Human alveolar echinococcosis (AE) is a rare, life-threatening zoonosis caused by the larvae of Echinococcus multilocularis, a helminth of the class Cestoda. Almost all cases of AE arise in the liver and may spread via the bloodstream to distant organs, including the lungs, brain, and kidneys.1–3 PAE studies in the literature typically comprise case reports, and clinical studies are infrequent.4–7 Lung involvement generally manifests as widespread metastases, and only a small number of cases are suitable for surgical treatment.8–10 Consequently, there is currently no agreement regarding the surgical treatment of PAE. The aim of our study was to investigate the efficacy and feasibility of surgery in the treatment of alveolar echinococcosis, which is endemic in our region. The statement was added in the manuscript. The study protocol was approved by the Institutional Review Board for Human Subjects Research and Ethics Committee (B.30.2.ATA.0.01.00/470, 02Jun2022).
Retrospectively, the study included a total of 13 patients who underwent surgical treatment for PAE between January 2012 and December 2023. All patients were admitted from the Eastern Anatolia region of Turkey and all patients lived in rural areas. The patients comprised 5 males and 8 females, with a mean age of 41.9±12.1 years (range 28–65 years). Of the 11 cases assessed, the Echinococcus IgG ELISA test was positive in eight cases (72.7%) and negative in three cases (27.3%). Furthermore, a histopathological diagnosis of alveolar echinococcus was established in all cases.
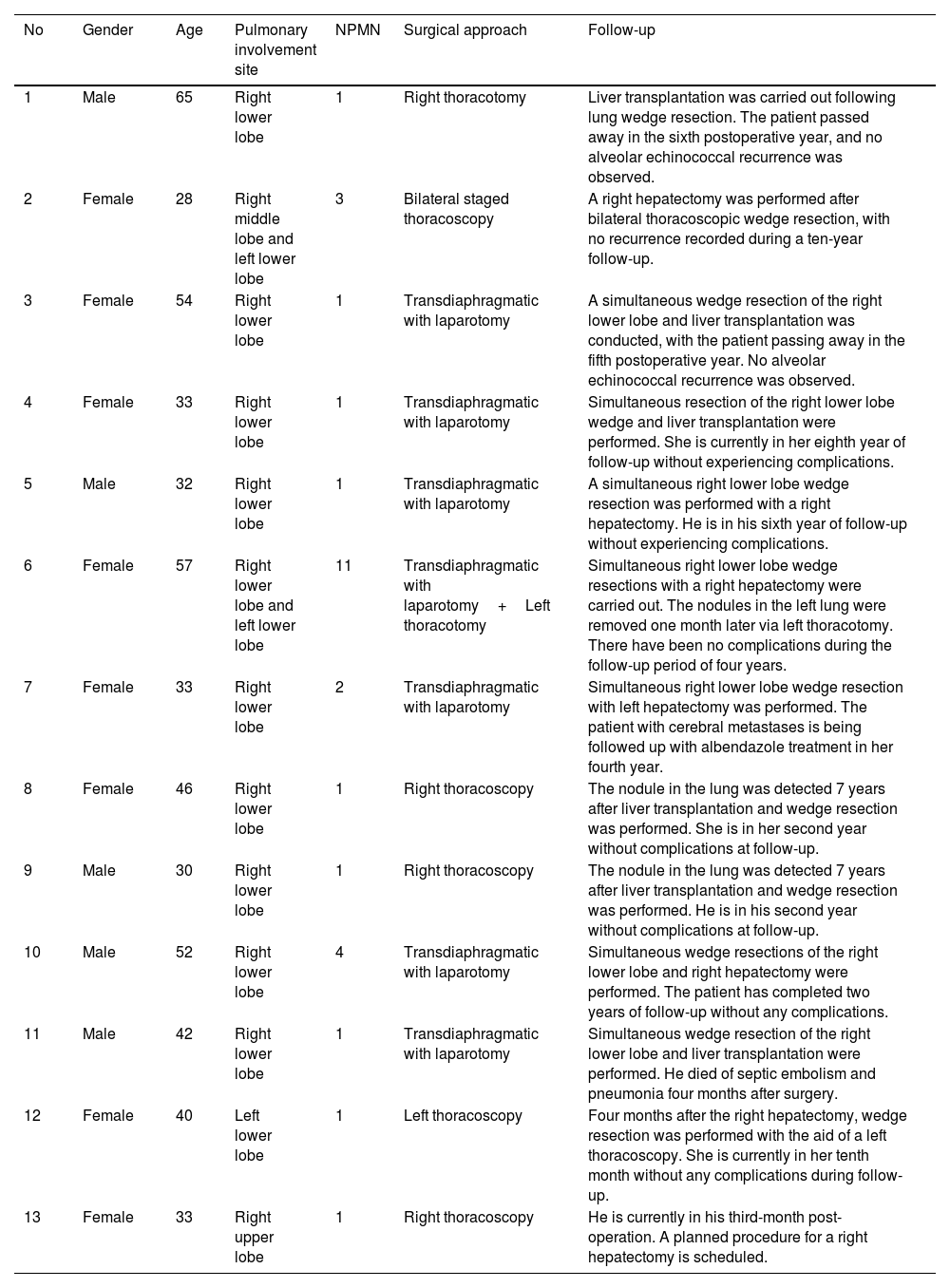
Surgical cases comprised 22.8% (13/57) of all cases of PAE. Of these, 84.6% (eleven cases) had involvement limited to one lung, while two cases (15.4%) exhibited involvement in both lungs. In the affected cases, involvement was present in the lower lobe of the right lung in 66.7% (10 cases), in the lower lobe of the left lung in 20% (three cases), and in the upper and middle lobes of the right lung in a single case each (Table 1). While 11 (84.6%) of the cases were asymptomatic with regards to the respiratory system, two (15.4%) cases exhibited coughing symptoms.
Patient characteristics and treatment approach.
| No | Gender | Age | Pulmonary involvement site | NPMN | Surgical approach | Follow-up |
|---|---|---|---|---|---|---|
| 1 | Male | 65 | Right lower lobe | 1 | Right thoracotomy | Liver transplantation was carried out following lung wedge resection. The patient passed away in the sixth postoperative year, and no alveolar echinococcal recurrence was observed. |
| 2 | Female | 28 | Right middle lobe and left lower lobe | 3 | Bilateral staged thoracoscopy | A right hepatectomy was performed after bilateral thoracoscopic wedge resection, with no recurrence recorded during a ten-year follow-up. |
