Blunt thoracic trauma is ranked third among the most common types of trauma, and is the second cause of traumatic death after head injury.1 The mechanisms of injury range from high-impact chest wall trauma to low-energy ground level falls in the elderly.2,3 Rib fractures are the most common injury among patients requiring admission to trauma care units.4 Numerous studies have attempted to identify high-risk patients that are likely to experience serious complications.5 Patients with multiple rib fractures have poorer outcomes, this is particularly true in elderly patients, who experience disproportionately high morbidity rates after chest wall injuries.6 Several trauma score predictors have been described to predict the outcome of these patients which included the presence of organ injuries. However, the value of these systems in subjects with minor chest trauma is still unclear.7
For all the above reasons, it was hypothesized that it is possible to predict the hospitalization stay and need for admission in an intensive care unit (ICU), and potential complications, in chest trauma patients with rib fractures. Accordingly, the main objective of this study was to identify independent factors for prolonged hospitalization and ICU admission.
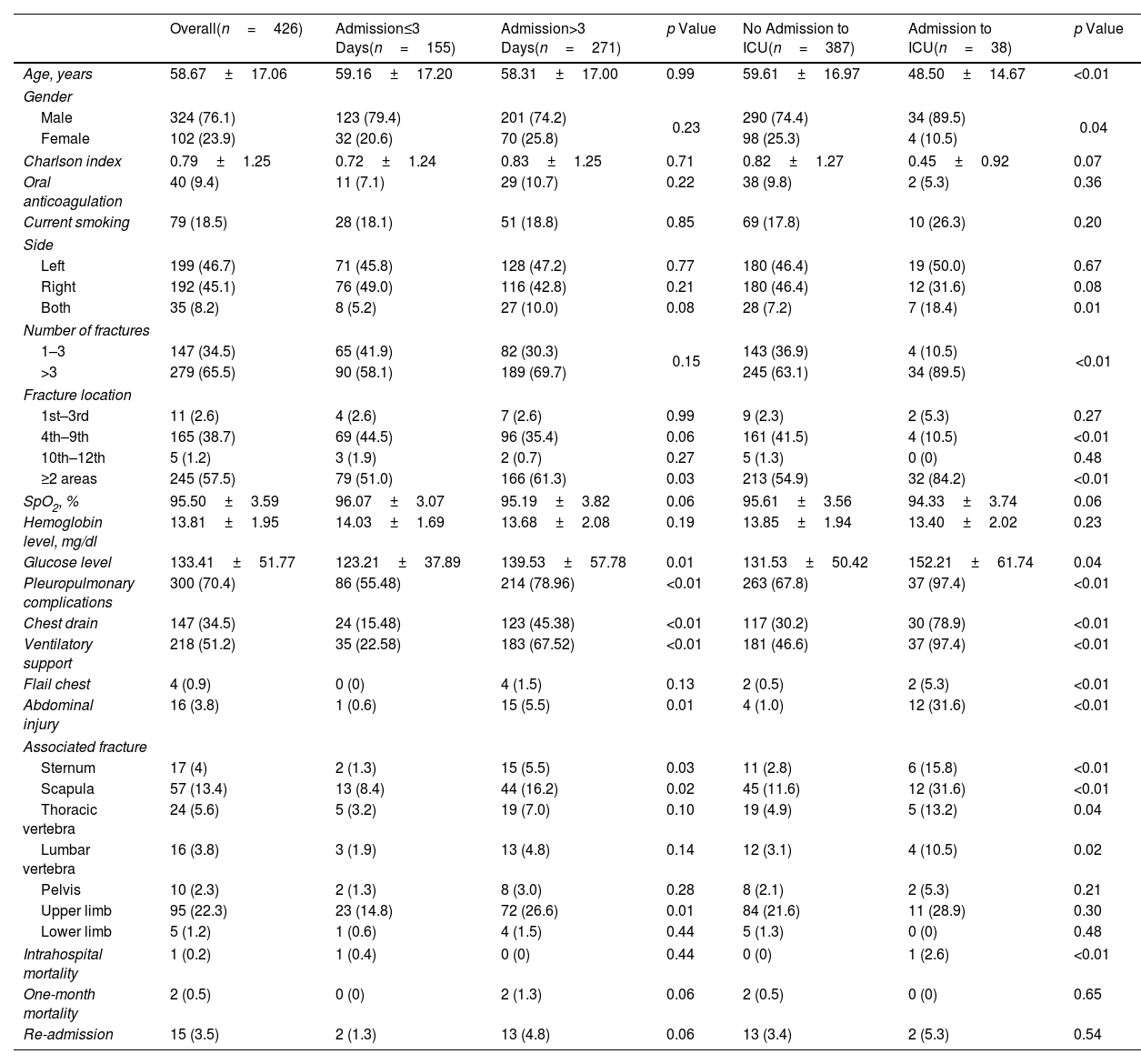
We conducted a retrospective case–control study on patients over 16 years old with rib fractures who were admitted in our institution during the period between June 2012 and June 2022. Patient's records were withdrawn from the regional public Andalusian healthcare system database. The study was approved by the local ethics committee. Patients with pathological fractures (i.e., history of malignancy, Paget's disease, osteomalacia) were excluded from the study. The information presented in Table 1 was collected from our local computerized database. To determine which factors were independently associated with long hospitalization (>3 days) and ICU admission, a logistic regression model using the Wald Backward method was performed. Variables with p values ≤0.10 according to the univariate analysis and age (independent of p value) were used as independent variables and entered into multiple logistic regression analyses.
