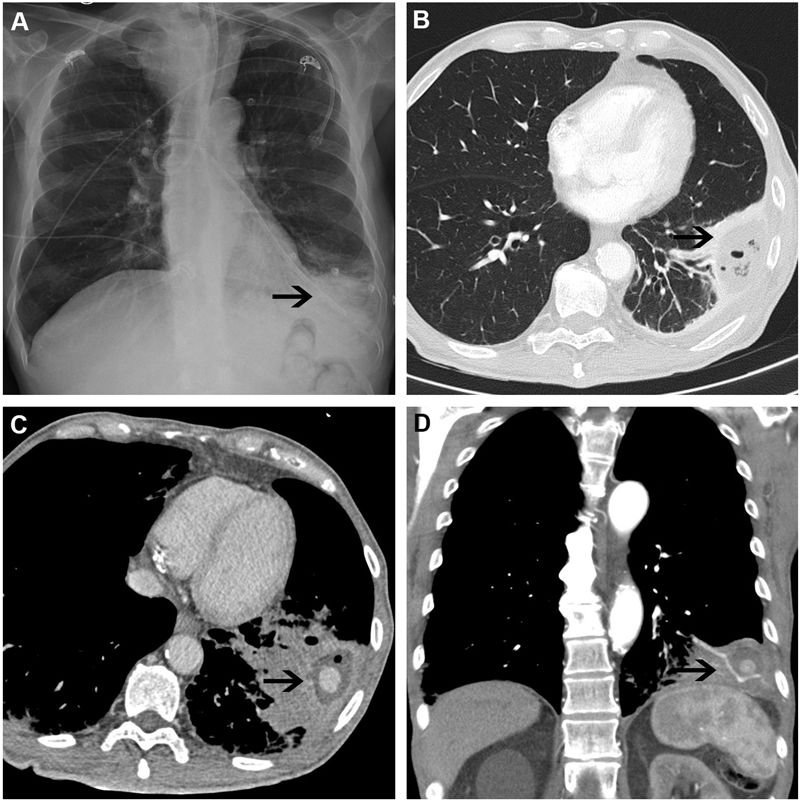
We report the case of a 72-year-old man with oropharyngeal squamous carcinoma treated with chemoradiotherapy, who had a nasogastric tube (NGT) placed due to dysphagia associated with mucositis. After accidental displacement, the NGT was repositioned in the emergency department. The patient presented 24h later with a complaint of dyspnea and left chest pain. The chest X-ray showed the distal tip of the NGT in the left lower lobe (Fig. 1A). The suggested diagnosis was chemical pneumonitis, intravenous antibiotic therapy was started, and he was admitted. During his stay, the chest computed tomography (CT) showed an image suggestive of resolving necrotizing pneumonia (Fig. 1B) and he was discharged with oral antibiotic therapy.
(A) Chest X-ray showing the nasogastric tube (NGT) with distal tip (arrow) in the left lower lung and alveolar infiltrate. (B) Chest CT of the left lower lung showing an area of hypodense consolidation containing air bubbles (arrow) suggestive of necrotizing pneumonia. (C, D) Axial and coronal slices, respectively, of the chest CT showing image of cavitary consolidation in left lower lung (arrow) containing active bleeding.
The patient presented 2 months later with life-threatening hemoptysis. CT angiography showed increased cavitary consolidation and an image of active bleeding: segmental pulmonary artery pseudoaneurysm could not be ruled out (Fig. 1C, D). Left lower lobectomy was performed and he was discharged 3 days later.
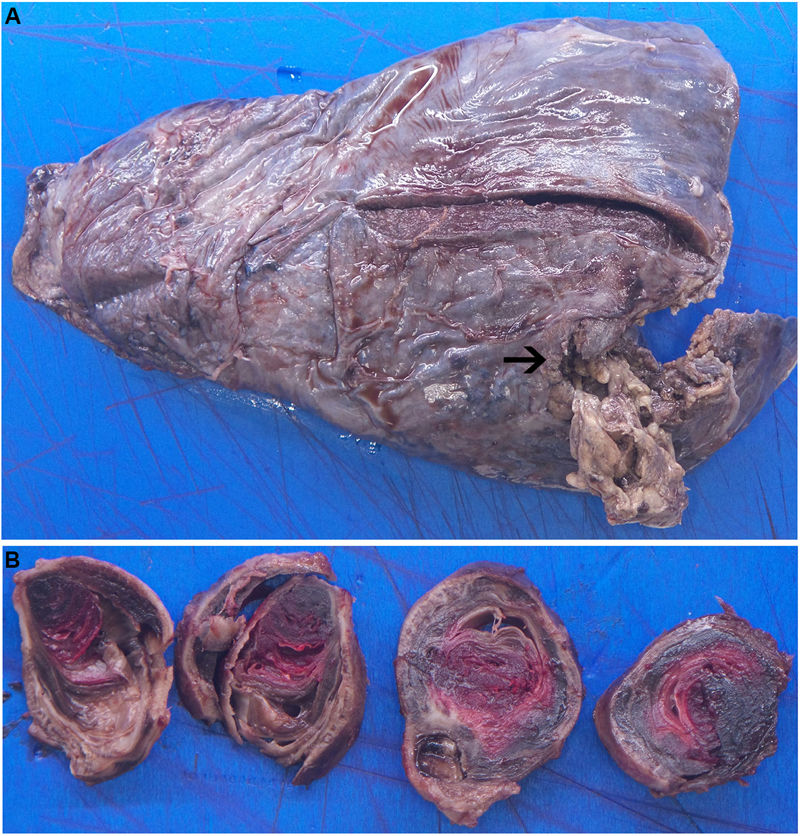
The histopathology study reported acute necrotizing pneumonia with abscess and ulceration of the bronchial wall, associated bleeding, and a foreign-body giant cell reaction (Fig. 2A, B).
Iatrogenic pulmonary artery pseudoaneurysm is a rare entity occasionally associated with the use of intravascular catheters or surgical reconstruction of the pulmonary artery.1 Surgical repair is the appropriate approach in cases that are symptomatic or increasing in size.2