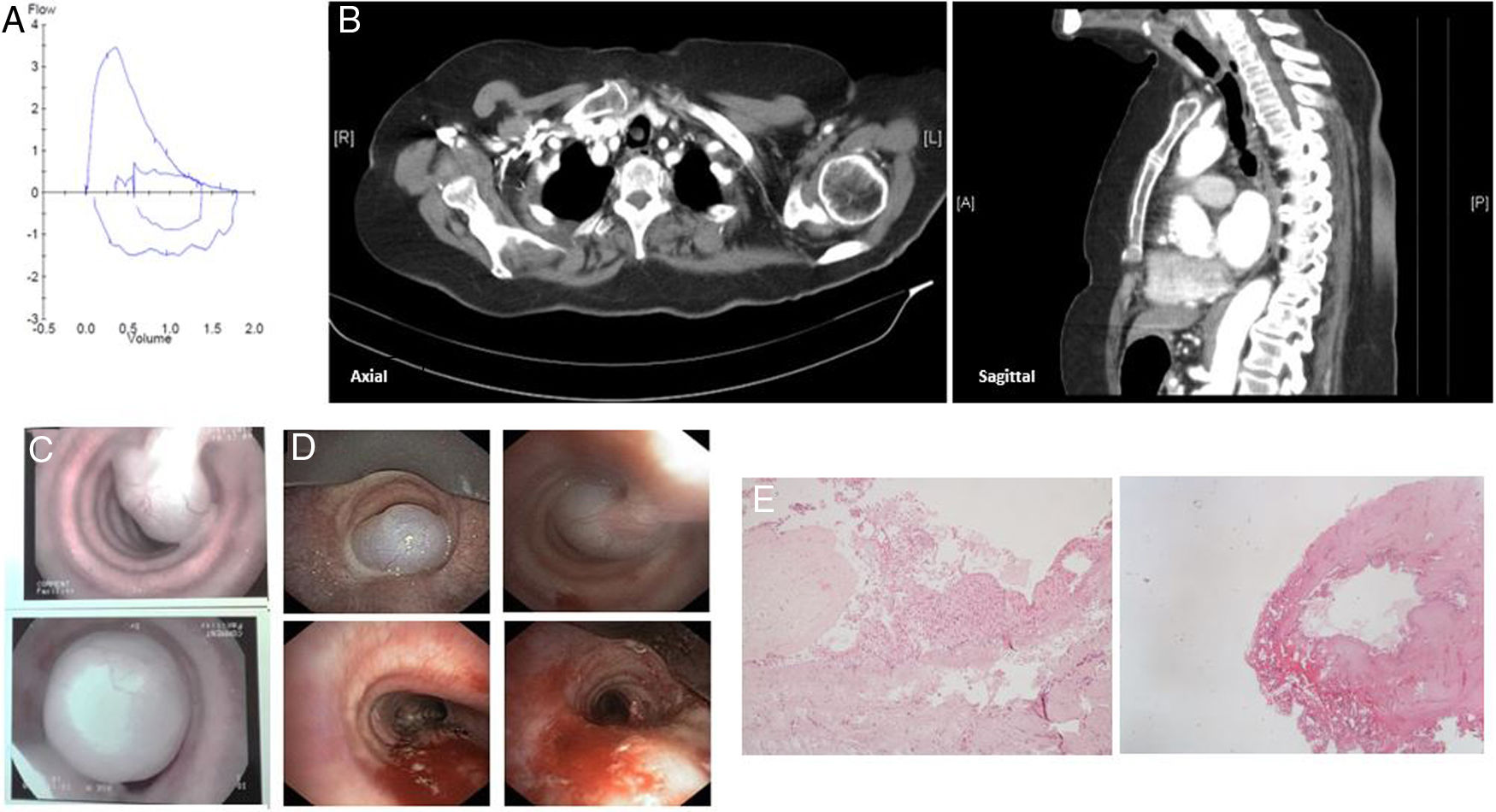
A 86-year-old woman, non-smoker, presented dyspnea of progressive aggravation with a few months of evolution that increased in dorsal decubitus, associated with episodes of cough with sputum difficult to expel and wheezing. Spirometry showed only bronchiolar obstruction (Fig. 1A). Thoracic CT scan showed a pedicled lesion in the trachea (Fig. 1B). Flexible bronchoscopy confirmed the presence of a large, non-hemorrhagic, smooth, pink polypoid lesion with a pedicle implanted in the posterior wall of the middle third of the trachea. Rigid bronchoscopy was performed with argon-plasma therapy and mechanical debridement with en bloc removal of the lesion (Fig. 1C and D). Pathological examination was compatible with polypoid fibroma of the tracheal mucosa, a benign lesion (Fig. 1E). There was no recurrence and the patient remains asymptomatic to this day.
Spirometry flow-volume loop (A) was not typical of an extrathoracic obstruction. CT-scan axial and sagittal images (B) show a pedicled lesion in middle third of the trachea. Images of flexible bronchoscopy (C) and rigid bronchoscopy (D) before and after argon-plasma therapy and mechanical debridement with en bloc removal of the lesion. Histological images of polypoid fibroma of the tracheal mucosa [hematoxylin and eosin staining] (E).
Primary tumors of the trachea are rare, accounting for about 2% of upper respiratory tract tumors and 0.3% of all tumors. Only 20% of these tumors are benign.1 These lesions often manifest themselves with symptoms that mimic obstructive pulmonary pathology, and patients are then treated with targeted therapy without clinical improvement.2 The gold standard method for the diagnosis of central airway obstruction is bronchoscopy, allowing not only the diagnosis of the lesions but also their treatment.


![Spirometry flow-volume loop (A) was not typical of an extrathoracic obstruction. CT-scan axial and sagittal images (B) show a pedicled lesion in middle third of the trachea. Images of flexible bronchoscopy (C) and rigid bronchoscopy (D) before and after argon-plasma therapy and mechanical debridement with en bloc removal of the lesion. Histological images of polypoid fibroma of the tracheal mucosa [hematoxylin and eosin staining] (E). Spirometry flow-volume loop (A) was not typical of an extrathoracic obstruction. CT-scan axial and sagittal images (B) show a pedicled lesion in middle third of the trachea. Images of flexible bronchoscopy (C) and rigid bronchoscopy (D) before and after argon-plasma therapy and mechanical debridement with en bloc removal of the lesion. Histological images of polypoid fibroma of the tracheal mucosa [hematoxylin and eosin staining] (E).](https://static.elsevier.es/multimedia/03002896/0000005700000007/v2_202107030624/S0300289619306076/v2_202107030624/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)