| 3 | Female | 54 | Right lower lobe | 1 | Transdiaphragmatic with laparotomy | A simultaneous wedge resection of the right lower lobe and liver transplantation was conducted, with the patient passing away in the fifth postoperative year. No alveolar echinococcal recurrence was observed. |
| 4 | Female | 33 | Right lower lobe | 1 | Transdiaphragmatic with laparotomy | Simultaneous resection of the right lower lobe wedge and liver transplantation were performed. She is currently in her eighth year of follow-up without experiencing complications. |
| 5 | Male | 32 | Right lower lobe | 1 | Transdiaphragmatic with laparotomy | A simultaneous right lower lobe wedge resection was performed with a right hepatectomy. He is in his sixth year of follow-up without experiencing complications. |
| 6 | Female | 57 | Right lower lobe and left lower lobe | 11 | Transdiaphragmatic with laparotomy+Left thoracotomy | Simultaneous right lower lobe wedge resections with a right hepatectomy were carried out. The nodules in the left lung were removed one month later via left thoracotomy. There have been no complications during the follow-up period of four years. |
| 7 | Female | 33 | Right lower lobe | 2 | Transdiaphragmatic with laparotomy | Simultaneous right lower lobe wedge resection with left hepatectomy was performed. The patient with cerebral metastases is being followed up with albendazole treatment in her fourth year. |
| 8 | Female | 46 | Right lower lobe | 1 | Right thoracoscopy | The nodule in the lung was detected 7 years after liver transplantation and wedge resection was performed. She is in her second year without complications at follow-up. |
| 9 | Male | 30 | Right lower lobe | 1 | Right thoracoscopy | The nodule in the lung was detected 7 years after liver transplantation and wedge resection was performed. He is in his second year without complications at follow-up. |
| 10 | Male | 52 | Right lower lobe | 4 | Transdiaphragmatic with laparotomy | Simultaneous wedge resections of the right lower lobe and right hepatectomy were performed. The patient has completed two years of follow-up without any complications. |
| 11 | Male | 42 | Right lower lobe | 1 | Transdiaphragmatic with laparotomy | Simultaneous wedge resection of the right lower lobe and liver transplantation were performed. He died of septic embolism and pneumonia four months after surgery. |
| 12 | Female | 40 | Left lower lobe | 1 | Left thoracoscopy | Four months after the right hepatectomy, wedge resection was performed with the aid of a left thoracoscopy. She is currently in her tenth month without any complications during follow-up. |
| 13 | Female | 33 | Right upper lobe | 1 | Right thoracoscopy | He is currently in his third-month post-operation. A planned procedure for a right hepatectomy is scheduled. |
NPMN: number of pulmonary metastatic nodules.
