Despite current treatments, more than half of patients with asthma are not controlled. The objective was to evaluate the correlation between control perceived by patients and physicians, compared with control evaluated according to criteria of the Spanish Guidelines for Asthma Management (GEMA), and to investigate the factors associated with that control.
MethodsMulticenter, cross-sectional, observational study including 343 patients with severe persistent asthma according to GEMA criteria seen in the Department of Pulmonology and Allergology. The correlation between asthma control perceived by the patient, the physician and according to clinical judgment based on the GEMA criteria was calculated, and a multivariate analysis was used to determine variables related to the perception of asthma control.
ResultsAccording to GEMA criteria, only 10.2% of patients were well controlled, 27.7% had partial control and 62.1% were poorly controlled. Both the physicians and the patients overestimated control: 75.8% and 59.3% of patients had controlled asthma according to the patient and the physician, respectively, and were not controlled according to GEMA (P<.0001). Patients with uncontrolled asthma according GEMA had higher body mass index (P=.006) and physical inactivity (P=.016). Factors associated with a perceived lack of control by both physicians and patients were: nocturnal awakenings (≥1 day/week), frequent use of rescue medication (≥5 days/week) and significant limitation in activities. Discrepant factors between physicians and patients were dyspnea and emergency room visits (patients only), FEV1≤80% and a poorer understanding of the disease by the patient (physicians only).
ConclusionsOnly 10% of patients with severe asthma evaluated in this study are controlled according to GEMA criteria. Patients and physicians overestimate control and the overestimation by patients is greater. Physical inactivity and obesity are associated with a lack of control according to GEMA.
A pesar de los tratamientos actuales más de la mitad de pacientes con asma no están controlados. El objetivo fue evaluar la concordancia entre la percepción de control por parte de pacientes y médicos comparado con el control evaluado según criterios de la Guía española para el manejo del asma (GEMA), así como investigar los factores asociados con dicho control.
MétodosEstudio multicéntrico, observacional y transversal que incluyó 343 pacientes con asma grave persistente según criterios de la GEMA atendidos en consultas de neumología y alergología. Se calculó la concordancia entre control del asma según percepción del paciente, criterio clínico del médico y en función de criterios GEMA, y se utilizó análisis multivariante para determinar variables relacionadas con la percepción de control del asma.
ResultadosSegún criterios GEMA solo el 10,2% de pacientes estaba bien controlado, el 27,7% presentaba control parcial y el 62,1% estaba mal controlado. Tanto médicos como pacientes sobrestimaron el control: el 75,8 y 59,3% de individuos con asma controlada según el propio paciente y su médico, respectivamente, no estaba controlada según GEMA (p<0,0001). Los pacientes con asma no controlada según GEMA presentaron un mayor índice de masa corporal (p=0,006) y más sedentarismo (p=0,016). Los factores asociados a la falta de control percibida tanto por médicos como por pacientes fueron: despertares nocturnos (≥ 1 día/semana), uso frecuente de medicación de rescate (p=0 días/semana) y limitación importante de actividades. Los factores discordantes entre médicos y pacientes fueron: disnea y visitas a urgencias (solo pacientes); FEVI ≤ 80% y peor conocimiento de la enfermedad por el paciente (solo médicos).
ConclusionesSolo el 10% de pacientes con asma grave evaluados en este estudio está controlado según criterios GEMA. Tanto pacientes como médicos sobrestiman el control, con una mayor sobrestimación en pacientes. El sedentarismo y la obesidad se asocian con la falta de control según GEMA.
The prevalence of asthma in Spain is approximately 5%.1 Most patients have mild or moderate disease that can be controlled with relative ease. Around 10% of patients have severe asthma requiring long-term treatment with high doses of inhaled or oral corticosteroids combined with adrenergic beta-2 agonists.
Several studies have shown that, despite the availability of therapy, more than half of patients are not well controlled in clinical practice.2,3 Asthma control was recently defined as the extent to which disease manifestations are absent or reduced to a maximum with therapeutic interventions.4 Asthma control has acquired an important role in the management of the disease and is now considered as a reference objective in treatment guidelines. However, there may be discrepancies between physician- and patient-perceived asthma control, and between these latter and the definition of control according to the guidelines. Discrepancies appear to be less pronounced in patients with severe asthma than in those with less severe manifestation.5
Various risk factors associated with poor disease control have been described, including age, educational level, asthma severity and even patients’ knowledge of the disease.2,6,7 Improved awareness of these factors could lead to improved management of asthma.8
The aims of this study were to evaluate the correlation between physician- and patient-perceived control compared with control evaluated according to the criteria of the Spanish Guidelines for Asthma Management (GEMA), and to investigate the factors associated with perceived control.
Patients and MethodsA multicenter, observational, cross-sectional study was performed between November 2009 and May 2010 on patients seen in a specialized clinic who met the inclusion criteria. Criteria included patients aged 18 years of age or more, seen in pulmonology and allergology clinics, with spirometry performed within the previous month and persistent severe asthma diagnosed according to the GEMA guidelines9: i.e., continuous symptoms during the day, frequent nighttime symptoms, use of rescue medication several times a day, severe limitation of activities, forced expiratory volume (FEV1) ≤60% or ≥2 exacerbations per year. Patients participating in other clinical studies were excluded. The investigators collected study data from the patients’ clinical records and from the information obtained from the patient in the single study visit.