Patient Demographic and Clinical Features.
| Overall(n=426) | Admission≤3 Days(n=155) | Admission>3 Days(n=271) | p Value | No Admission to ICU(n=387) | Admission to ICU(n=38) | p Value | |
|---|---|---|---|---|---|---|---|
| Age, years | 58.67±17.06 | 59.16±17.20 | 58.31±17.00 | 0.99 | 59.61±16.97 | 48.50±14.67 | <0.01 |
| Gender | |||||||
| Male | 324 (76.1) | 123 (79.4) | 201 (74.2) | 0.23 | 290 (74.4) | 34 (89.5) | 0.04 |
| Female | 102 (23.9) | 32 (20.6) | 70 (25.8) | 98 (25.3) | 4 (10.5) | ||
| Charlson index | 0.79±1.25 | 0.72±1.24 | 0.83±1.25 | 0.71 | 0.82±1.27 | 0.45±0.92 | 0.07 |
| Oral anticoagulation | 40 (9.4) | 11 (7.1) | 29 (10.7) | 0.22 | 38 (9.8) | 2 (5.3) | 0.36 |
| Current smoking | 79 (18.5) | 28 (18.1) | 51 (18.8) | 0.85 | 69 (17.8) | 10 (26.3) | 0.20 |
| Side | |||||||
| Left | 199 (46.7) | 71 (45.8) | 128 (47.2) | 0.77 | 180 (46.4) | 19 (50.0) | 0.67 |
| Right | 192 (45.1) | 76 (49.0) | 116 (42.8) | 0.21 | 180 (46.4) | 12 (31.6) | 0.08 |
| Both | 35 (8.2) | 8 (5.2) | 27 (10.0) | 0.08 | 28 (7.2) | 7 (18.4) | 0.01 |
| Number of fractures | |||||||
| 1–3 | 147 (34.5) | 65 (41.9) | 82 (30.3) | 0.15 | 143 (36.9) | 4 (10.5) | <0.01 |
| >3 | 279 (65.5) | 90 (58.1) | 189 (69.7) | 245 (63.1) | 34 (89.5) | ||
| Fracture location | |||||||
| 1st–3rd | 11 (2.6) | 4 (2.6) | 7 (2.6) | 0.99 | 9 (2.3) | 2 (5.3) | 0.27 |
| 4th–9th | 165 (38.7) | 69 (44.5) | 96 (35.4) | 0.06 | 161 (41.5) | 4 (10.5) | <0.01 |
| 10th–12th | 5 (1.2) | 3 (1.9) | 2 (0.7) | 0.27 | 5 (1.3) | 0 (0) | 0.48 |
| ≥2 areas | 245 (57.5) | 79 (51.0) | 166 (61.3) | 0.03 | 213 (54.9) | 32 (84.2) | <0.01 |
| SpO2, % | 95.50±3.59 | 96.07±3.07 | 95.19±3.82 | 0.06 | 95.61±3.56 | 94.33±3.74 | 0.06 |
| Hemoglobin level, mg/dl | 13.81±1.95 | 14.03±1.69 | 13.68±2.08 | 0.19 | 13.85±1.94 | 13.40±2.02 | 0.23 |
| Glucose level | 133.41±51.77 | 123.21±37.89 | 139.53±57.78 | 0.01 | 131.53±50.42 | 152.21±61.74 | 0.04 |
| Pleuropulmonary complications | 300 (70.4) | 86 (55.48) | 214 (78.96) | <0.01 | 263 (67.8) | 37 (97.4) | <0.01 |
| Chest drain | 147 (34.5) | 24 (15.48) | 123 (45.38) | <0.01 | 117 (30.2) | 30 (78.9) | <0.01 |
| Ventilatory support | 218 (51.2) | 35 (22.58) | 183 (67.52) | <0.01 | 181 (46.6) | 37 (97.4) | <0.01 |
| Flail chest | 4 (0.9) | 0 (0) | 4 (1.5) | 0.13 | 2 (0.5) | 2 (5.3) | <0.01 |
| Abdominal injury | 16 (3.8) | 1 (0.6) | 15 (5.5) | 0.01 | 4 (1.0) | 12 (31.6) | <0.01 |
| Associated fracture | |||||||
