According to the most recent clinical practice guidelines, pulmonary rehabilitation (PR) has demonstrated high level of evidence as a key component in the management of people with bronchiectasis.1,2 Although the implementation of PR depends on local resources, health-system organization, multidisciplinarity, and individual patient needs,3 the role of the respiratory physiotherapists in those programs is crucial. Their intervention should be centered on airway clearance techniques, exercise training, promotion of physical activity and education on bronchiectasis self-management.3
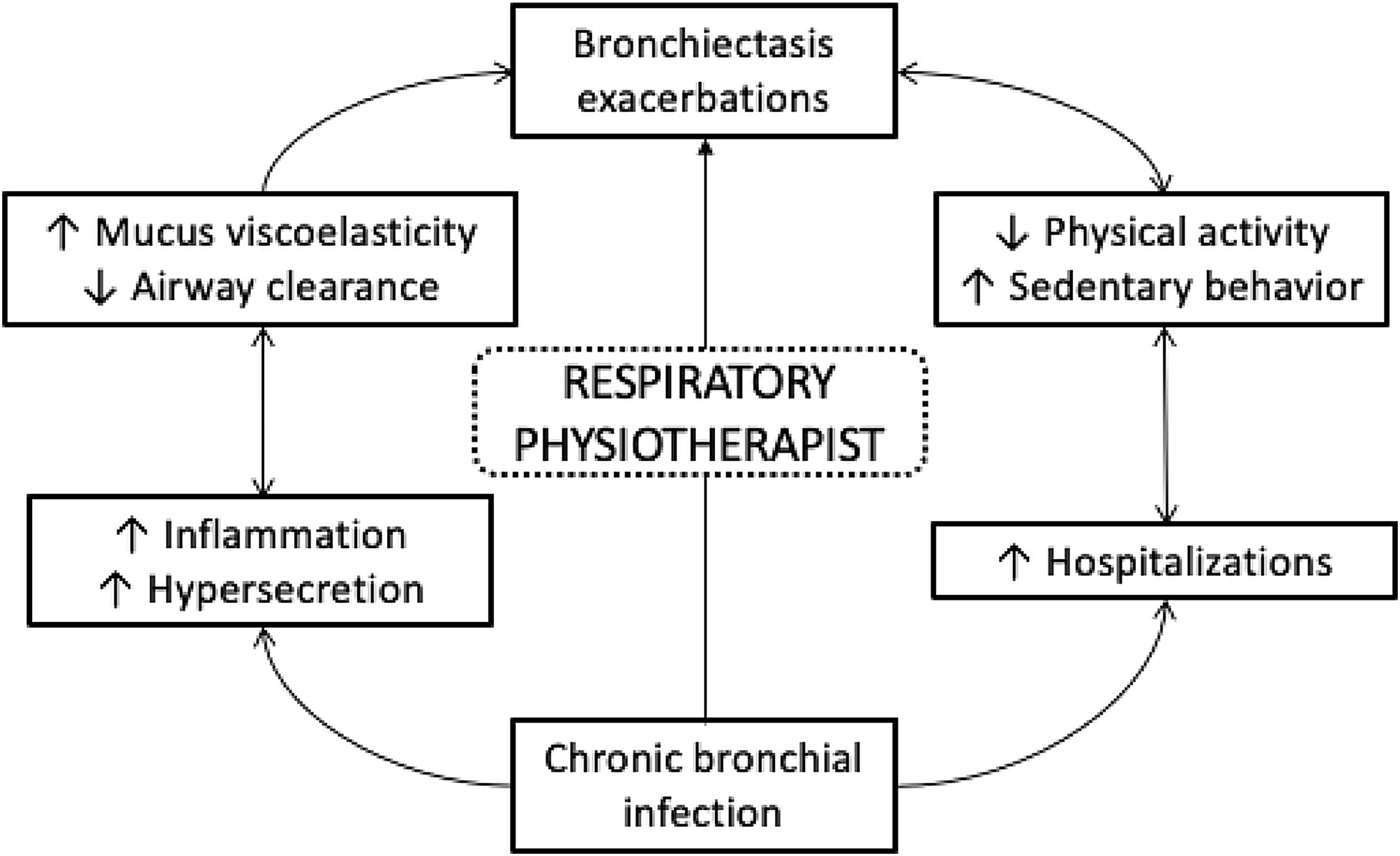
One of the most prevalent and important consequences of bronchiectasis is sputum production, inflammation and bronchial infection which contributes to airway clearance impairment. These respiratory changes together with repetitive acute exacerbations of bronchiectasis contribute to impaired airway clearance. Furthermore, physical inactivity and high sedentary behavior as a consequence of infection may also enhance the number of mild and severe exacerbations requiring hospitalization. The contribution of each of these pathophysiological processes are outlined in Fig. 1 and are a guide to non-pharmacological management for people with bronchiectasis.