The study was performed in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. The study protocol was approved by the ethics committee of the Hospital Clínic (Barcelona) and reported to the Spanish Agency for Medicinal Products (AEMPS). Informed consent was obtained from all participants.
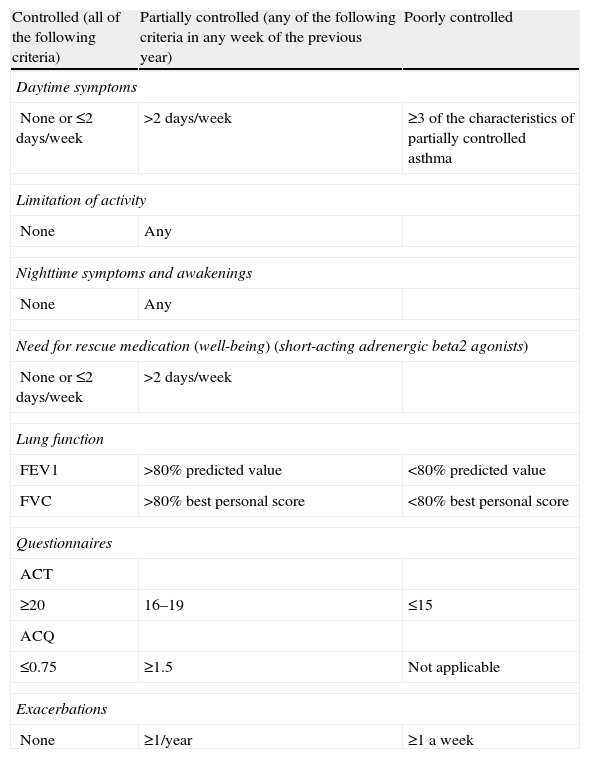
The principal endpoint was physician- and patient-perceived asthma control, and control according to GEMA criteria (Table 1). In the first case, the patients were asked how they perceived their asthma control, on the basis of their opinion only. They were given 3 choices (controlled, partially controlled or poorly controlled). Physician-perceived asthma control was obtained in a similar fashion. GEMA asthma control criteria (listed in Table 1) were evaluated for each patient and the Asthma Control Questionnaire (ACQ) was self-administered by the patient on the day of the visit,10 taking into account daytime symptoms, nighttime symptoms, limitation of activity and use of rescue medication (short-acting bronchodilators, such as salbutamol) in the previous week, and percent predicted FEV1. The only criteria that referred to the previous year (presence of exacerbations) was obtained from patient interviews and a review of clinical records.11 Only exacerbations in which bronchial obstruction was established clinically and corticosteroids were required were taken into account, as stipulated in the GEMA recommendations. The physician recorded the latest available forced vital capacity (FVC) and FEV1 measurements in the ACQ.
Classification of Asthma Control According to GEMA Criteria.
| Controlled (all of the following criteria) | Partially controlled (any of the following criteria in any week of the previous year) | Poorly controlled |
| Daytime symptoms | ||
| None or ≤2 days/week | >2 days/week | ≥3 of the characteristics of partially controlled asthma |
| Limitation of activity | ||
| None | Any | |
| Nighttime symptoms and awakenings | ||
| None | Any | |
| Need for rescue medication (well-being) (short-acting adrenergic beta2 agonists) | ||
| None or ≤2 days/week | >2 days/week | |
| Lung function | ||
| FEV1 | >80% predicted value | <80% predicted value |
| FVC | >80% best personal score | <80% best personal score |
| Questionnaires | ||
| ACT | ||
| ≥20 | 16–19 | ≤15 |
| ACQ | ||
| ≤0.75 | ≥1.5 | Not applicable |
| Exacerbations | ||
| None | ≥1/year | ≥1 a week |
ACQ, asthma control questionnaire; ACT, asthma control test; FEV1, forced expiratory volume in first second; FVC, forced vital capacity.
Physicians also completed an ad hoc questionnaire with the following patient variables, and these data were used to complete the patient's clinical profile and/or were included in the subsequent multivariate analyses: (1) sociodemographic and anthropometric data; (2) physical activity (active: sport or any physical activity >3 times a week; moderately active: 2 or 3 times a week; sedentary: none); (3) smoking habit (smoker [defined as smoker in the 30 days prior to the study, including daily smokers], ex-smoker [<1 year, ≥1 year] or never-smoker); (4) asthma clinical history (date of diagnosis, number of visits to emergency room, admissions and unscheduled visits to primary care for asthma in the last year, days with nocturnal awakenings in the last 4 weeks, average use of rescue medication per week, presence and intensity of cough and/or expectoration, concomitant diseases acting as inflammatory stimuli); (5) clinical tests (FVC, FEV1, total IgE, skin prick tests); (6) current asthma treatment (beclometasone/fluticasone/budesonide/formoterol/salmeterol/montelukast/theophyllines/omalizumab/others); (7) anxiolytic or antidepressant treatment; and (8) additional evaluations (AQLQ quality of life mini-questionnaire,12 questionnaire evaluating knowledge of asthma,13 Hospital Anxiety and Depression [HAD] scale,14 Nijmegen questionnaire [hyperventilation]15).
