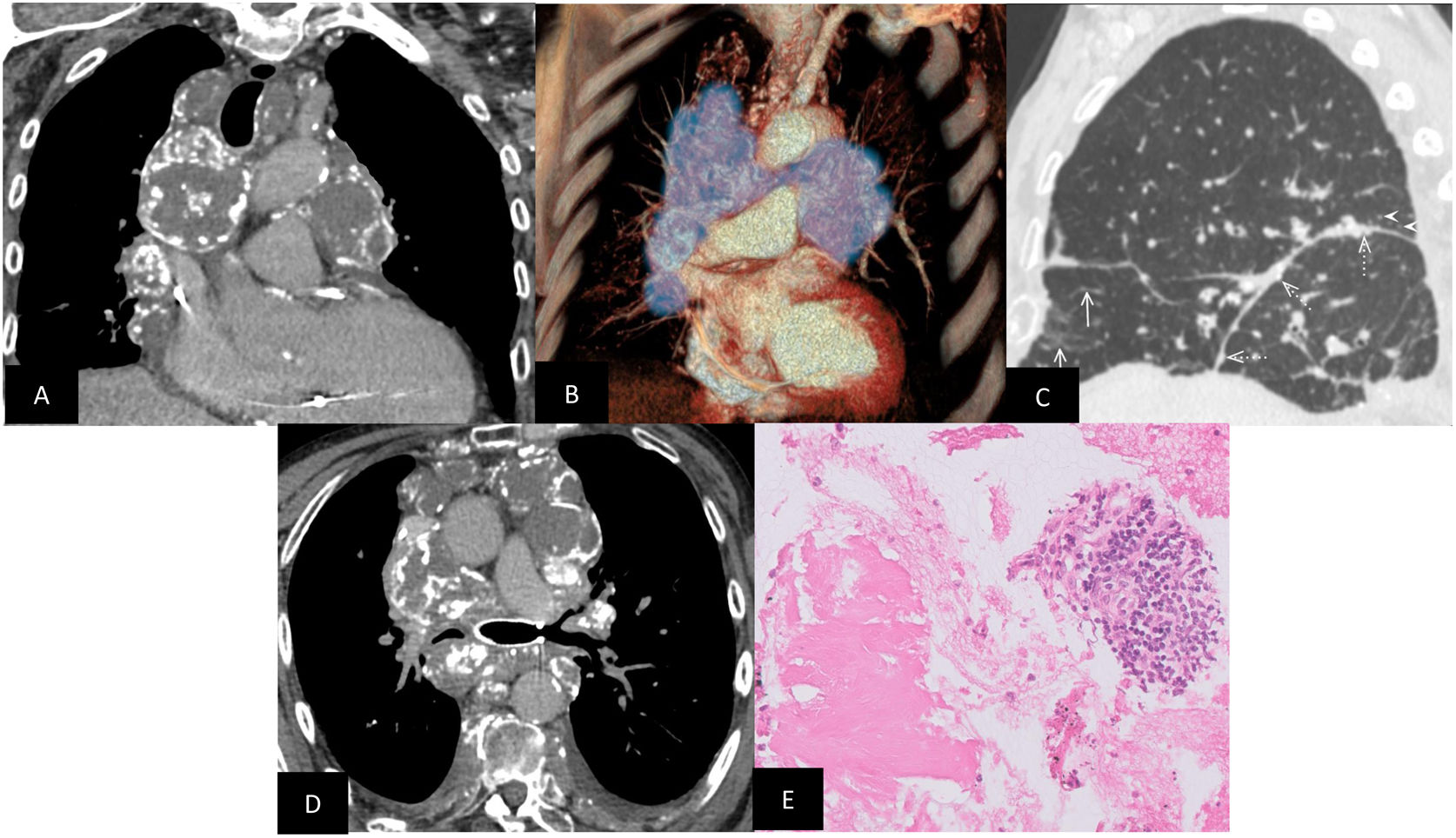
A 68-year-old man with a long-standing history of systemic light-chain (primary, AL) amyloidosis and bronchiectasis, was admitted into hospital repeatedly with shortness of breath, inspiratory stridor and wheeze. Computed tomography scan was performed (Fig. 1). There was no physical obstruction above the level of the vocal cords on bronchoscopy; obtained tissue samples confirmed amyloidosis.
(A) Coronal computed tomography image in soft-tissue windows showed striking peripherally calcified mediastinal and hilar lymphadenopathy. Mediastinal lymphadenopathy is usually a feature of systemic as opposed to localised disease, as demonstrated here. (B) Volume-rendered three-dimensional reconstructions highlight the extent of the lymphadenopathy shaded in blue. (C) Lung windows highlight the varied features of pulmonary parenchymal amyloidosis including septal involvement, in the form of interlobular septal thickening (arrows), parenchymal nodules or amyloidomas (arrowheads), peri-lymphatic calcified nodules (dotted arrows). (D) The patient was offered endobronchial stenting of his left main bronchus, which alleviated the symptoms greatly. (E) Mediastinal lymph node biopsy specimen obtained via endobronchial ultrasound (EBUS) demonstrates acellular deposits which appeared cyanophilic on Papanicolau's stain and eosinophilic on haematoxylin and eosin (H&E) stain. When stained with Congo red, it exhibited apple-green birefringence under polarised light characteristic of amyloidosis (the image was not available for publication).
Amyloidosis is a group of conditions related to extracellular tissue deposition of insoluble amyloid proteins; the classification is based upon the protein structure. There are many clinical forms, which commonly manifest as secondary disease to a range of pathological processes; however, primary and hereditary forms also exist. The radiological features are diverse, often non-specific, sometimes making its diagnosis elusive for the radiologist.1
Systemic AL amyloidosis affects a vast range of organs; the clinically significant deposition sites are the kidneys, heart, and liver. Pulmonary involvement is infrequently encountered and is usually a localised entity.2 Laryngeal, tracheobronchial, parenchymal (diffuse, nodular) and mediastinal/hilar forms exist and may overlap. Pulmonary involvement should be considered in patients suffering from systemic amyloidosis who present with unexplained recurrent pleural effusions and respiratory symptoms such as cough, wheezing and stridor.
FundingNo funding was received for this work.
Competing InterestsAuthors have no competing interests to declare.