To address respiratory symptoms, airway clearance techniques are considered as a relevant part of the treatment plan throughout the disease trajectory, from diagnosis, in exacerbated and stable states, in deteriorating patients, and those with frequent exacerbations.1 These techniques should be taught and individually prescribed by a respiratory physiotherapist, adopting a patient-centered approach, with the execution of these treatments reviewed periodically.
Additionally, as a result of respiratory symptoms and hospitalizations, people with bronchiectasis may have impaired exercise capacity. The effects of exercise training in bronchiectasis have been widely studied with the recommendation for participation supported by high quality evidence.1,2 Those who participate in a PR program and undertake regular exercise benefit from an increased exercise capacity, improved quality of life and longer time to first exacerbation.4 The duration of programs ideally has a length of minimum 8 weeks, with 2–3 sessions per week, of 30–45min of aerobic training.5 These programs commonly combine the aerobic exercise with upper and lower limb strength training and may also include inspiratory muscle training which could enhance the maintenance of the training effect.1 Those with bronchiectasis respond in a similar manner and magnitude to exercise training to people with chronic obstructive pulmonary disease (COPD).6 The benefits of exercise training and inclusion of a regular exercise regimen within daily life following completion of a PR program in people with bronchiectasis should be reinforced.
It is noteworthy that physical inactivity and higher sedentary behaviors are global, preventable, and crucial problems due to their influence on health. The association between those behaviors and chronic respiratory conditions (e.g., patients with COPD) is significant, with evidence consistently showing that people with COPD who are more inactive and/or who have a higher sedentary behavior have a higher number of hospitalizations, worse quality of life and higher mortality rates than those who are more active or have less sedentary behavior.7,8 According to the Global Initiative for Chronic Obstructive Lung Disease Report,9 monitoring physical activity and sedentary behavior through accelerometers or multi-sensors, and applying interventions to encourage more active behavior, should be included in clinical practice of those with COPD.
Although research in this field in bronchiectasis is still scarce, some interesting results have emerged in recent years. Both people with bronchiectasis and COPD have lower levels of physical activity compared to healthy individuals, but those with bronchiectasis are a little more active than people with COPD.10 The association of physical inactivity and its impact on clinical outcomes appear to be quite similar in both populations. People with bronchiectasis who are more active have better lung function, exercise capacity and less dyspnea perception than those who are less active in their daily life.11 Physical activity levels and sedentary behavior were associated with long-term clinical outcomes; those with low levels of physical activity (≤6290 steps per day) and high sedentary behavior (≥7.8h per day) had a higher risk of hospitalization after 1-year of follow-up compared to those who were more active and less sedentary.12
Understanding why people are or not physically active is one of the most difficult questions to answer. Only one study that investigated the determinants of inactivity and a higher sedentary behavior in bronchiectasis13 found that the number of exacerbations was associated with a higher inactivity and higher sedentary behavior after 1-year of follow-up. When compared both people with COPD or bronchiectasis behave similarly as the number of exacerbations, independent of severity, are also associated with a higher inactivity in COPD.14 However, physical activity is a complex behavior and its study, especially in chronic respiratory disease such as bronchiectasis, should be based on a broad model which comprises all the determinants for this behavior. To illustrate this, Bauman et al. in 201215 proposed an ecological model that included individual, interpersonal, environmental, regional, and global determinants of physical activity. To date, research in chronic respiratory conditions has been centered mostly in biological and clinical determinants of physical activity, and into a lesser extent interpersonal determinants. The scientific community should center further research in the understanding of these comprehensive models in order to implement appropriate interventions to increase physical activity and reduce sedentary behaviors in people with chronic respiratory conditions, including bronchiectasis.
In summary, those with bronchiectasis should have access to PR programs to obtain optimal disease management,1 and it is essential to offer exercise training, airway clearance techniques and implementation of an active lifestyle to reduce the frequency of acute exacerbations. The respiratory physiotherapist has the knowledge and skills to assess and treat people with bronchiectasis and this mix of interventions could have direct implications in the prognosis of the disease.