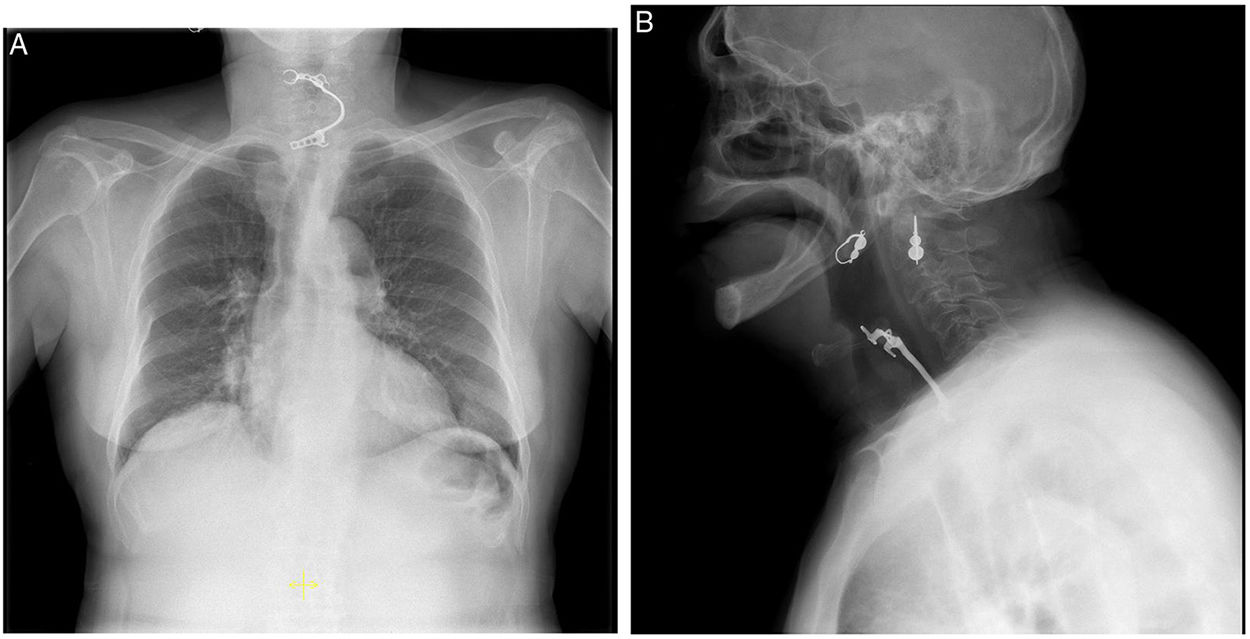
73-Year-old female patient, which presented to the emergency service with dyspnea, cough and hoarseness. Reference to an episode of choking at dinner the day before. Heimlich maneuvering was performed with food expulsion (meat), with transient improvement, but no dental prosthesis was found after the event. Chest radiograph shows dental prosthesis located on the laryngo-esophageal transition at the C4–C7 level. The patient was submitted to endoscopic removal of the prosthesis in the operating room. Severe pharyngeal edema was detected (need for oro-tracheal intubation), and upper esophagus showed extensive superficial ulceration at the denture impaction site, without active hemorrhage. The patient was admitted to Intensive Care Unit. During the stay, the institution of corticotherapy and ibuprofen resulted in a decrease in pharyngeal edema, with a 48-h cuff-leak test compatible with arway permeability, which allowed successful extubation. On the thirteenth day she got discharged.
Foreign body airway obstruction usually manifests as acute respiratory failure. However, in about 50% of these patients the manifestation occurs within the first 24h after the episode and cough is the most common symptom.1,2 It is fundamental to maintain a high degree of clinical suspicion in patients with respiratory distress after a choking episode and Chest radiograph may confirm the diagnosis1,2 (Fig. 1).