Hypoxaemia is a typical feature of the coronavirus disease 2019 (COVID-19). The rapid rise in the number of patients requiring oxygen therapy during the pandemic may cause a sharp increase in oxygen demands and potential threats of supply disruption, particularly in developing countries1 or nursing homes. Moreover, the use of elevated oxygen flows via nasal cannula raises concerns about exhaled air dispersion distance and the potential risk of generating aerosols.2–6
The Double-Trunk Mask (DTM) (image and description in supplement) is a patent-free handmade system which, when placed over nasal cannula, increases the PaO2 by 50% in patients with acute respiratory failure without clinical impact on PaCO2.7 From another perspective, the DTM may reduce the oxygen flow required to correct hypoxaemia which, in addition to reducing side-effects of prolonged dry oxygen administration,8–10 could have crucial implications in situations where medical gases are a rare commodity. The study's objective was to assess the efficacy of the DTM in preserving oxygen consumption in patients with COVID-19.
All adult patients with laboratory-confirmed COVID-19 and hypoxaemia requiring low-flow oxygen therapy (LFOT) ≤15L/min to maintain SpO2 between 92 and 96%, who were consecutively hospitalized between April and May 2020 in our hospital, were asked to participate in the study.
This ClinicalTrials.gov registered study (NCT04346420) was conducted with the approval of the local ethics committee. All subjects signed informed consent. Exclusion criteria were chronic respiratory diseases, language barriers, confusion, altered consciousness (Glasgow Coma Scale ≤12), hypoxaemia corrected with oxygen flow ≤3L/min and any contra-indication to arterial puncture.
Patients were in a semi-recumbent position and received LFOT through their standard oxygen delivery method. The initial oxygen flow and delivery system were determined in accordance with our standard practice. The baseline oxygen flow was titrated to achieve a target SpO2 value of 94% at the lowest output. Oxygen flow requirements determined the baseline oxygen delivery system (supplements). The baseline delivery system was then replaced by the DTM covering nasal cannula for 30min. Oxygen output (primary outcome) was adjusted to achieve the same SpO2 target as at baseline. After this period, the DTM was withdrawn and the standard oxygen delivery system was reinstated for 30min. Oxygen output was readjusted to achieve the baseline SpO2 value. Patients received no instructions regarding nasal or mouth breathing during the whole process. Arterial blood gases, vital parameters and oxygen output were measured at baseline (T0) and at the end of the 30-min DTM period (T30). Vital parameters and oxygen output were measured again 30minutes after the DTM was withdrawn (T60). Comfort-discomfort level with each system was assessed at T30 and T60 (supplements).
Eleven subjects were needed to detect a mean difference of 2L/min11 (SD, 1.8L/min) in oxygen output (α-risk, 0.05; power, 90%). Because SpO2 may inaccurately reflect arterial oxygen saturation (SaO2) and therefore interfere with our design, patients were retrospectively excluded from the analysis if SpO2-SaO2 mismatch exceeded the expected error of 4%.12,13 Data are presented as mean±SD or median [interquartile range (IQR)] as appropriate. Pairwise comparisons were tested with paired t-test or Wilcoxon test. Ordinal paired data were compared with Wilcoxon test. P-values<0.5 were considered statistically significant.
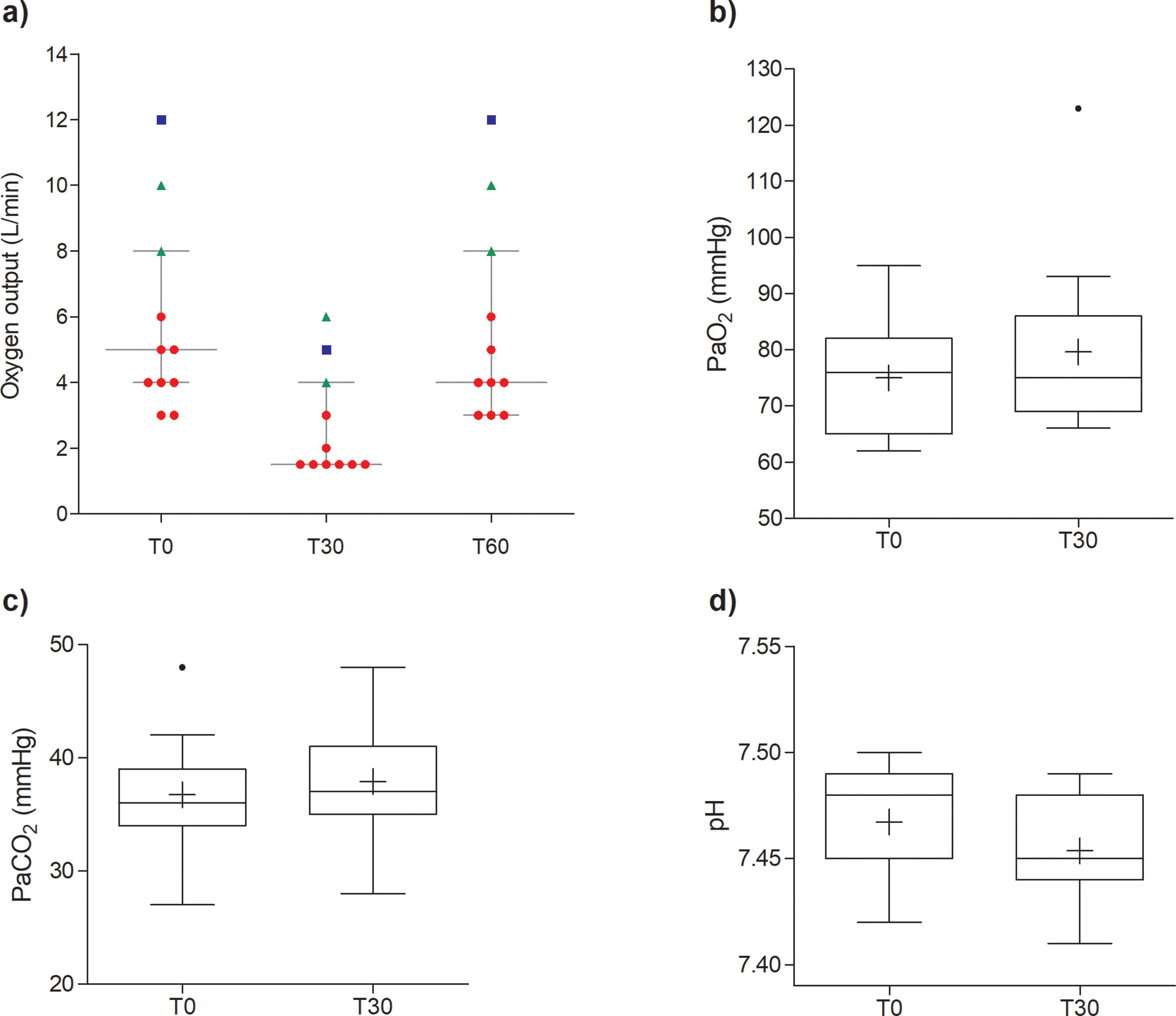
