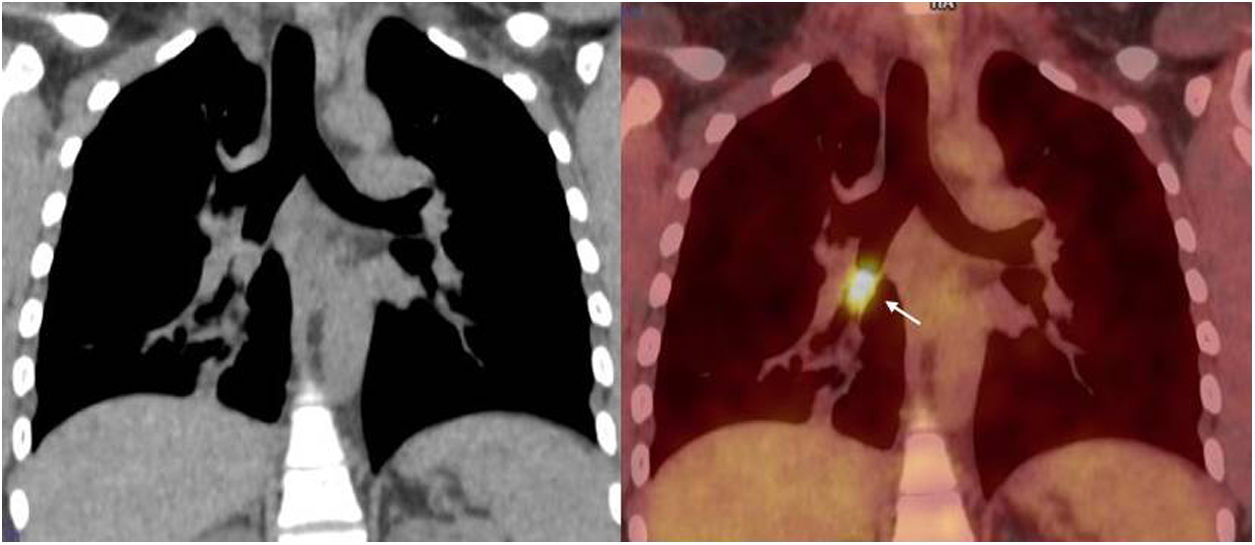
Oncocytoma of the lung is very rare. This type of tumour is more common at other sites such as the salivary or thyroid glands or the kidneys.1 In the lung, it is diagnosed in asymptomatic patients after the radiological finding of a solitary pulmonary nodule.2 What makes our case distinct is the fact that it was a 35-year-old woman with symptoms mimicking bronchial asthma in whom the definitive diagnosis of oncocytoma of the lung was reached by bronchial biopsy, when in most cases the diagnosis is made following surgical excision. The this was a 35-year-old woman with no relevant medical history admitted to our unit because of chronic cough with whitish expectoration and wheezing, with no pyrexia or other symptoms. The patient reported a year and a half of episodes of cough, dyspnoea and wheezing, which improved with antibiotic therapy, oral corticosteroids and inhalation therapy. As bronchial asthma had been suspected, the week before her admission the patient had spirometry tests at another centre, which were normal, as well as a chest computed tomography (CT) scan, which showed complete stenosis of the intermediate bronchus. Her blood test identified leucocytosis of 17.72×103/μl (80% neutrophils) without other relevant findings, and chest X-ray on admission was suggestive of consolidation in the right lower lobe (RLL). After reviewing the chest CT and confirming the bronchial stenosis, bronchoscopy identified a lesion with an exophytic appearance and smooth surface at the entrance to the intermediate bronchus, occluding 90% of its lumen. Tumour biopsies were taken and the study for other lesions was completed with a CT scan of the abdomen and pelvis, which ruled out extra-thoracic lesions. Positron emission tomography and CT scans were requested of the chest (Fig. 1) and body, which showed a metabolic increase suggestive of malignancy in the intermediate bronchus, with no distant metastasis. The pathology study of the bronchial biopsy found an infiltration by a neoplasm made up of elements of broad, eosinophilic and granular cytoplasm, with rounded monomorphic nuclei, often with prominent central nucleoli, arranged in sheets or in the form of cord-like structures. There was very little mitotic activity (1mitosis/2mm2) and the proliferation rate, determined by immunostaining for ki67, was low (5%). Immunohistochemistry study was negative for neuroendocrine markers (chromogranin A, synaptophysin, CD56), positive for cytokeratin AE1/AE3 and p63 and for PTHA in some cell groups and high intensity for anti-mitochondrial antibodies. Based on these findings, our hospital's pathologist concluded that this was oncocytoma of the lung. The patient was referred to the Thoracic Surgery Department, where she underwent lobectomy of the right middle and lower lobes. The pathological report on the surgical specimen confirmed the previous diagnosis of oncocytoma of the lung, without invasion of enlarged peribronchial lymph nodes. At the time of writing the patient remains asymptomatic and has shown no signs of recurrence.