Statistical AnalysisQualitative or discrete quantitative variables were summarized using absolute and relative frequencies, while continuous quantitative variables were described using central tendency and dispersion measurements. The degree of concordance between (a) patient-perceived asthma control and GEMA criteria, (b) physician-perceived asthma control and GEMA criteria and (c) physician-perceived and patient-perceived control was calculated. Differences between controlled patients and uncontrolled patients were evaluated with Chi-squared tests (categorical variables) and the Mann–Whitney–Wilcoxon non-parametric test (continuous variables). The variables with greatest association in the bivariate analysis were included in multivariate logistic regressions in order to determine the variables with a significant independent effect in the perception of asthma control according to patients or physicians. The choice of possible variables was conducted similarly to previous studies. Hosmer and Lemeshow's goodness-of-fit test was used to determine the total variation explained by the model.
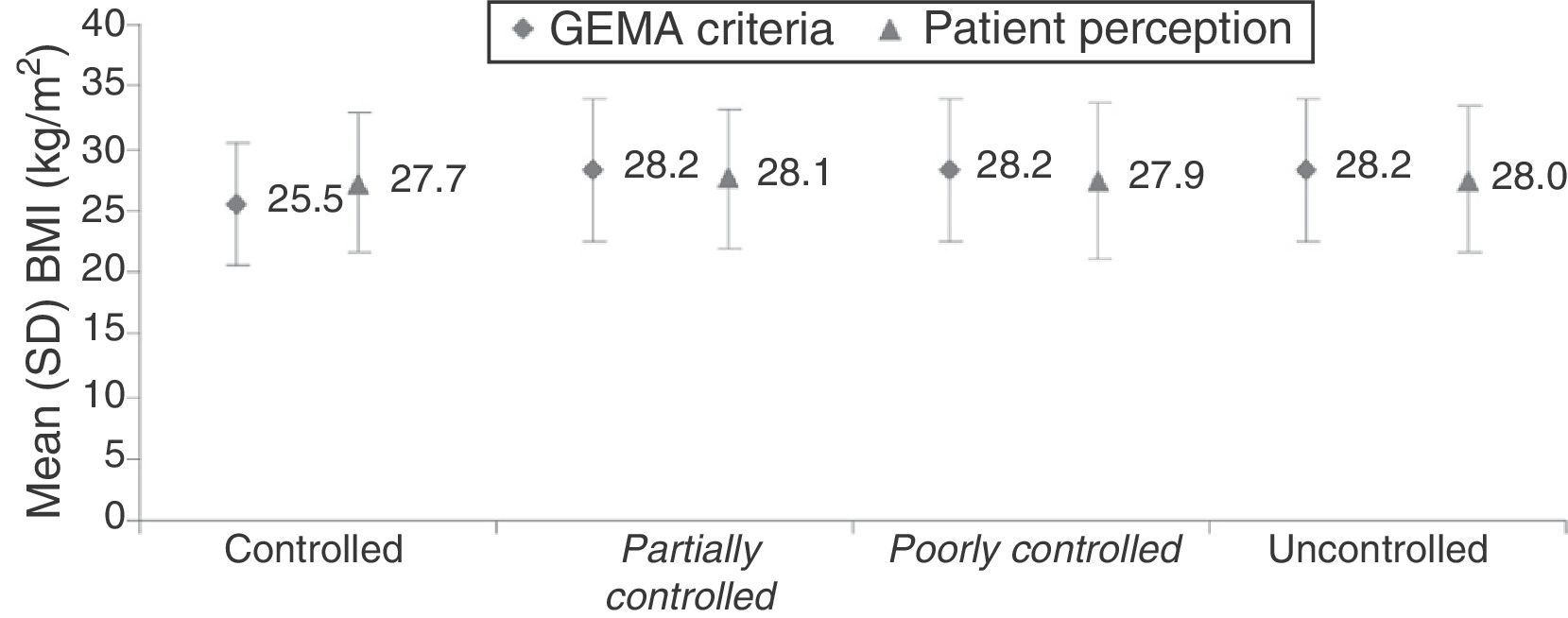
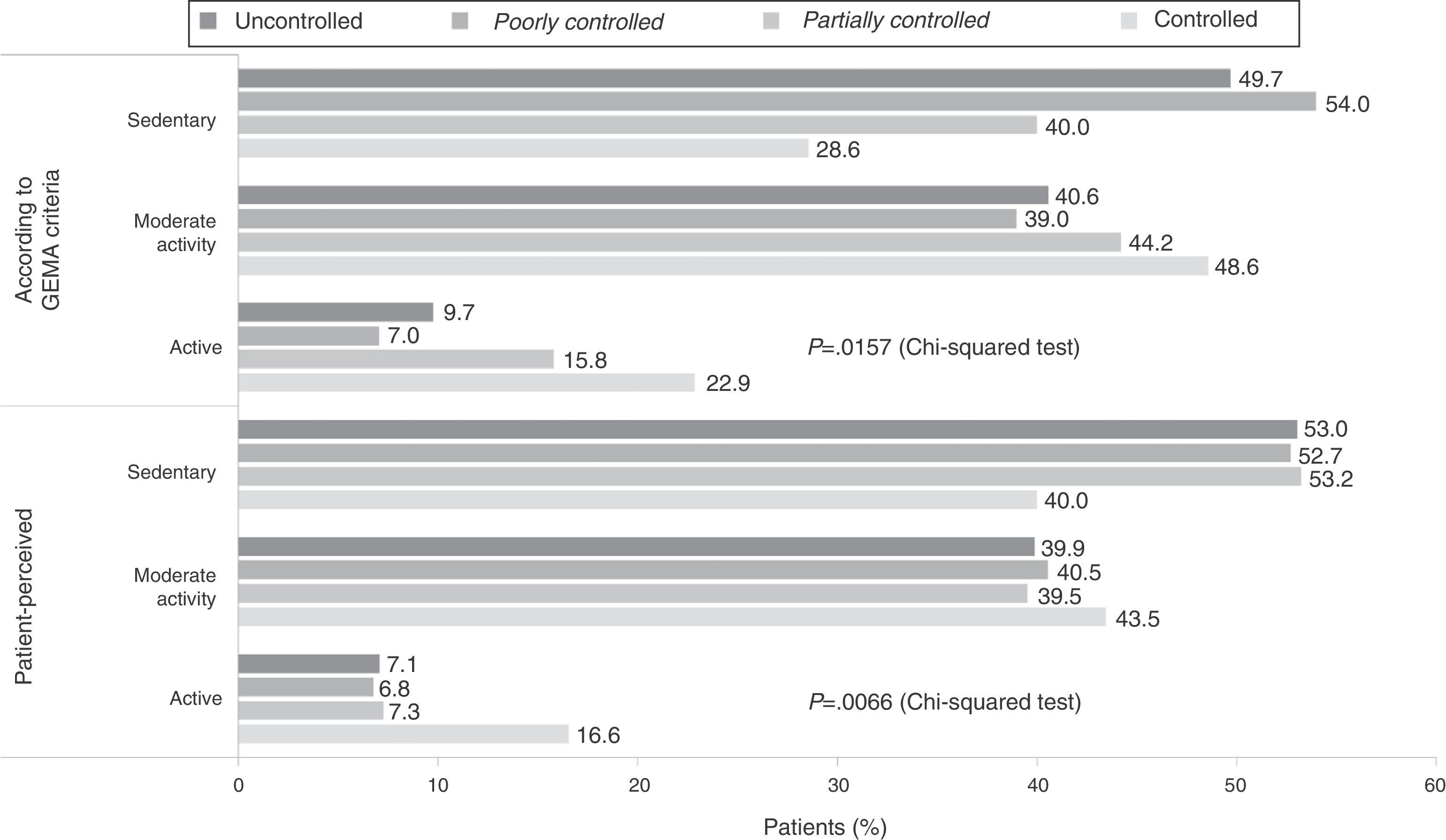
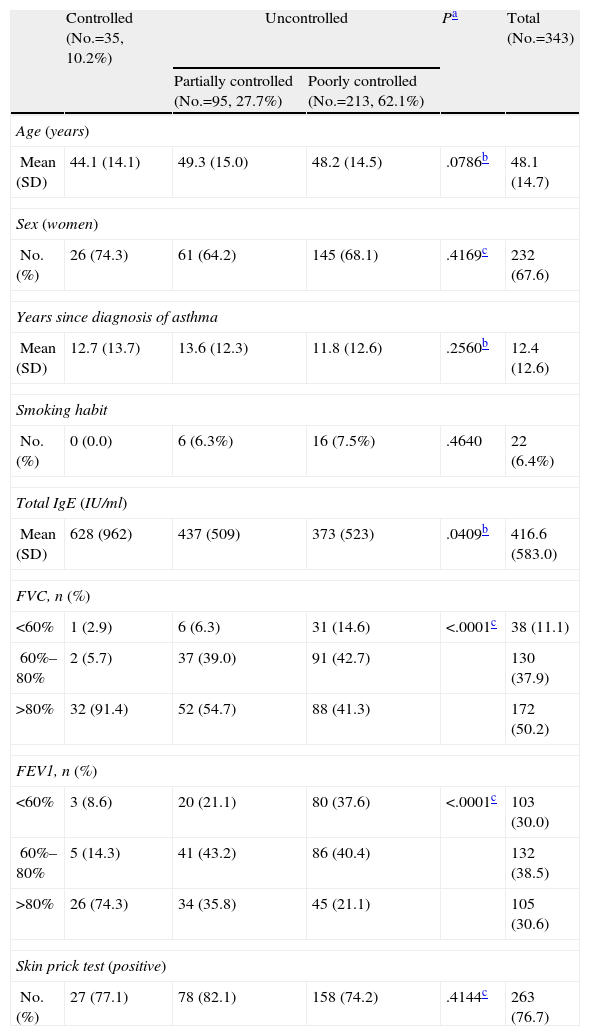
ResultsPatient Characteristics and Control According to the Spanish Guidelines for Asthma ManagementA total of 343 patients with a mean age (standard deviation [SD]) of 48.1 (14.7) years were included, of whom one third were women. According to GEMA criteria, only 10.2% of patients were controlled, 27.7% had partial control and 62.1% were poorly controlled. Table 2 shows baseline demographic and clinical data by grades of control. As expected, patients controlled according to GEMA had significantly higher FVC and FEV1 values (Table 2). Moreover, they had higher levels of total IgE (P=.0409). Patients with uncontrolled asthma according to GEMA had a higher body mass index (BMI) (Fig. 1, P=.006) and a more sedentary lifestyle (Fig. 2, P=.016), as well as a tendency toward a higher mean age (48.5 [14.7] vs 44.1 [14.1] years in the controlled asthma subgroup, P=.079).
