Pneumothorax after shoulder arthroscopy is an infrequent complication that has hardly ever been published in the literature and for which there is no clear cause.1–3 Possible causes are postulated to be surgery-related, anaesthesia-related and respiratory comorbidities.1–3 The most commonly advocated hypotheses are inadvertent accidental injuries to the pleura or lung during regional anaesthetic block, continuous positive pressure from the arthroscopic pump, the patient's position during surgery or excessive intra-articular debridement.1–3 Nonetheless, the exact cause has not been proven in any case.
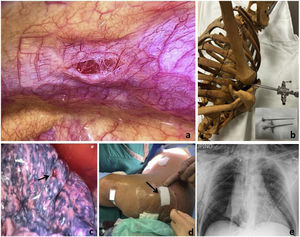
We present the case of a 66-year-old male smoker with no other medical or surgical history of interest who underwent arthroscopic surgery of the right shoulder through the usual portals for a ruptured supraspinatus muscle (Fig. 1d). Six hours after completion of surgery, the patient presented dyspnoea with an O2 saturation of 85%. The patient underwent a chest X-ray which showed massive right pneumothorax and subcutaneous emphysema (Fig. 1e). We proceeded to place an endothoracic drainage tube as a matter of urgency, but in the absence of complete lung re-expansion and persistent air leak, we decided to perform surgery by videothoracoscopy. Here we identified the origin of the leak as a deep rounded laceration in the posterolateral aspect of the right upper pulmonary lobe. This was of iatrogenic origin secondary to the insertion of the posterior arthroscopy trocar, and with an opening notch in the parietal pleura above it (Fig. 1a, c, and d). We repaired the laceration with a wedge resection using a surgical stapler.
(a) Parietal pleural lesion corresponding to the trocar entry point. (b) Simulation of the patient's position in the operating theatre and possible direction of the trocar for penetrating the thorax. Insert: working control of the arthroscope with the sharp trocar used. (c) Wound in the lung parenchyma located immediately below the chest wall injury (arrow). (d) Healing of the arthroscopy incisions. The arrow points to the trocar incision causing the pneumothorax. (e) Chest X-ray in AP showing complete right pneumothorax accompanied by subcutaneous emphysema.
There are very few documented cases such as this one of pneumothorax associated with surgical instrumentation in the literature. We can affirm that the difference between this case and the others is that when performing videothoracoscopy we could see the iatrogenic pulmonary lesion, which occurred while introducing the working trocar through the posterior portal. We believe that there may have been several reasons for this complication. Firstly, although we generally use a blunt trocar to introduce the arthroscope sleeve through the posterior portal, in this case we used a sharper trocar, which was similar to the one used in knee arthroscopy (Fig. 1b, inset). Secondly, the position of the patient and the experience and confidence of the surgeon, in this case an accomplished surgeon, may also have played a role. The patient was placed in the lateral decubitus position but with excessive posterior body tilt with the arm in traction, with antepulsion and some adduction. Pleural penetration with the trocar could take place at the end of the procedure, when after tendon suture, we accessed the glenohumeral space again to visualise the correct tendon reinsertion from this area. At this point, as the shoulder was swollen by the insufflated water, the coracoid was not correctly referenced. Combined with the patient's poor position and the surgeon's faith, it is possible that this could have led to iatrogenesis.
Therefore, we insist on the correct positioning of the patient, awareness of this possible complication and extreme caution during surgery. In addition, it is important to recognise this complication in the postoperative period and to manage it appropriately at an early stage.
Authors’ ContributionsAll authors have contributed intellectually to the case, meet the conditions of authorship and have approved the final version of the case.
FundingThere has been no funding or sponsorship for the publication of this article.
Conflict of InterestThe authors declare that they have no conflict of interest.