A 40-year-old male consulted complaining of progressive dyspnea worsening over the last 4 years. During history, the patient mentioned motor-vehicle incidents at the ages of 6 and 12 years and posteriorly left diaphragmatic paralysis at 14. In 2019, he was hospitalized on the grounds of a respiratory infection. Upon pulmonary auscultation, borborygmi were found. A thoracoabdominal Computed Tomography (CT) was taken, revealing a diaphragmatic hernia of approximately 6.5cm×4.5cm. The hernial sac contained abdominal viscera in the left hemithorax. A comparison of the 2023 CT scan with the one obtained in 2019 demonstrates progression of the herniation.
After multidisciplinary discussion and planning, the patient underwent surgery for diaphragmatic reconstruction. Initially, two double J stents were placed to assure left ureter patency during and after surgery. He was positioned in right lateral decubitus. Video Assisted Thoracic Surgery (VATS) was performed first. Minimal visceral adhesions to the chest wall led to continuing with a thoracoabdominal approach through the 7th intercostal space. Abdominal viscera were manually reduced, with continuous anesthesia monitoring of the intraabdominal pressure. The diaphragm was reconstructed with a dynamic patch using 2 pieces of 2-mm-thick Gore-Tex Dual Mesh (W.L. Gore and Associates) tailored to the size of the defect. The prosthesis was anchored posteriorly, laterally, and anteriorly to the chest wall with 11 Ethibond 1 sutures. To prevent tearing of the sutures through the wall, they were tied over manually tailored Gore-Tex buttons.1
After surgery, an intravenous contrast CT scan was performed to assure adequate perfusion and positioning of all the abdominal viscera. The patient spent the first two postoperative days in the ICU, where total parenteral nutrition was initiated. After chest tube removal on day 2, he was transferred to the ward, where diet was advanced as bowel sounds progressed. The patient was discharged on postoperative day 10.
It was difficult to approach this case. Given that the herniation between CTs had shown (despite gradual) a significant progression, the risk of undergoing surgery was considered inferior to the possible long-term complications of a conservative management. A case series by Ganie et al. demonstrated a 27% mortality of patients after undergoing surgical management. However, the mortality of a sudden strangulation is considerable given the significant herniation of visceral structures. The young age of the patient increased the probability of such an emergent situation occurring. It was indispensable to balance the total risk implied with a surgical treatment (perforation while manipulating viscera, correct fitting of rearranged organs, respiratory compromise due to diaphragmatic manipulation, etc.) against the total risk of an expectant management2 (abrupt strangulation of the abdominal contents).
Currently, there are few similar cases described in the literature yet neither specific protocols nor management guidelines exist. This proved to be the greatest limitation when deciding the most beneficial care we could provide. In our patient's case, considering age, hernial progression, recent worsening of respiratory symptoms and a comorbid diaphragmatic paralysis, a programmed multidisciplinary surgical approach involving Urology, Thoracic, General and Vascular surgery as well as Radiology was undertaken (Fig. 1).
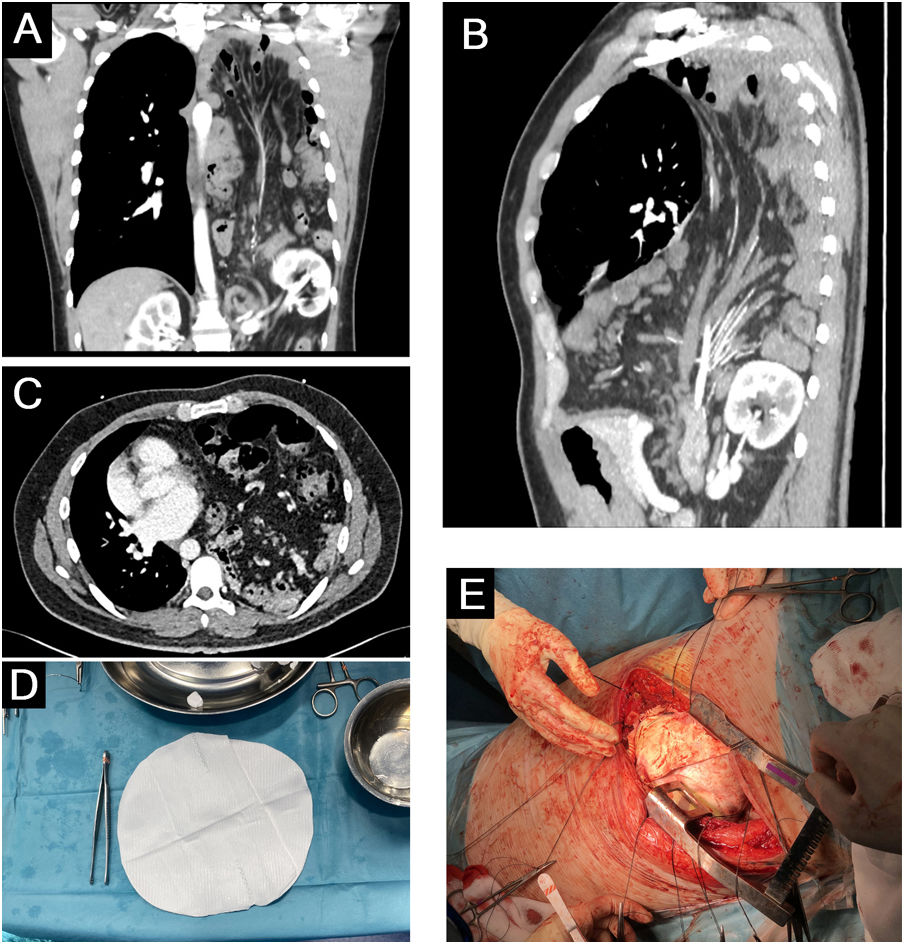
Images A–C belong to the 2023 Computed Tomography (CT) scan in the coronal, sagittal and axial planes, respectively. Herniation of the abdominal viscera into the left hemithorax is evident, with the following sac contents: ventral portion of a pancreas bifidum, left kidney, mesenteric root, transverse colon, ascending colon, cecum, appendix, a major portion of the stomach as well as the angle of Treitz and the entire small intestine. The displacement of the mediastinum toward the right has led to compression of not just the left but also the right lung, which is consistent with the patient's worsening dyspnea. Image D corresponds to the Gore-Tex Dual mesh dynamic patch, 20cm×30cm in diameter, used in this case. Its dimensions were revised again prior to placement to ensure complete coverage of the defect. Image E was taken just moments after the end of the placement of the patch with 11 manually tailored Gore-Tex buttons additionally sutured to provide structural support to the prosthesis.
Does not apply.
Informed consent statementThe authors confirm that written informed consent has been obtained from the involved patient and he has given approval for this information to be published in this case report.
Funding statementThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors declare that they have no relevant or material financial interests that relate to the research described in this paper.