Demographic and Clinical Data by Asthma Control According to GEMA Criteria (Controlled/Uncontrolled [Partially Controlled/Poorly Controlled]).
| Controlled (No.=35, 10.2%) | Uncontrolled | Pa | Total (No.=343) | ||
| Partially controlled (No.=95, 27.7%) | Poorly controlled (No.=213, 62.1%) | ||||
| Age (years) | |||||
| Mean (SD) | 44.1 (14.1) | 49.3 (15.0) | 48.2 (14.5) | .0786b | 48.1 (14.7) |
| Sex (women) | |||||
| No. (%) | 26 (74.3) | 61 (64.2) | 145 (68.1) | .4169c | 232 (67.6) |
| Years since diagnosis of asthma | |||||
| Mean (SD) | 12.7 (13.7) | 13.6 (12.3) | 11.8 (12.6) | .2560b | 12.4 (12.6) |
| Smoking habit | |||||
| No. (%) | 0 (0.0) | 6 (6.3%) | 16 (7.5%) | .4640 | 22 (6.4%) |
| Total IgE (IU/ml) | |||||
| Mean (SD) | 628 (962) | 437 (509) | 373 (523) | .0409b | 416.6 (583.0) |
| FVC, n (%) | |||||
| <60% | 1 (2.9) | 6 (6.3) | 31 (14.6) | <.0001c | 38 (11.1) |
| 60%–80% | 2 (5.7) | 37 (39.0) | 91 (42.7) | 130 (37.9) | |
| >80% | 32 (91.4) | 52 (54.7) | 88 (41.3) | 172 (50.2) | |
| FEV1, n (%) | |||||
| <60% | 3 (8.6) | 20 (21.1) | 80 (37.6) | <.0001c | 103 (30.0) |
| 60%–80% | 5 (14.3) | 41 (43.2) | 86 (40.4) | 132 (38.5) | |
| >80% | 26 (74.3) | 34 (35.8) | 45 (21.1) | 105 (30.6) | |
| Skin prick test (positive) | |||||
| No. (%) | 27 (77.1) | 78 (82.1) | 158 (74.2) | .4144c | 263 (76.7) |
FEV1, forced expiratory volume in first second; FVC, forced vital capacity; GEMA, Spanish Guidelines for Asthma Management; IU, international units.
BMI in subgroups defined as asthma control according to GEMA and according to the patient him/herself (controlled/uncontrolled [partially controlled/poorly controlled]). Differences between subgroups according to GEMA criteria were significant (P=.0065) and non-significant according to patient perception (P=.5088).
Omalizumab use, prescribed in 193 of 342 patients, was significantly more prevalent in patients with controlled asthma according to GEMA (71.4%) than in partially controlled patients (63.2%) and those with poor control (49.5%) (P<.005).
No significant association between smoking and asthma control according to GEMA was observed (P=.464).
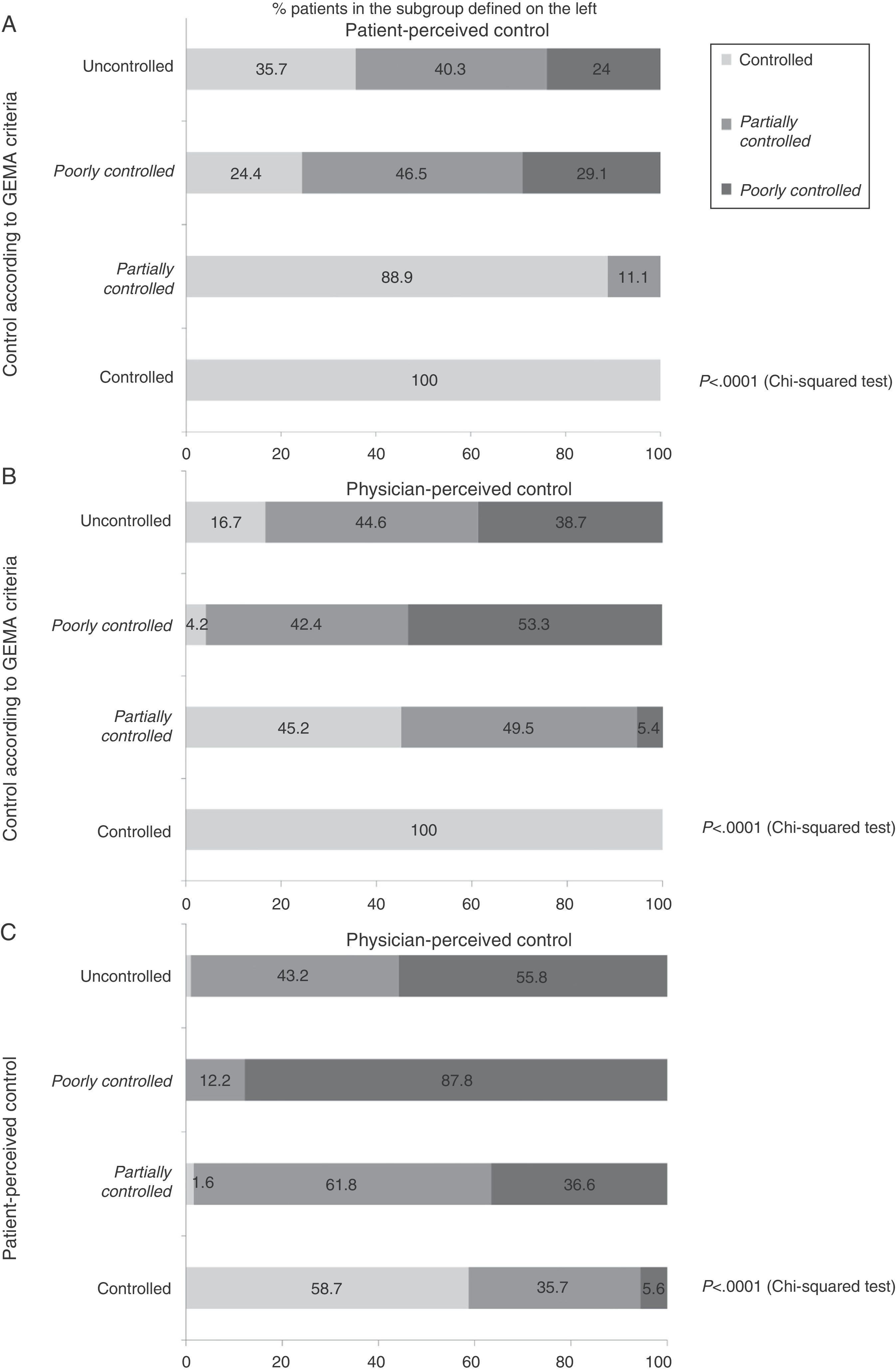
Concordance Between Asthma Control According to the Spanish Guidelines for Asthma Management, Patients and PhysiciansAccording to patients’ perceptions, 42.3% of the population were well controlled, 36.1% had partial control and 21.6% were poorly controlled. According to the physicians, these percentages were 25.7%. 39.7% and 34.6% of patients, respectively.
