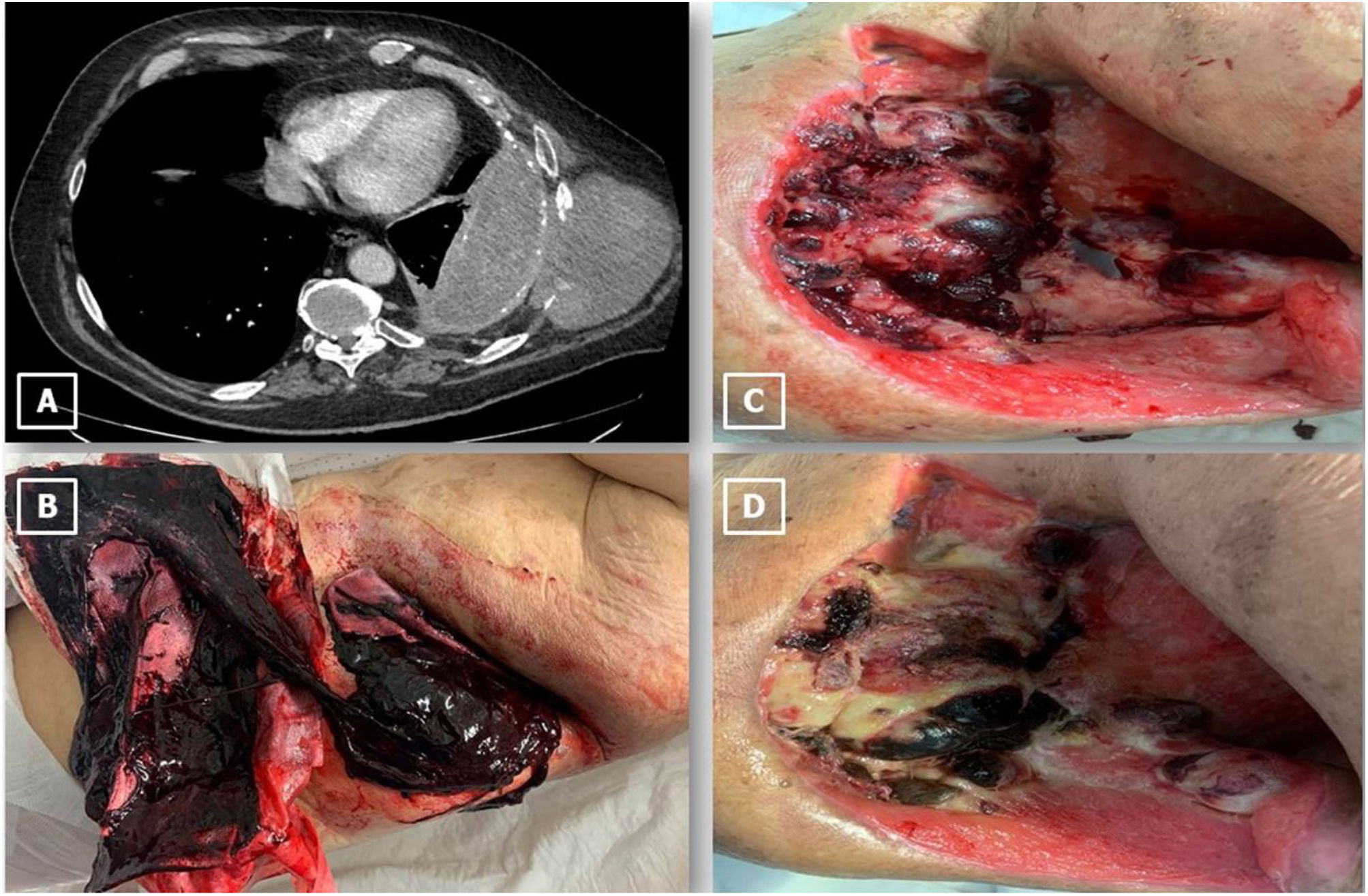
A 62-year-old man with a previous history of pulmonary tuberculosis from 15 years earlier was complaining of persistent left rib pain. Chest computed tomography showed encapsulated pleural effusion, pleural calcification and heterogeneous soft tissue mass (85mm×110mm) destroying the 9th and 10th ribs (Fig. 1A). A diagnostic-therapeutic thoracocentesis was performed, which revealed purulent pleural effusion and elevated lactate dehydrogenase (639). In addition, an ultrasound-guided fine needle aspiration of soft tissue mass was carried out without detecting any malignant cells, only material consisting of blood. Previous radiological images were also reviewed, in which the patient already had a mild pleural effusion and chronic pleural thickening. Due to his previous history of tuberculosis, his pleuritic pain and complementary tests’ results, our suspected diagnosis was tuberculous empyema necessitatis, and tuberculostatic drugs were started.
(A) Chest computed axial tomography showed encapsulated pleural effusion, pleural calcification and heterogeneous soft tissue mass (85mm×110mm) destroying the 9th and 10th ribs. (B) Clots after thoracostomy bleeding. (C) Friable protruding lesions in thoracostomy. (D) Protuding lesions after radiotherapy and chemotherapy treatment.
Two months later, because of the lack of response to tuberculostatic treatment without any clinical-radiological improvement and the increase in size of the soft tissue mass, we decided to perform a diagnostic-therapeutic surgery. Due to the extend period of infection, as well as the patient's morbidity, we thought that lung re-expansion would not be achieved, and an open thoracostomy would be an appropriate surgical option. During surgery, a large collection of blood with many clots was observed. Soft tissue mass’ histological findings were: necrotic-haemorrhagic material and occasional atypical cells, without any tumour cells in resected ribs. Furthermore, a mycobacterium tuberculosis complex was isolated in parietal pleura culture, which supported our initial suspected diagnosis.
In the first postoperative month, the patient had mild self-limited bleeding in the thoracostomy. In the third month, he suffered a massive haemorrhage, requiring hospital admission and emergency haemostatic surgery (Fig. 1B). During admission, protruding lesions prone to bleeding were observed, causing anaemia in the transfusion range (Fig. 1C). Due to torpid evolution, the mass was biopsied two more times and the final result was epithelioid angiosarcoma. The patient was not a candidate for resective surgical treatment, choosing radical radiotherapy and chemotherapy (Fig. 1D). He died of bilateral pneumonia two months after diagnosis.
Epithelioid angiosarcoma is an uncommon subtype of soft tissue sarcoma that is rare in the chest wall. Its prognosis is poor. This pathology is a major diagnostic challenge due to its low incidence (few cases have been published in the literature),1 nonspecific clinical features and complex differential diagnosis (empyema necessitatis, haematoma).2,3 Biopsy may be inconclusive because of diffuse haemorrhagic and necrotic areas. Immunohistochemistry is important in the definitive diagnosis with positivity for CD31, CD34, ERG and Factor VIII. It is thought the origin of epithelioid angiosarcoma of the chest wall could be related to chronic pleuropulmonary inflammation, because this pathology has been described in patients with a previous history of pulmonary-pleural tuberculosis and empyema.4 In conclusion, this tumour should be suspected in patients with soft tissue mass, a previous history of chronic tuberculous empyema, and poor evolution in spite of tuberculostatic drugs and inconclusive biopsies, in order to achieve an early-stage diagnosis and to be a candidate for resective surgical treatment.
Conflict of InterestsThe authors state that they have no conflict of interests.