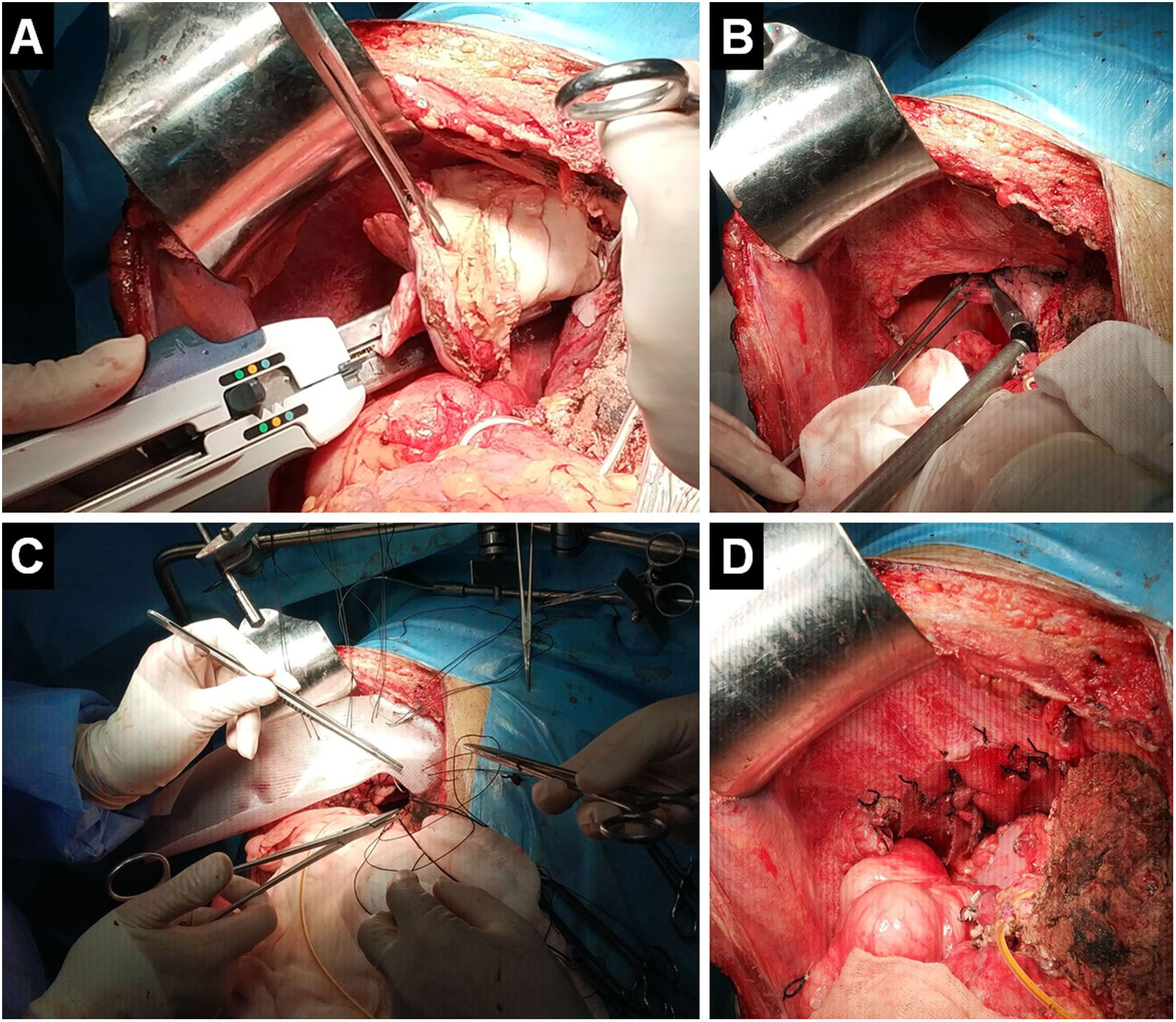
The liver was the primary affected organ in all cases. Regarding the liver, six cases underwent liver transplantation, six underwent hepatectomy, and one case is awaiting hepatectomy. Seven cases underwent diaphragmatic resection and reconstruction through laparotomy using a transdiaphragmatic approach due to diaphragmatic invasion. Among these cases, four underwent hepatectomy, while three received surgical treatment for nodules in the right lung during liver transplantation. One of the two cases with bilateral involvement underwent consecutive bilateral thoracoscopy, whereas in the second case, a transdiaphragmatic approach was carried out through laparotomy for the right lung and thoracotomy for the left lung. Four out of the other five cases were approached thoracoscopically, with one undergoing thoracotomy. In all cases, wedge resection was used for PAE lesion excision. A total of twenty-five metastatic lesions were removed from the lungs through wedge resections (Fig. 1). None of the cases yielded any postoperative complications or mortalities.