| Sternum | 17 (4) | 2 (1.3) | 15 (5.5) | 0.03 | 11 (2.8) | 6 (15.8) | <0.01 |
| Scapula | 57 (13.4) | 13 (8.4) | 44 (16.2) | 0.02 | 45 (11.6) | 12 (31.6) | <0.01 |
| Thoracic vertebra | 24 (5.6) | 5 (3.2) | 19 (7.0) | 0.10 | 19 (4.9) | 5 (13.2) | 0.04 |
| Lumbar vertebra | 16 (3.8) | 3 (1.9) | 13 (4.8) | 0.14 | 12 (3.1) | 4 (10.5) | 0.02 |
| Pelvis | 10 (2.3) | 2 (1.3) | 8 (3.0) | 0.28 | 8 (2.1) | 2 (5.3) | 0.21 |
| Upper limb | 95 (22.3) | 23 (14.8) | 72 (26.6) | 0.01 | 84 (21.6) | 11 (28.9) | 0.30 |
| Lower limb | 5 (1.2) | 1 (0.6) | 4 (1.5) | 0.44 | 5 (1.3) | 0 (0) | 0.48 |
| Intrahospital mortality | 1 (0.2) | 1 (0.4) | 0 (0) | 0.44 | 0 (0) | 1 (2.6) | <0.01 |
| One-month mortality | 2 (0.5) | 0 (0) | 2 (1.3) | 0.06 | 2 (0.5) | 0 (0) | 0.65 |
| Re-admission | 15 (3.5) | 2 (1.3) | 13 (4.8) | 0.06 | 13 (3.4) | 2 (5.3) | 0.54 |
Data are presented as No. (%) or mean±SD.
ICU: intensive care unit.
A total of 426 patients fulfilled the inclusion–exclusion criteria (324 males and 102 females) (Table 1). Two hundred and seventy-one patients (63.62%) had a long hospital stay (>3 days) and 38 patients (8.92%) were admitted in the ICU. There were no statistical differences between the short and long admission groups regarding smoking, anticoagulation use, oxygen saturation level, fracture side, mechanism of injury, number of rib fractures and fracture location. There were no differences between groups regarding mortality and re-admission rates. Patient demographic and clinical features are shown in Table 1.
Regarding the pleuropulmonary complications, the presence of pneumothorax (47.4%), empyema (2.6%) and diaphragm rupture (2.6%) were statistically higher in ICU admitted patients (p<0.05).
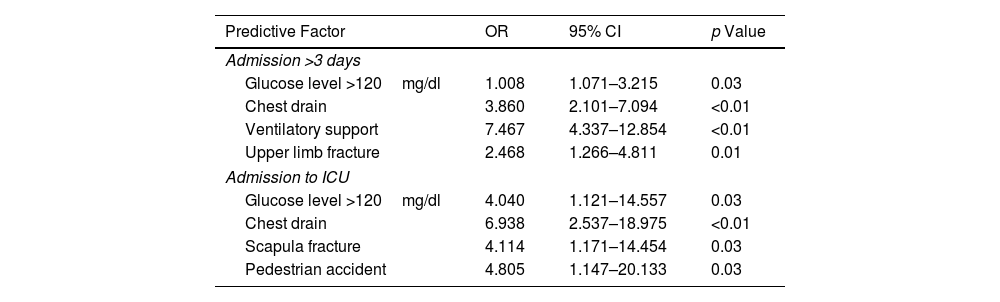
The multivariate analyses allowed us to identify four independent factors for long hospital stay and ICU admissions (Table 2). Having a blood glucose level >120mg/dl (OR=1.568), the need of chest drain (OR=3.860) and ventilatory support (OR=7.467) and the presence of an upper limb fracture (OR=2.468) were found to be statistically significant predictive factors of long hospitalization stay. On the other hand, having a blood glucose level >120mg/dl (OR=4.040), the need of chest drain (OR=6.938), the presence of a scapula fracture (OR=4.114) and suffering a pedestrian accident (OR=4.805) were also found to be statistically significant predictive factors of ICU admission.