When the different asthma control criteria were compared, significant differences were observed for all the comparisons made: patient vs GEMA (P<.0001); physician vs GEMA (P<.0001) and patient vs physician (P<.0001). Both patients and physicians overestimated asthma control: in the subgroup of patients with uncontrolled asthma according to GEMA, 35.7% considered themselves to be well controlled (Fig. 3A) and 16.7% were well controlled according to their physician (P<.0001) (Fig. 3B). Of the total sample, 75.8% and 59.3% of patients controlled from the perspective of the patient and the physician, respectively, did not meet the criteria for control according to GEMA.
Patients overestimated asthma control more than physicians: 41.3% of patients who considered themselves controlled were not well controlled according to their physicians (P<.0001) (Fig. 3C).
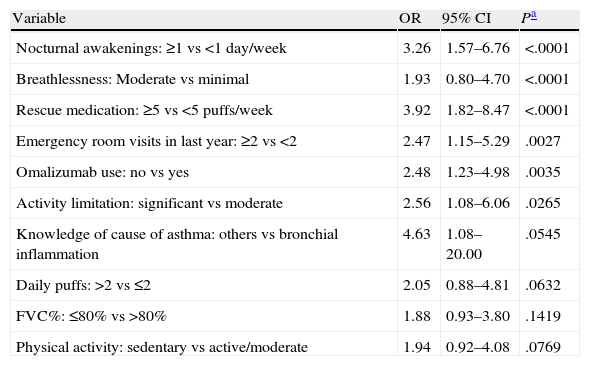
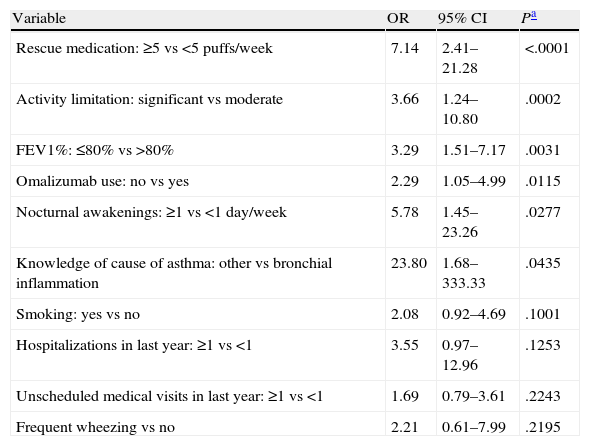
Determinant Factors for Perception of Control by Patients and PhysiciansThe main factors associated with patient- and physician-perceived lack of control are shown in Tables 3 and 4, respectively (multivariate logistic regression analysis). Other variables tested but not included in either of the two final models were age, sex, level of studies, BMI, time since diagnosis, morning symptoms and treatment with theophyllines.
Multivariate Logistic Regression Model to Predict Patient-Perceived Lack of Asthma Control.
| Variable | OR | 95% CI | Pa |
| Nocturnal awakenings: ≥1 vs <1 day/week | 3.26 | 1.57–6.76 | <.0001 |
| Breathlessness: Moderate vs minimal | 1.93 | 0.80–4.70 | <.0001 |
| Rescue medication: ≥5 vs <5 puffs/week | 3.92 | 1.82–8.47 | <.0001 |
| Emergency room visits in last year: ≥2 vs <2 | 2.47 | 1.15–5.29 | .0027 |
| Omalizumab use: no vs yes | 2.48 | 1.23–4.98 | .0035 |
| Activity limitation: significant vs moderate | 2.56 | 1.08–6.06 | .0265 |
| Knowledge of cause of asthma: others vs bronchial inflammation | 4.63 | 1.08–20.00 | .0545 |
| Daily puffs: >2 vs ≤2 | 2.05 | 0.88–4.81 | .0632 |
| FVC%: ≤80% vs >80% | 1.88 | 0.93–3.80 | .1419 |
| Physical activity: sedentary vs active/moderate | 1.94 | 0.92–4.08 | .0769 |
FVC, forced vital capacity; CI, confidence interval; OR, odds ratio.