The images from the patient number 10 demonstrate intra-abdominal resection of the diaphragm and affected lung during the same session with right hepatectomy (A), transdiaphragmatic excision of four metastatic pulmonary nodules (B), reconstruction of the diaphragmatic defect after resection with an 8cm×5cm double mesh (C) and closure of the diaphragmatic defect after the procedure (D).
The patient with bilateral involvement was intervened one month after hepatectomy for the left lung. Lung surgery was performed four months after hepatectomy in one case. Before the liver, metastases in the lungs were treated in three cases. A metastatic lesion was detected in the right lung seven years after liver transplantation in two cases, and wedge resection was carried out. One case revealed cerebral metastasis during hepatectomy, and this case is being followed up with albendazole treatment in the fourth year. Since 2010, although intermittent treatment is not recommended, in cases where pulmonary wedge resection is conducted, patients are treated with albendazole (10mg/kg/day) for three months each year for two years to avoid recurrence. Three patients who underwent liver transplantation died during the follow-up period (fourth month, fifth year, and sixth year). However, during the average 46.5±36.4 months of follow-up (ranging from 3 to 120 months) after pulmonary metastasectomy, none of the cases exhibited any lung or systemic recurrence.
The treatment guidelines for AE established by the WHO Informal Working Group on Echinococcosis (IWGE) suggest that surgical removal of parasitic foci should be the primary option for patients with operable disease, followed by a limited course of chemotherapy.11,17 Hepatectomy, if complete resection of lesions at the origin site can be achieved and if liver function is well preserved, is the sole curative therapy for AE.12–14 [Unfortunately, a curative resection is not possible for around 70% of patients when diagnosed with AE, resulting in only a resection rate of 20–40%.14,15 Liver resection is the safest intervention for AE, and once the lesions are completely removed, a 2-year course of albendazole is recommended.14,15
If a parasitic lesion cannot be removed through hepatectomy, liver transplantation may be considered. However, it is important to note that re-growth or recurrence of lesions caused by immunosuppression after liver transplantation is a significant issue.15 Therefore, it is not advisable to undergo liver transplantation if metastases are present in other organs, as the mandatory use of immunosuppressive drugs creates favourable conditions for metacestode development.16,17 However, Zavoikin et al.18 demonstrated that liver transplantation, in conjunction with continuous albendazole treatment, extended patients’ lifespans both in the absence and presence of metastases. Additionally, our study indicates that liver transplantation and the removal of lung metastases significantly contribute to the survival of patients with lung metastases. Therefore, we posit that the presence of removable lung metastases should not be deemed an absolute contraindication for liver transplantation. Nonetheless, our study reveals the occurrence of pulmonary metastases in two cases, seven years post-liver transplantation, emphasizing the necessity for extending albendazole administration in transplant patients.
We think that the treatment of PAE should be evaluated together with the lesion in the liver. Surgical treatment should be the first choice in cases where pulmonary metastases are not extensive. In such cases, the lung parenchyma should be conserved as much as possible while removing metastatic lesions. Unfortunately, a majority of cases are unsuitable for surgery due to extensive pulmonary involvement. Our study found that surgical treatment was only possible in 22.8% of patients diagnosed with PAE.
The study has several limitations. First, the study was retrospective. Secondly, the number of cases is low. Another factor is the lack of sufficient data to compare surgical techniques.
It is important to evaluate patients with hepatic AE for PAE involvement. These cases should be approached as in lung metastasis of other tumours. In situations where there is diaphragmatic involvement, lung metastases can be removed transdiaphragmatically through laparotomy during liver transplantation or hepatectomy while preserving the parenchyma as much as possible. In all other cases, transthoracic minimally invasive approaches can be employed. To prevent recurrence, postoperative albendazole treatment should be administered.
Data availabilityThe data underlying this article will be shared on reasonable request to the corresponding author.
Financial supportThe authors received no financial support for the research and/or authorship of this article.
Conflict of interestThe authors declare that they have no conflict of interest in the publication of this article.