We report the case of a 77-year-old man with hypertension and diabetes who underwent revascularization for ischemic heart disease 2 years previously. In 2013, lower bilobectomy extended to the pericardium was performed due to pulmonary follicular lymphoma. A manual bronchial suture was made and the pericardial defect was lined with PTFE mesh to prevent cardiac herniation.
Since 2015, he has had recurrent, self-limiting episodes of hemoptysis, along with habitual purulent expectoration. Prior to the onset of these slowly advancing symptoms, imaging tests showed soft tissue formation in the intermediate bronchus stump, so the prosthetic material was partially removed by rigid bronchoscope. After this first rigid bronchoscopy (no photographic images available), the patient was monitored with fiberoptic bronchoscopy every 8–10 weeks, and no major changes with regard to migration of the prosthetic material were observed.
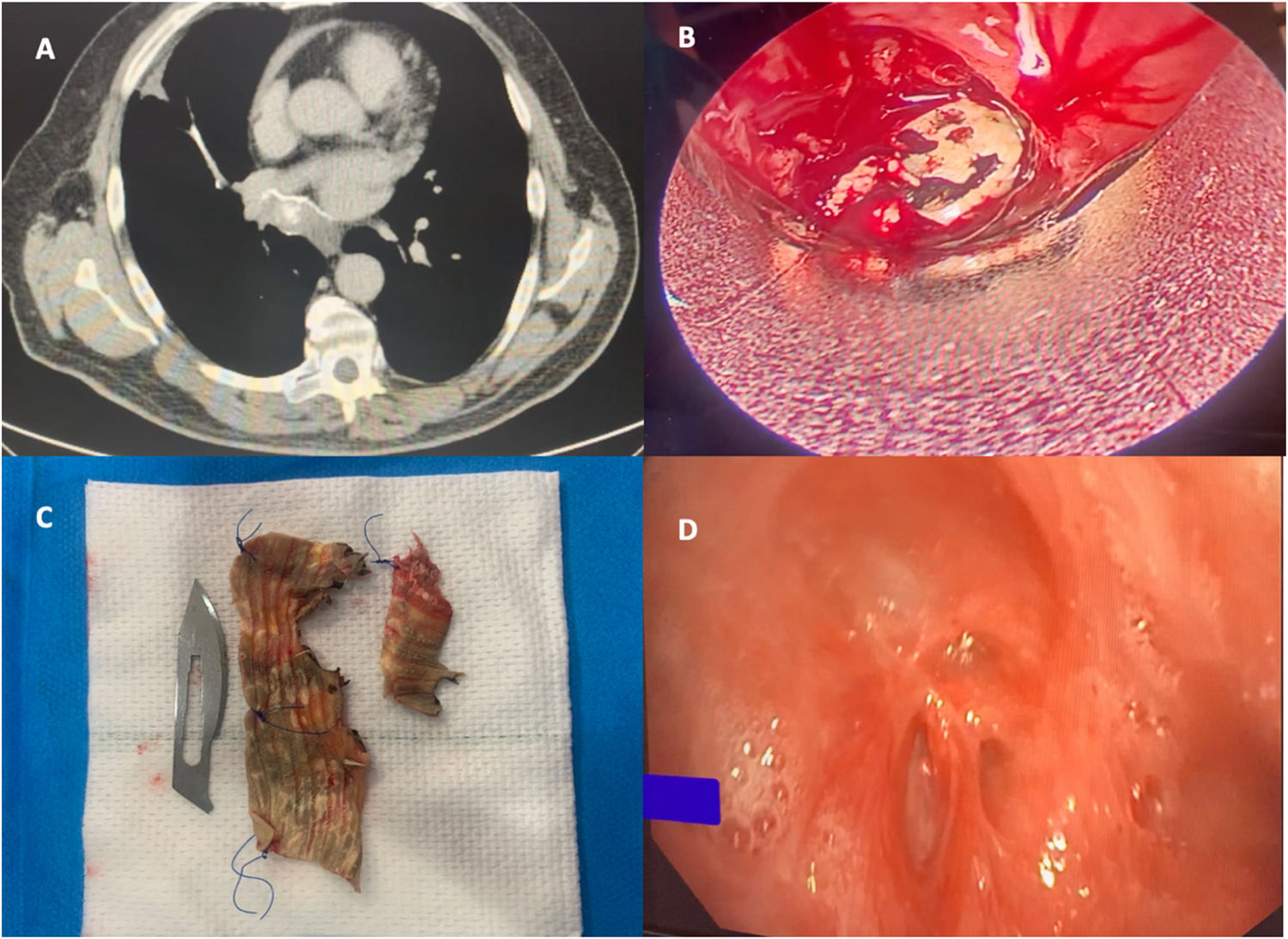
Given his clinical progress and history, a chest CT scan was performed to plan a definitive therapeutic approach. The report was as follows: “Soft tissue formation containing small high-density mass. Finger-like projection of the mass from the intermediate bronchus stump to the lower wall of the right main bronchus toward the lumen” (Fig. 1A). The subsequent follow-up fiberoptic bronchoscopy showed a significant protrusion of prosthetic material from the intermediate bronchus stump, while the upper lobe bronchus remained patent. Several unsuccessful attempts were made to remove the material by fiberoptic bronchoscopy, so rigid bronchoscopy was performed, and the mesh could be cut away and removed (Fig. 1B, C). Subsequent bronchoscopy monitoring was satisfactory and the patient's clinical symptoms resolved completely (Fig. 1D).
The patient is currently being followed up by the hematology department, and no images or clinical evidence of bronchopleural fistula have been observed.
Although this is an extremely rare situation, we must take into account the potential complications that can occur when prosthetic material is used in the mediastinum (infection, migration, tamponade in case of pericardial defects, etc.).
Despite an intensive search, we could not find any similar cases in the published literature, as this is an extremely rare late complication.1,2
The attached video (Annex A) shows the clinical process and the outcome after the procedure.