Multivariate Logistic Regression Model for Physician-Perceived Lack of Asthma Control.
| Variable | OR | 95% CI | Pa |
| Rescue medication: ≥5 vs <5 puffs/week | 7.14 | 2.41–21.28 | <.0001 |
| Activity limitation: significant vs moderate | 3.66 | 1.24–10.80 | .0002 |
| FEV1%: ≤80% vs >80% | 3.29 | 1.51–7.17 | .0031 |
| Omalizumab use: no vs yes | 2.29 | 1.05–4.99 | .0115 |
| Nocturnal awakenings: ≥1 vs <1 day/week | 5.78 | 1.45–23.26 | .0277 |
| Knowledge of cause of asthma: other vs bronchial inflammation | 23.80 | 1.68–333.33 | .0435 |
| Smoking: yes vs no | 2.08 | 0.92–4.69 | .1001 |
| Hospitalizations in last year: ≥1 vs <1 | 3.55 | 0.97–12.96 | .1253 |
| Unscheduled medical visits in last year: ≥1 vs <1 | 1.69 | 0.79–3.61 | .2243 |
| Frequent wheezing vs no | 2.21 | 0.61–7.99 | .2195 |
FEV1, forced expiratory volume in first second; FVC, forced vital capacity; OR, odds ratio.
Five independent factors significantly associated with patient-perceived lack of control were found (Table 3): nocturnal awakenings (P<.0001), a greater perception of breathlessness evaluated according to the Nijmegen questionnaire (P<.0001), more frequent use of rescue medication (P<.0001), more emergency room visits in the last year (P=.0027) and greater limitation in activities of daily living (P=.0265). The model was significant and the Hosmer and Lemeshow goodness-of-fit adjustment gave a P-value of .5080, showing that the analysis explains more than 50% of the variation in patient-perceived asthma control.
In the model for predicting physician-perceived lack of control (Table 4), a total of 6 significant predictive variables were obtained: more frequent use of rescue medication (P<.0001), greater perceived limitation in activities of daily living (P=.0002), FEV1 lower than 80% (P=.0031), no omalizumab treatment (P=.0115), nocturnal awakenings (P=.0277) and misunderstanding of the biological cause of asthma shown in the asthma knowledge evaluation questionnaire (P=.0435). This second model was also highly significant (Hosmer and Lemeshow goodness-of-fit test: P=.8776) and explained most of the variation associated with physician-perceived lack of control (around 88% variation).
DiscussionPrincipal Results and Comparison With Other StudiesThis study, carried out in a large Spanish cohort of patients with persistent severe asthma, shows that both patients and physicians overestimate asthma control as defined by the clinical criteria recommended by GEMA. Moreover, it shows that the main factors associated with lack of control according to GEMA are sedentary lifestyle and higher BMI. In our cohort, the degree of disease control according to the guidelines was very low: only 1 in 10 patients was well controlled. Accordingly, the prevalence of uncontrolled asthma (around 90%) was clearly higher than that of other studies which record a range of 55.0%–71.6%.2,16,17 These differences may be due to the use of other definitions of control and the lack of objective and reliable indicators to complement the information on patient-reported symptoms. A recent study showed that even asthmatics who are well controlled according to asthma control questionnaires (e.g., ACQ) present persistent corticosteroid-sensitive inflammation.18
Although asthma control is overestimated by both patients and physicians, patients showed higher subjective perception of control than physicians. This discordance between physician- and patient-perceived control has already been observed in previous studies.5 A British study found that only 52% of classifications were consistent between physicians and patients.19 Similarly, it is interesting to note the results of a recent study conducted in Spain20 in the same healthcare setting as ours, that showed a considerable degree of discordance between patient and the physician perception of aspects such as treatment satisfaction and impact of asthma on daily life (for both variables, in 26% of the cases the physicians’ perception was lower than the patients’). The physician-patient discordance was shown to increase as asthma control worsened (being about 30% in the group of controlled patients, but over 73% in the case of patients with poor asthma control). Although these results underline the importance of the perception of control in the asthma patient, current Spanish guidelines do not take this opinion into account.
In this study, no differences were reported in asthma control with respect to age, sex or smoking habit. In contrast, sedentary lifestyle, higher BMI and poorer knowledge of the disease were associated with a poorer degree of control in severe asthma. These results coincide partially with those of other studies. In the REACT study,16 no significant differences were found in control with respect to age, ethnic origin, lifestyle (urban, suburban or rural) or the type of health insurance. However, lack of control was more common in women and in patients from lower income groups and lower educational level. Díez et al.2 identified sex, ethnic group, BMI, smoking habit, educational level, physical activity and medical history as factors associated with asthma control.