Of 12 patients who completed the entire study procedure, one was excluded from the analysis because SpO2-SaO2 difference at T0 was 4.3%. Final analyses were performed on 11 patients (61±14 years; 27% female). E-Table 1 details baseline characteristics. Compared with standard delivery systems, the oxygen output was significantly reduced with the DTM (median [IQR], 5 [4–8]L/min vs 1.5 [1.5–4]L/min; p=0.003) when oxygen saturation and PaO2 remained stable. The DTM was also associated with a significant but slight increase in PaCO2 (median, 36 vs 37mmHg, p=0.006), a decrease in pH (median, 7.48 vs 7.45, p=0.009) and an increase in respiratory rate (mean, 26 vs 30breaths/min, p=0.05), Fig. 1, e-Table 2. Other parameters were unaltered. The DTM was generally considered less comfortable than the baseline oxygen delivery system, especially in patients requiring low oxygen flow at baseline (e-Fig. 2). There were no differences between T0 and T60 for any outcomes (e-Table 2), indicating that all values were reset when the standard delivery system was reinstated.
Change of oxygen output and blood gas outcomes. (a) Panel shows raw values of oxygen flow before (T0) and after (T30) wearing the double-trunk mask, as well as after reinstating the baseline oxygen delivery system (T60). Horizontal lines indicate median, 25th and 75th percentiles. The shape of each data point represents the baseline oxygen supply system: circles for nasal cannula, triangles for oronasal mask and square for the non-rebreathing mask. (b–d) Panels show respectively PaO2, PaCO2 and pH outcomes before (T0) and after (T30) wearing the double-trunk mask. The boxes indicate 25th and 75th percentiles; horizontal lines and “+” within boxes indicate median and mean, respectively; whiskers indicate the highest and lowest values within 1.5× interquartile range; and points beyond the whiskers indicate outliers.
Treating hypoxaemia is the cornerstone of COVID-19 patient management and this pre-post intervention trial shows that the DTM enables clinicians to safely treat severe hypoxaemia while reducing the oxygen flow by more than half that required with conventional delivery systems. Therefore, settings in which oxygen supplies are limited (e.g. nursing homes, healthcare centres in deprived medical areas, during patient transport) may benefit most from the DTM. Although evaluation of its place relative to the non-rebreathing mask, high-flow oxygen therapy or non-invasive ventilation was not within the scope of this study, we believe the DTM could also be considered when SpO2 falls below the target value with standard LFOT systems.7,11 Consequently, the need for non-invasive respiratory support, which increases risks of generating aerosols,6 may possibly be avoided.
The DTM was considered less comfortable than LFOT delivered through nasal cannulas, yet patients who initially required high oxygen flow considered the DTM as equally comfortable. This might be explained by using a facemask at baseline or the large absolute oxygen flow reduction with the DTM. However, the low number of patients wearing oxygen facemasks at baseline precludes generalization of our conclusions with these systems.
The importance of our findings is emphasized by the large oxygen flow reduction under the DTM (56%) and the high proportion of hospitalized patients who met the inclusion criteria at some point of their stay (266/412). The main limitation was the pre-post intervention design of short duration. Moreover, the investigator who readjusted oxygen flow was not blinded in order to limit prolonged and multiple exposures of healthcare workers. Randomized controlled trials of longer duration involving a broader range of oxygen flows are required.
In conclusion, our study showed that the DTM is a useful oxygen delivery system that enables a safe reduction in oxygen output without hampering patient oxygenation. This finding is of particular interest in the current context of high and potentially overwhelming oxygen demand.
Sources of supportNone.
Conflict of interestNone.
We are grateful to Prof. Annie Robert for the statistical review of our analysis. We thank Mariana Andrade MD, who provided editorial assistance. Compensation but no commercial funding was received for this purpose. We also thank the interns (S. Brilot, S. Demartin, E. Lagneaux, R. Lattenist, J. Lux, G. Pierman, G. Vandercam, S. Wallemacq, M. Gagliardi) in the internal medicine and pneumology departments for their contributions.