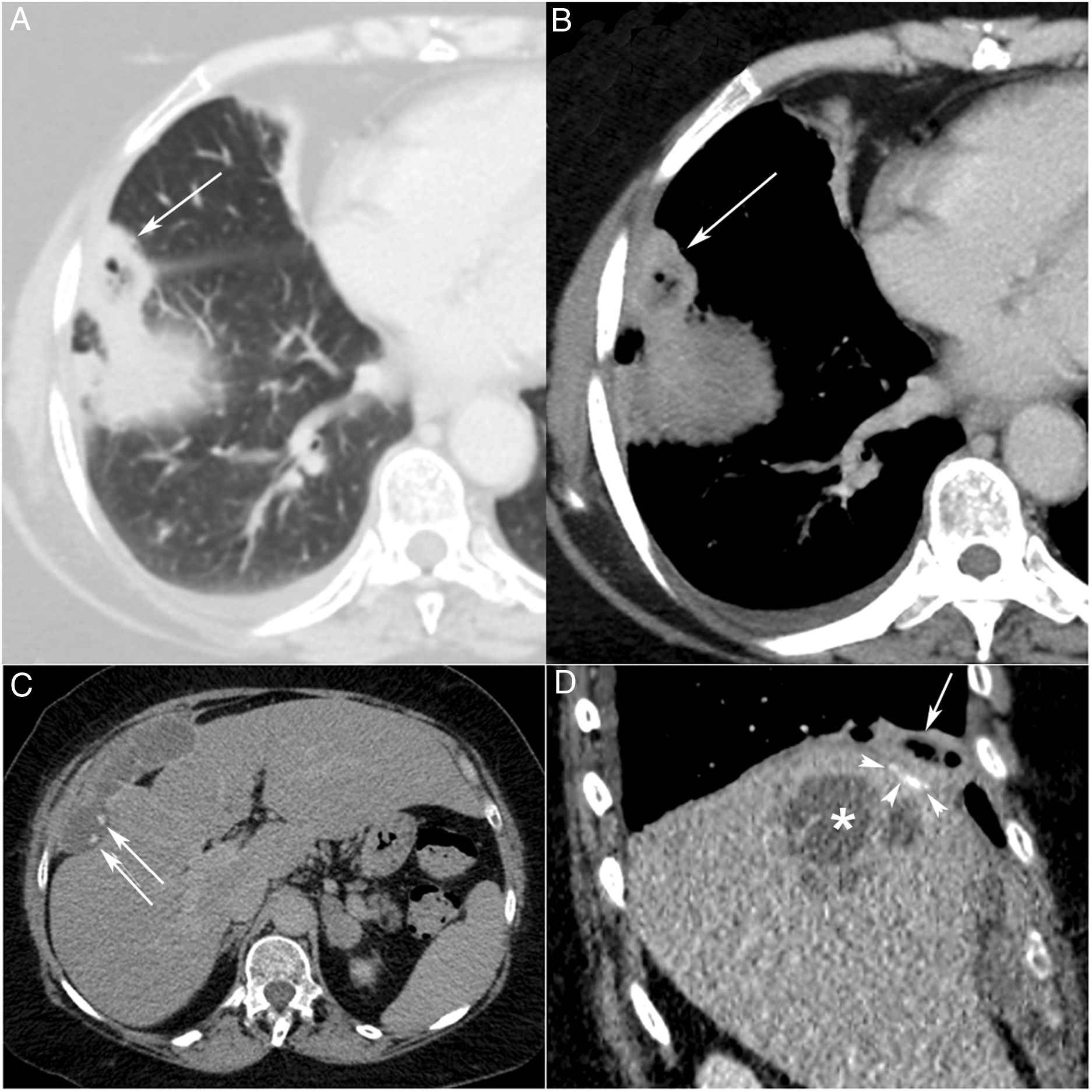
A 60-year-old woman presented with a 2-week history of fever, cough, yellow expectoration, and right upper quadrant pain. The patient had a medical history of laparoscopic cholecystectomy for cholelithiasis 21 years previously. Contrast-enhanced chest computed tomography showed a cavitated nodular lesion located in the middle lobe and right lower lobe. The lesion communicated with a perihepatic fluid collection containing two small calcified-dependent foci (Fig. 1). A diagnosis of perihepatic abscess eroding through the diaphragm and causing a lung abscess was made. Cultures of the bronchoalveolar lavage grew Klebsiella pneumonia. Video-assisted thoracoscopic surgery revealed lung abscess cavity in contact with the diaphragm. Drainage was performed, and several gallstones were retrieved from the collection.
Axial chest CT images obtained with lung (A) and mediastinal (B) window settings demonstrate a small, nodular, cavitary pulmonary lesion in the right lower lobe (arrows). An abdominal CT (C) image shows a large and complex perihepatic collection containing two calcified gallstones (arrows) adjacent to the right hepatic lobe. A sagittal thoracoabdominal reconstruction (D) demonstrates the abdominal collection (asterisk) adjacent to the pulmonary abscess (arrow). Note also the gallstones inside the lesion (arrowheads).
Iatrogenic perforation of the gallbladder during laparoscopic cholecystectomy is a recognized occurrence, with gallstones dropping in the peritoneal cavity. A small percentage of dropped stones causes complications, including abscess and fistula formation.1,2 Thoracic complications from spilled gallstones, such as pneumonia, empyema or lung abscess, are rare. Hemoptysis, pleurolithiasis, cholelithoptysis, and broncholithiasis due to spilled gallstones have been reported. In some instances, stones may be cleared from an abscess cavity using minimally invasive techniques, but open drainage remains the most effective and certainly the simplest treatment.1,2