The association between poor asthma control and higher BMI and/or sedentary lifestyle has also been described in other publications.21–24 A recent review concluded that obesity increases the prevalence and incidence of asthma, although this effect appears to be modest.25 Although no causal mechanism has been described, lack of control in obese patients may be explained by mechanical and inflammatory phenomena. In particular, obesity affects pulmonary and airway anatomy and increases abdominal wall and chest mass. This leads to reduced bronchial diameter and residual functional capacity and produces a state of chronic inflammation that contributes significantly to hyperresponsiveness.26 In contrast to another review,27 no association was found between control and smoking, probably because of differences in the definition of asthma control.
In multivariate analyses, common factors associated with both physician- and patient-perceived lack of control included nocturnal awakenings, frequent use of rescue medication and significant limitation of activities. On the other hand, 4 factors were perceived differently by physicians and patients. When patients’ perception was analyzed, a marked perception of breathlessness and visits to the emergency room in the last year were significant. When physicians’ perception was analyzed, low FEV1 and poor understanding of the biological cause of asthma were significant. Thus, the most important variables in determining the perception of poor asthma control, particularly for patients, are generally related with symptoms and interference in daily life and sleep, while physicians also take lung function into account. With regard to these results, a recent study28 showed that uncontrolled patients had more catastrophic thinking in the absence of exacerbation, as well as more activity limitation. Thus, the mental component appears to be important in the effective management of uncontrolled asthma.19 It is interesting to note that neither morning symptoms nor previous exacerbations were taken by the physicians as predictive factors for lack of control. These 2 variables are taken into account in the GEMA classification, but our results suggest that physicians either do not use them in their clinical practice or do not give them the importance they deserve.
LimitationsSince this was an observational, uncontrolled, non-interventional study, there are several limitations inherent in the design, and selection or data bias cannot be ruled out. The amount of information available for each patient and the sample size were limited. Accordingly, it would be of interest to replicate the results in a larger, more diverse group of patients with severe asthma.
Implications for Future Research and Clinical PracticeControl of severe asthma is considered the principal objective of clinical guidelines. In our opinion, the findings of this study have important implications, since they reveal lack of control of asthma in clinical practice and the direct effect this has on patients’ quality of life. Our results also show that, from the patients’ point of view, symptoms should be considered important when evaluating control of severe asthma. In this respect, guidelines should consider the perspective of the patient in order to facilitate physician–patient consensus. Overestimation by physicians must be reduced if better disease control is to be achieved, and raising awareness of the importance of correctly questioning patients about their morning symptoms and exacerbations in the weeks or months before the visit could improve detection of poorly controlled patients. Future studies must also address the cost-efficacy ratio of treatment strategies, based on differences in control achieved by each of those strategies.
ConclusionsIn this study, only 1 in 10 patients with severe persistent asthma monitored in specialized clinics are well controlled according to GEMA criteria. Both patients and physicians overestimate control, patients more so, and there is low concordance between perceptions and the GEMA classification. Sedentary lifestyle and obesity are associated with a lack of control according to GEMA, while physicians and patients associate poor control with increased nocturnal symptoms, limitation in activities and use of rescue medication. Our study suggests that a comprehensive approach to patient management, including physical exercise and better eating habits, could improve the control of severe asthma.
FundingThis study was sponsored by Novartis Farmacéutica S.A. This company also funded assistance in scientific writing.
Author ContributionMCV designed the study and coordinated the study group. All authors participated in the collection of clinical data, reviewed the manuscript and approved the final version.
Conflict of InterestsCP is a member of the International Scientific Advisory Board of Novartis Farmacéutica S.A. and has received research grants from Leti S.A., Uriach S.A. and Chiesi. MCV has received payments from Novartis Farmacéutica S.A. for giving conferences and for consultancy and support for attending scientific meetings. LH, JG and JC are employees of Novartis Farmacéutica S.A., Spain.
Our thanks to Emili González-Pérez of the Medical Department of TFS Develop (Barcelona), for providing scientific writing assistance for this article.
Please cite this article as: Vennera M C, Picado C, Herráez L, Galera J, Casafont J, en nombre del Grupo de Estudio CONTROL. Factores asociados con el asma grave no controlada y con la percepción del control por parte de médicos y pacientes. Arch Bronconeumol. 2014;50:384–391.

![BMI in subgroups defined as asthma control according to GEMA and according to the patient him/herself (controlled/uncontrolled [partially controlled/poorly controlled]). Differences between subgroups according to GEMA criteria were significant (P=.0065) and non-significant according to patient perception (P=.5088). BMI in subgroups defined as asthma control according to GEMA and according to the patient him/herself (controlled/uncontrolled [partially controlled/poorly controlled]). Differences between subgroups according to GEMA criteria were significant (P=.0065) and non-significant according to patient perception (P=.5088).](https://static.elsevier.es/multimedia/15792129/0000005000000009/v1_201408240420/S1579212914001967/v1_201408240420/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)
![Level of physical activity in subgroups defined by asthma control according to GEMA (top figure) and the patient (lower figure) (controlled/uncontrolled [partially controlled/poorly controlled]). Level of physical activity in subgroups defined by asthma control according to GEMA (top figure) and the patient (lower figure) (controlled/uncontrolled [partially controlled/poorly controlled]).](https://static.elsevier.es/multimedia/15792129/0000005000000009/v1_201408240420/S1579212914001967/v1_201408240420/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)