Oncocytoma is rare, representing less than 1% of all lung tumours and it is more common at other sites, such as the salivary or thyroid glands or the kidneys.1 It is a benign tumour composed of oncocytes, cells of epithelial origin with numerous cytoplasmic eosinophilic granules, a vesicular nucleus and prominent nucleolus. This tumour originates in the mucosa and/or myoepithelium of the collecting ducts of peribronchial glands in the respiratory tract,1,3 and the tumour cells are uniform in size, with very low degrees of atypia and mitosis and generally without local invasion or distant metastasis.3,4 Tumours most commonly responsible for mistaken histological diagnoses are the oncocytic carcinoid tumour and acinic cell carcinoma of the saliva glands.5–8 The oncocytic carcinoid contains neuroendocrine granules, with positive staining for CD56, chromogranin A and synaptophysin. Another type of tumour which can lead to confusion is acinic cell carcinoma of the saliva glands, as one of the patterns it presents is oncocytic, with immunohistochemistry being the key to diagnosis (intense positive PAS staining).6–8 Such was the case with the first “oncocytoma of the lung” described by Black in 19691 which, in later reviews, given its histological characteristics, appeared to be an acinic cell carcinoma.
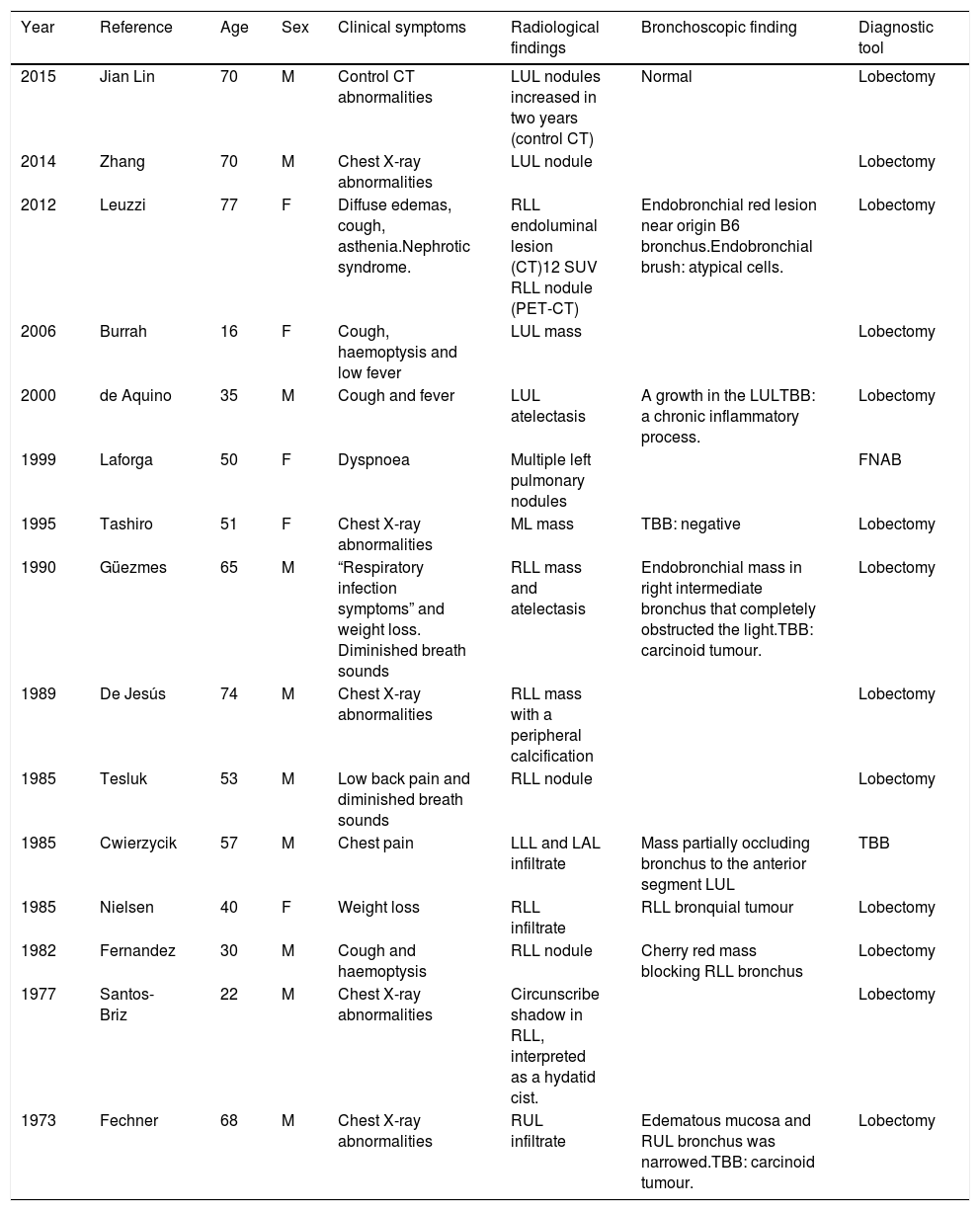
Oncocytoma of the lung tends to occur in middle-aged men.6 Of the fourteen cases reported to date, nine were in men and five in women, with a mean age of 50 years (range 16–74). Oncocytoma of the lung is usually discovered in asymptomatic patients as a coincidental finding in the form of nodules, masses or pulmonary infiltrates when the patient is undergoing radiological tests for other reasons.2 In some cases, as in our patient, oncocytomas can cause partial or complete bronchial obstruction, giving rise to cough, dyspnoea, haemoptysis and chest pain.3,6–9 Although oncocytomas of the lung are generally localised tumours, the case described by Tashiro et al.10 had focal growth, and the case reported by Nielsen5 had evidence of invasion of enlarged peribronchial lymph nodes. Nevertheless, there are no published cases with evidence of distant metastasis.1,3 The definitive diagnosis of oncocytoma of the lung is usually made after surgical