Lung cancer is the leading cause of cancer death worldwide and, unfortunately, the majority of patients present with advanced/metastatic disease.1 A significant proportion of lung cancer patients present with just one or few distant metastases (oligometastatic patients) on imaging, which raise diagnostic and therapeutic concerns and may have a different prognosis than patients with a larger number of distant metastases.2 Tissue diagnosis of (oligometastatic) extrapulmonary lesions in certain patients may allow differentiation between extrapulmonary lung cancer metastasis and an organ-specific primary tumor. We present the case of a patient in whom a triple computed-tomography (CT)-guided core-needle biopsy performed in a single interventional procedure allowed the diagnosis and correct staging of two simultaneous neoplasms.
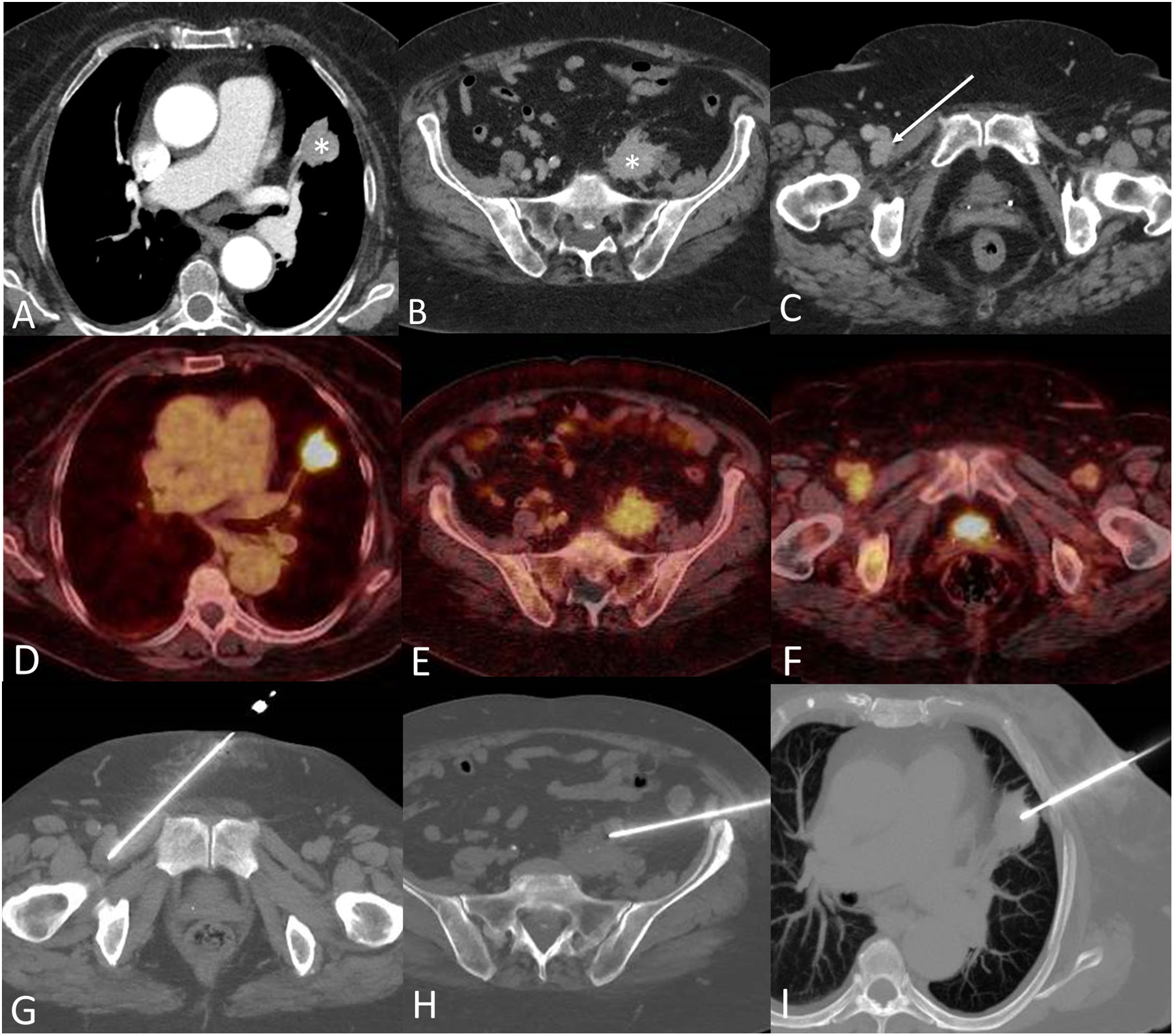
A 74-year-old active smoker female was found to have a suspicious lung nodule in the left upper lobe (Fig. 1A). An 18F-fluorodeoxyglucose (FDG) whole-body positron emission tomography/CT (PET/CT) performed for staging purposes ruled out mediastinal involvement but detected two additional extrathoracic lesions: a left retroperitoneal mass (Fig. 1B) and an enlarged right inguinal lymph node (Fig. 1C). PET/CT also confirmed that the FDG-avidity of the lung lesion (maximum standardized uptake value [SUVmax]: 9.8) was significantly different than that of the extrapulmonary lesions (SUVmax of retroperitoneal mass: 5.7; SUVmax of inguinal lymph node: 5.2), suggesting the possibility that the three lesions could represent different conditions (Fig. 1D–F). Since the patient was taking apixaban for atrial fibrillation, the interventional thoracic radiologist proposed to attempt a triple CT-guided core-needle biopsy during one single session. The uneventful triple CT-guided core-needle biopsy procedure was performed sequentially: first, the lesion with the lowest anticipated biopsy-related risk (the inguinal lymph node) was biopsied (Fig. 1G); second, the lesion with an intermediate biopsy-related risk (the retroperitoneal mass) was biopsied (Fig. 1H); and last, the lesion with the highest biopsy-related risk (the lung nodule) was biopsied (Fig. 1I). The pathological diagnosis confirmed that the pulmonary lesion was a primary lung adenocarcinoma (stage I) whereas the other 2 lesions represented a non-Hodgkin's lymphoma. The patient was treated first for her lung cancer (thoracoscopic surgery) and 1 month later she initiated systemic chemo-immunotherapy for the non-Hodgkin's lymphoma.
