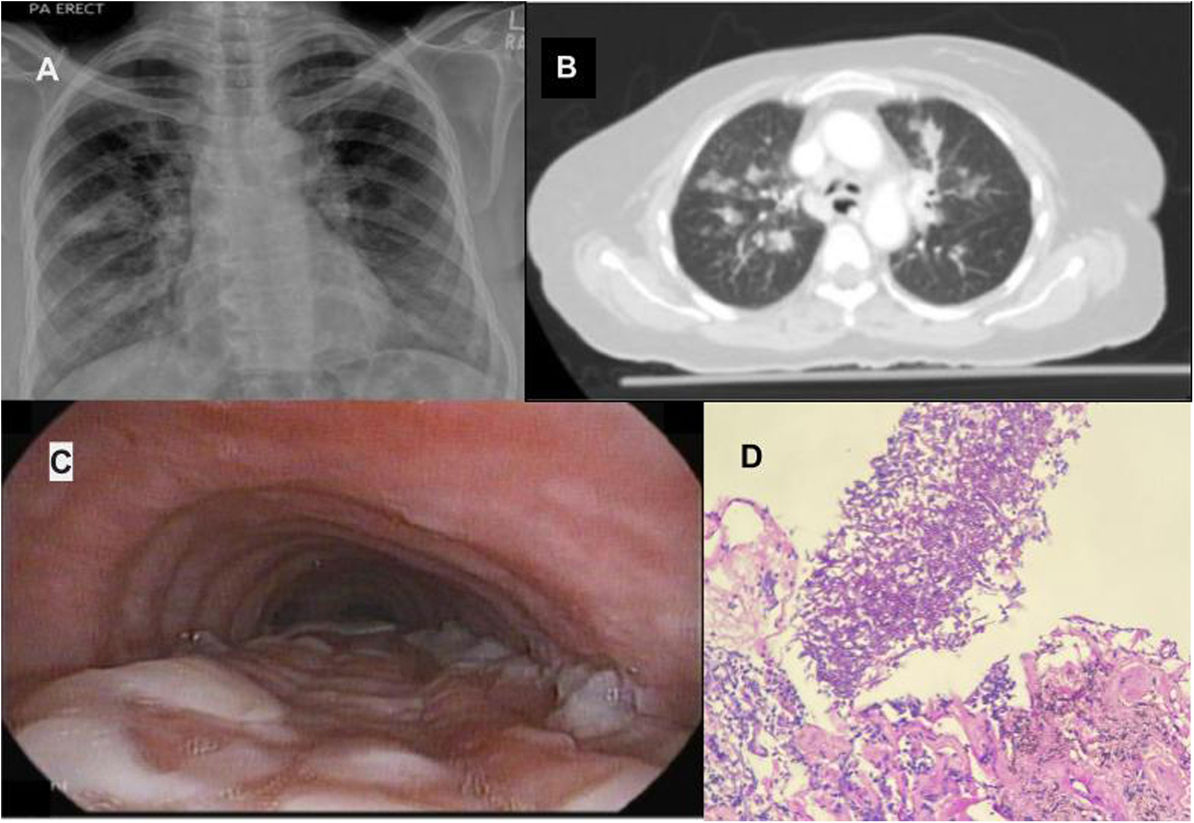
A 65-year-old female presented with shortness of breath and cough for the last 10 days. She was mildly hypoxemic, and chest imaging showed bilateral nodular infiltrates and consolidations, predominantly in the right upper lobe (Fig. 1A and B). She underwent bronchoalveolar lavage and transbronchial lung biopsy of the right upper lobe. On bronchoscopic airway examination, the posterior mid-distal trachea and proximal bronchi were covered with a thick white membrane (Fig. 1C). The transbronchial biopsy showed numerous septate hyphae, and the endobronchial biopsy from the membrane grew Aspergillus on tissue culture (Fig. 1D). Her HbA1c was 9.5%, and work-up for HIV, autoimmune diseases, tuberculosis and malignancy was negative. The patient was diagnosed to have invasive aspergillosis with pseudomembranous tracheobronchitis due to aspergillus. The uncontrolled diabetes was likely the immunosuppressant factor leading to the Aspergillus tracheitis and invasive aspergillosis.
(A) Chest X-ray showing bilateral alveolar opacities, more prominent in the right upper lobe. (B) CT Chest showing nodular ground glass opacities in the right upper lobe. (C) Bronchoscopic view from the mid trachea showing multiple white plaques on the posterior tracheal wall, extending up to the carina (seen distally in the picture). (D) Lung parenchyma with alveolar spaces infiltrated by septated hyphae branching at acute angles.
Patient consent was obtained for permission of writing the case about her. All information regarding the patient has been deidentified.
Consent for publicationThe manuscript has been read and approved by all the authors, and each author believes that the manuscript represents honest work. All authors have consented for publication. Moiz Salahuddin takes responsibility for the integrity of the work, from inception to published article and should be designated as ‘guarantor’.
FundingNo grant or funding was received for this study.
Conflict of interestsNo author has any competing interests in this study.