excision of the lesion.9 Out of all the published cases of oncocytoma of the lung, eleven needed pulmonary lobectomy and subsequent study of the surgical specimen to reach a diagnosis. Of these, bronchoscopy was previously performed in six patients, but bronchial biopsy was negative or they were misdiagnosed as carcinoid tumours. In the case described by Laforga,11 the diagnosis of oncocytoma of the lung was obtained by transthoracic fine-needle aspiration biopsy, while diagnosis by bronchoscopy with bronchial biopsy was only achieved in two cases, that reported by Cwierzyk et al.6 and ours. It is always important to rule out that lung lesions are metastases from oncocytic carcinomas of the adrenal or thyroid glands or kidneys. In renal metastases, there will be a sinusoidal vascular pattern, variable amounts of clear cells and positive immunohistochemical staining for vimentin, while in thyroid metastases, there will be a papillary or follicular pattern with colloid and positive staining for thyroglobulin. The treatment of oncocytoma of the lung is surgical by lobectomy of the affected bronchus.7,8,12–14 They are several reasons why surgical resection was performed in our case. First, the approach was surgical in every article published to date. Second, There were two published cases in which local infiltration at the submucosal level and presence of tumour component in lymph nodes have been observed.5,10 Third, for the histological similarity with the carcinoid tumour. Finally, the bronchoscopic approach to endobronchial tumours is not available in our hospital. Despite being a benign tumour, follow-up should be prolonged to rule out recurrence or metastases. At the time of writing, since 1973 there has been no evidence of tumour recurrence in any of the cases of oncocytoma of the lung, our patient included (Table 1). Oncocytoma of the lung has generally been described in asymptomatic middle-aged men, but it can occur in women, and with symptoms of bronchial obstruction mimicking bronchial asthma. Of the fourteen reported cases of oncocytoma of the lung, including our patient, most have required surgical resection for the definitive diagnosis. We have described a second case of bronchial oncocytoma detected by CT and diagnosed by bronchial biopsy, which is very unusual.