(A) Axial CT image (lung window) shows a suspicious lung nodule in the left upper lobe (asterisk). (B and C) Axial CT images show an ill-defined left retroperitoneal mass (B, asterisk) and an enlarged right lymph node (C, arrow). (D–F) Axial fused PET/CT images corresponding to lesions shown in A–C, respectively, show intense FDG uptake by the left upper lobe lung nodule but mild FDG avidity by the retroperitoneal lesion and inguinal lymph node. (G–I) Axial CT images show the needles targeting the enlarged right inguinal lymph node (G), the left retroperitoneal lesion (H), and the left upper lobe nodule (I), respectively. The duration of the triple lung biopsy procedure was 54min (time elapsed between the acquisition of the first CT scout and the last series acquisition), and the patient was discharged 6h following the procedure.
A significant proportion of lung cancer patients present with just one or few distant metastases (oligometastatic patients) on imaging, which raise diagnostic and therapeutic concerns and may have a different prognosis than patients with a larger number of distant metastases.3 Moreover, the detection on imaging tests of one or just a few extrapulmonary lesions in patients with lung cancer does not necessarily imply that they correspond to metastases.4 In patients with oligometastatic extrapulmonary disease, tissue diagnosis may allow differentiation between extrapulmonary lung cancer metastasis and an organ-specific primary tumor, and thus may significantly impact patient staging and management. Unlike conventional staged-biopsy procedures in patients with more than one tumor lesion (in which patients return following a convalescent period for the second or subsequent biopsy), our single-session triple CT-guided biopsy allowed an expeditious histological diagnosis of two different neoplasms, a correct staging of both malignant tumors, and a prompt management of both cancers.
We believe that our case is interesting since a triple percutaneous CT-guided biopsy performed in a single interventional procedure in lung cancer patients has not been previously documented. We also believe that histological confirmation of suspected extrapulmonary metastases should be attempted as early as possible in some oligometastatic lung cancer patients, especially if imaging modalities (particularly PET/CT) suggest a differing metabolic behavior.
Authors’ contributionsThe four authors have made substantial contributions regarding not only the conception and design of the manuscript, but also the drafting and critical revision of the article.
Source of fundingNo one has provided financial support for the preparation of this manuscript.
Conflict of interestThe authors declare no conflict of interest.