV1 reference value, CI/CPT ratio <0.25 and PaO2. Nevertheless, the conclusions of the study do not coincide with the two epidemiological studies mentioned,8,9 which demonstrated that the increase in CRP concentrations was independently associated with global and cardiovascular mortality in COPD patients with mild or moderate obstruction of the airways. The present study also showed that the concentration was significantly associated with survival after being adjusted for age, sex and FEV1, even in the subgroup of patients with levels <50% the reference levels. The reason for these conflictive findings can be the different study designs, populations or COPD phenotypes, sample size and other known or unknown factors that probably influence CRP concentrations. Consequently, additional longitudinal studies are required in this direction in order to clarify this problem in more detail.
As the accumulated tests suggest that the mortality in patients with COPD is associated with multiple factors, the progress in the comprehension of the disease and its components will lead to the development of multidimensional scores, such as the frequently used BODE index. The importance of this index is that the prognosis of COPD patients is not associated with an individual factor but instead with different factors that span different phenotypes. This index is an invaluable instrument in the prediction of the need for hospitalization of an individual,7 and it determines the effect of interventions.8–11 In spite of the continued controversy about the possible causal role of CRP, its serum levels correlate with the future risk for morbidity and mortality in the general population.25,26 The present study demonstrates that the combination of CRP with the BODE index can stratify the patients with stable COPD into different risk levels for mortality. The combination of a low-grade systemic inflammation marker and a multidimensional score for predicting mortality in these patients is superior to an individual biological marker or any clinical parameter alone.
This present study has several limitations. In the first place, we evaluate the cardiovascular disease using only the clinical information that is registered, and we have not formally evaluated the presence of an active disease. In addition, the causes of mortality of the patients were not clearly divided into “cardiovascular, respiratory or other” from the clinical histories or from the communication with the families. Second of all, some patients treated with oral or inhaled steroids presented lower concentrations of CRP than the non-treated patients; nevertheless, this difference was not statistically significant. The reason could be the small sample size with a reduced statistical power. Although, in general, inhaled corticosteroid treatment with a long-acting β2 adrenergic agonist does not reduce the concentration of CRP or IL-6 in the serum of patients with COPD for 4 weeks, we consider that some corticosteroids used and their actual effect on this parameter have yet to be clarified.
In short, our study confirms that the serum concentration of CRP as well as the BODE score do not correlate and that both are independent prognostic variables for the survival in patients with stable COPD. A serum CRP concentration >3mg/l and a BODE score in quartile 3–4 are poorer prognostic variables of COPD compared with CRP concentration ≤3mg/l and a BODE score in quartile 1–2. The combination of both precisely predicted the survival of patients with stable COPD. Additional cohort studies with a larger size sample will determine their validity.
FundingThe Chang Gung Memorial Hospital provided funding for this study (CMRPG840421).
Conflict of InterestThe authors declare having no economic relationships with commercial entities with interests in this topic of research.
The authors would like to express their gratitude towards C. Y. Lin for helping with the statistical analysis.
Please cite this article as: Liu S-F, et al. Alto valor de la combinación de la concentración sérica de proteína C reactiva y la puntuación BODE para la predicción de la mortalidad en pacientes con EPOC estable. Arch Bronconeumol. 2011;47:427–32.