Factors Affecting Long Admission and ICU Admission: Multivariate Analysis.
| Predictive Factor | OR | 95% CI | p Value |
|---|---|---|---|
| Admission >3 days | |||
| Glucose level >120mg/dl | 1.008 | 1.071–3.215 | 0.03 |
| Chest drain | 3.860 | 2.101–7.094 | <0.01 |
| Ventilatory support | 7.467 | 4.337–12.854 | <0.01 |
| Upper limb fracture | 2.468 | 1.266–4.811 | 0.01 |
| Admission to ICU | |||
| Glucose level >120mg/dl | 4.040 | 1.121–14.557 | 0.03 |
| Chest drain | 6.938 | 2.537–18.975 | <0.01 |
| Scapula fracture | 4.114 | 1.171–14.454 | 0.03 |
| Pedestrian accident | 4.805 | 1.147–20.133 | 0.03 |
OR: odds ratio; CI: confidence interval; ICU: intensive care unit.
Our main findings were that blood glucose levels on admission and the need for a chest tube were independent factors for long hospital stay and ICU admission. The need for ventilatory support and the presence of an upper limb fracture were also independent factors for long admission, whereas the presence of a scapular fractures or suffering a pedestrian accident were independent factor for ICU admission.
Recent research has shown that the treatment of rib fracture patients was €4000 more expensive if the patients required hospital admission.8 Moreover, the early identification of patients who can be discharged within three days would result in significant cost savings9; therefore, our study could be significant use for this task. In addition, the identification of factors associated with ICU admission could be useful to identify high-cost users and to develop different strategies to shorten UCI admissions.10
One interesting finding of our study is that blood glucose levels could be an independent predictor for long hospitalization stay and for ICU admission. To the best of our knowledge this finding has not been previously described in chest trauma patients.11 In polytrauma admission, the measurement of blood glucose levels is an easy and available test that can predict the development of a hemorrhagic shock.12 Moreover, it is correlated with the initial serum IL-6 serum levels, and it is associated with more severe injuries.13 However, it seems that the presence of high glucose levels is an important factor in the prediction of ICU mortality in trauma patients.14 Catecholamines play a central role in these high serum glucose levels of trauma patients and the catecholamine response could be a marker to severe stress.15 Moreover, high catecholamine concentrations lead to a massive release of pro-inflammatory cytokines which stimulate renal and liver gluconeogenesis.12
Another finding of our research is that the need of a chest tube could be also an independent factor for long hospital stay and ICU admission. That is in consonance with previous research, which has also reported an increase in ICU and hospital stay lengths in chest trauma patients who underwent a thoracostomy.16 In addition, a recent report which showed that COVID-19 patients who were subjected to a thoracostomy had a longer ICU and hospital stay as well as a higher mortality rate.17 Furthermore, the use of a chest tube in elderly patients with rib fractures has been found to increase the risk for intubation and pneumonia.18
We also observed that the presence of a concomitant upper limb or a scapular fracture was an independent risk factors for a long hospital stay and an ICU admission. Our findings are in concordance with previous research which showed a higher admission rate and longer hospital stay in chest trauma patients with scapular fractures.19 However, extrathoracic upper limb fractures have been described previously as associated injuries not as independent factor for an increase of length of stay.20
Nevertheless, there are a series of limitation associated with this work. First, the retrospective design of the study made it exposed to errors due to confounding and former exposure to risk variables. However, in order to address this potential bias, logistic regression analyses were performed, including several potential confounding factors. Moreover, the sample size of the studied population was relatively small. In addition, it can be difficult to generalize these findings from a single center to other centers.
We conclude that blood glucose level and the need for a chest tube were independent factors that could predict a long hospital stay and ICU admission. Moreover, the need for ventilatory support on admission and the presence of an upper limb fracture could predict a long hospital stay whereas the presence of a scapular fracture and a history of pedestrian accident could predict an ICU admission. However, the number or localization of the rib fractures did not play an important role in the prediction of these parameters.
Authors’ ContributionsOFG and DGQ had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects. GZ, RAS and IT contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript.
FundingNone declared.
Conflict of InterestsThe authors state that they have no conflict of interests.