Interstitial lung diseases (ILD) have different causes, treatments, and courses. One ILD subgroup that progresses over time despite appropriate treatment is called progressive pulmonary fibrosis (PPF).1 A highly variable proportion of ILD patients develop PPF: between 3% and 63%, depending on the entity.2 No international agreement on the definition of PPF was available until an international group of respiratory societies recently published a consensus document.1 This document defined PPF as the presence of at least 2 of the following criteria occurring within the last year with no alternative explanation: (1) worsening respiratory symptoms (cough and/or dyspnea); (2) decline in forced vital capacity (FVC, % absolute)≥5% and/or decline in diffusing capacity of the lungs for carbon monoxide≥10% (% absolute); (3) New or increased extent of fibrosis on high-resolution computed tomography. Previously, the most commonly used definition of progression was that of the INBUILD study, which included relative FVC decline among its criteria. These criteria have been widely discussed, and we would like to focus on the definition, differences, and implications of absolute or relative FVC decline as variables for defining progression.
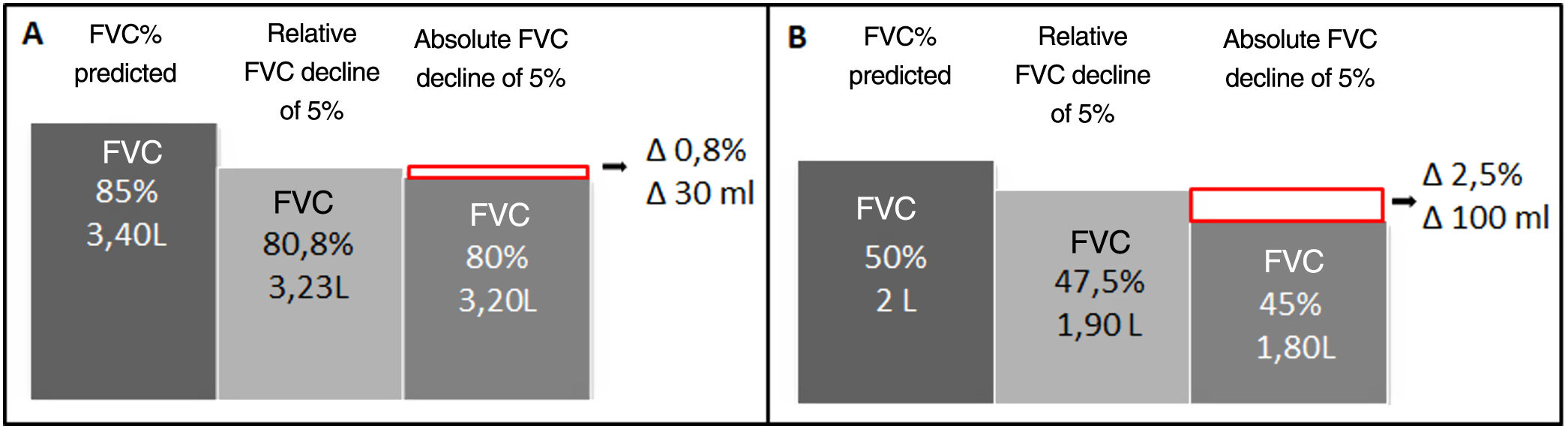
FVC decline is a criterion for progression and a predictor of mortality in fibrotic ILD.2 Absolute decline (as a percentage) is calculated as follows: baseline FVC – final FVC; while relative decline is (baseline FVC – final FVC)/baseline FVC.3 Both measurements are similar when the patient's FVC is preserved but differ increasingly as FVC declines (Fig. 1). The more severe baseline FVC, the greater the risk of identifying random or non-clinically significant fluctuations using the relative method.3 The method used will affect the design and outcomes of clinical trials. When the relative method is used to calculate a ≥5% decline in FVC, smaller sample sizes are needed.3 A retrospective study showed that the percentage of patients with PPF differs depending on the definition of progression used.4 The choice of method is also associated with earlier detection of progression (the relative method is more sensitive, despite some loss of specificity), which in turn affects the indication for antifibrotic treatment and patient prognosis. Finally, in patients with idiopathic pulmonary fibrosis, the minimum clinically significant difference in the percentage of absolute decrease in FVC has been estimated at 2%-6%.5 This value in patients with PPF is unknown. Studies evaluating the clinically significant minimum difference in relative and absolute decline of FVC in patients with PPF would therefore be of value.
Comparison of a 5% decline in FVC in absolute and relative terms according to the baseline FVC of a theoretical patient: (A) patient with preserved baseline FVC and (B) patient with decreased baseline FVC. As baseline FVC declines, the difference between the relative and absolute percentage value increases. The relative method is more sensitive for detecting decline and this parameter is more marked in patients with reduced baseline FVC values. Absolute FVCdecline=baseline FVC−final FVC; relative decline: (baseline FVC−final FVC)/baseline FVC; FVC: forced vital capacity; L: liters; Δ: Delta of change between a relative and absolute FVC decline of 5%.
In conclusion, changes in the criteria used to define PPF may have prognostic and therapeutic implications. The relative method is useful for the early detection of decline but is more susceptible to random fluctuations that lack clinical relevance.
FundingWe have no sources of funding for the development of the manuscript.
Conflict of interestsWe have no conflict of interests related directly or indirectly to the contents of this paper.