Summary of pulmonary oncocytoma cases reported since 1973.
| Year | Reference | Age | Sex | Clinical symptoms | Radiological findings | Bronchoscopic finding | Diagnostic tool |
|---|---|---|---|---|---|---|---|
| 2015 | Jian Lin | 70 | M | Control CT abnormalities | LUL nodules increased in two years (control CT) | Normal | Lobectomy |
| 2014 | Zhang | 70 | M | Chest X-ray abnormalities | LUL nodule | Lobectomy | |
| 2012 | Leuzzi | 77 | F | Diffuse edemas, cough, asthenia.Nephrotic syndrome. | RLL endoluminal lesion (CT)12 SUV RLL nodule (PET-CT) | Endobronchial red lesion near origin B6 bronchus.Endobronchial brush: atypical cells. | Lobectomy |
| 2006 | Burrah | 16 | F | Cough, haemoptysis and low fever | LUL mass | Lobectomy | |
| 2000 | de Aquino | 35 | M | Cough and fever | LUL atelectasis | A growth in the LULTBB: a chronic inflammatory process. | Lobectomy |
| 1999 | Laforga | 50 | F | Dyspnoea | Multiple left pulmonary nodules | FNAB | |
| 1995 | Tashiro | 51 | F | Chest X-ray abnormalities | ML mass | TBB: negative | Lobectomy |
| 1990 | Güezmes | 65 | M | “Respiratory infection symptoms” and weight loss. Diminished breath sounds | RLL mass and atelectasis | Endobronchial mass in right intermediate bronchus that completely obstructed the light.TBB: carcinoid tumour. | Lobectomy |
| 1989 | De Jesús | 74 | M | Chest X-ray abnormalities | RLL mass with a peripheral calcification | Lobectomy | |
| 1985 | Tesluk | 53 | M | Low back pain and diminished breath sounds | RLL nodule | Lobectomy | |
| 1985 | Cwierzycik | 57 | M | Chest pain | LLL and LAL infiltrate | Mass partially occluding bronchus to the anterior segment LUL | TBB |
| 1985 | Nielsen | 40 | F | Weight loss | RLL infiltrate | RLL bronquial tumour | Lobectomy |
| 1982 | Fernandez | 30 | M | Cough and haemoptysis | RLL nodule | Cherry red mass blocking RLL bronchus | Lobectomy |
| 1977 | Santos-Briz | 22 | M | Chest X-ray abnormalities | Circunscribe shadow in RLL, interpreted as a hydatid cist. | Lobectomy | |
| 1973 | Fechner | 68 | M | Chest X-ray abnormalities | RUL infiltrate | Edematous mucosa and RUL bronchus was narrowed.TBB: carcinoid tumour. | Lobectomy |
M, male; F, female; LUL, left upper lobe; ML, middle lobe; RLL, right lower lobe; LLL, left lower lobe; RAL, right upper lobe; CT, computed tomography; PET-CT, positron emission tomography-computed tomography; TBB, transbronchial biopsy; FNAB, fine-needle aspiration biopsy.
The authors have no conflicts of interest to declare.