As a complement to a previous study by our group whose data and methodology have already been published,1,2 we hypothesised that smokers who only attend the first visit of a cessation program are different from those who attend the full program. Therefore, the aim of this study was to describe whether there are differential characteristics between smokers who only attended the initial visit of a smoking cessation consultation versus those who attended more than one of the follow-up visits.
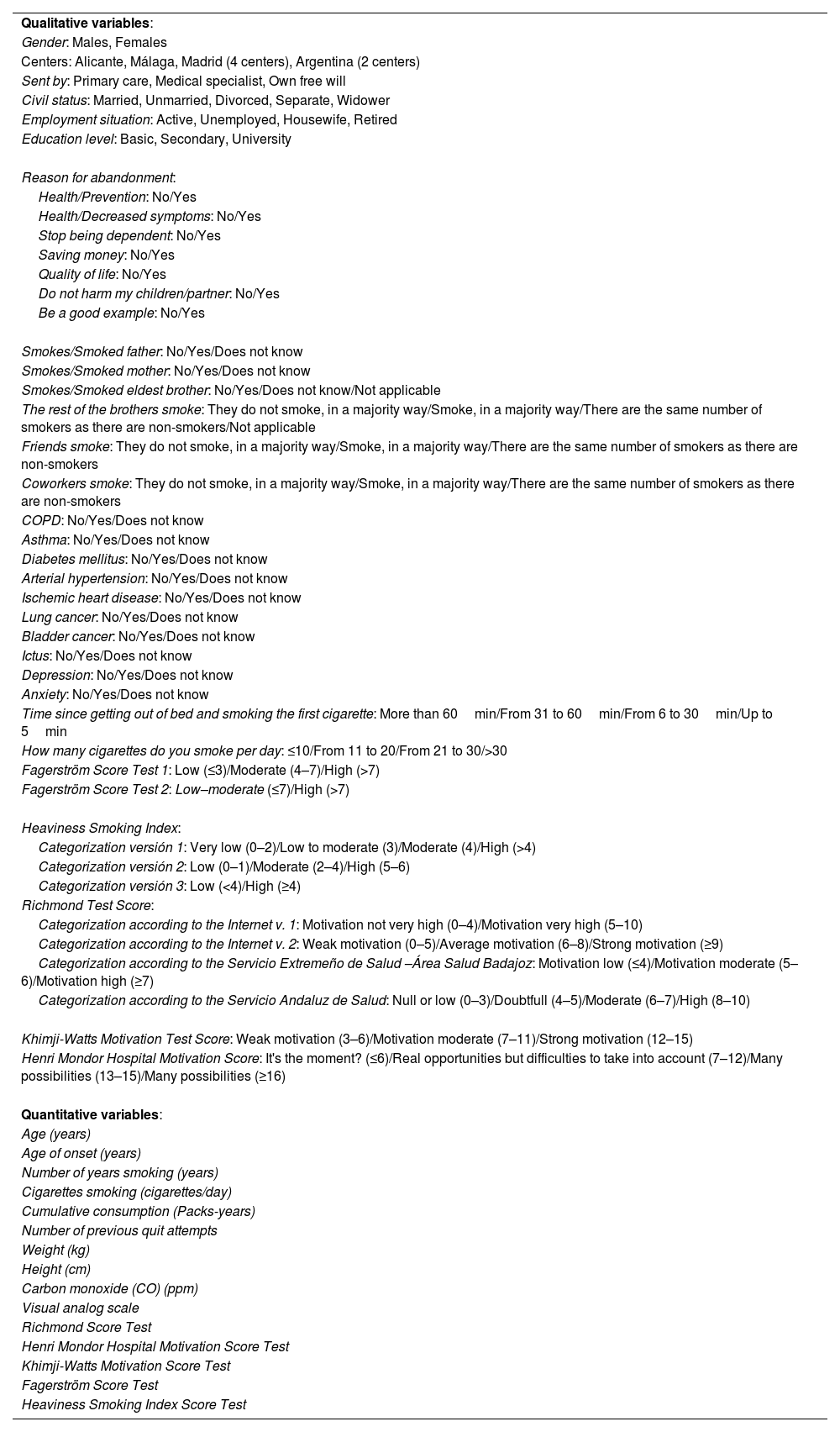
Prospective, observational, multi-center study of consecutive patients attending smoking consultations. Demographic and smoking status variables were collected (Table 1), the dependent variable was go for follow-up after the first visit, with 2 categories (Yes vs. No). The statistical analysis was descriptive and was carried out with the IBM SPSS v.22 and STATA 17 statistics programs. The joint effect of the variables that showed a significant association with the outcome variable Attended was assessed using a logistic regression model.
Collected Variables.
| Qualitative variables: |
| Gender: Males, Females |
| Centers: Alicante, Málaga, Madrid (4 centers), Argentina (2 centers) |
| Sent by: Primary care, Medical specialist, Own free will |
| Civil status: Married, Unmarried, Divorced, Separate, Widower |
| Employment situation: Active, Unemployed, Housewife, Retired |
| Education level: Basic, Secondary, University |
| Reason for abandonment: |
| Health/Prevention: No/Yes |
| Health/Decreased symptoms: No/Yes |
| Stop being dependent: No/Yes |
| Saving money: No/Yes |
| Quality of life: No/Yes |
| Do not harm my children/partner: No/Yes |
| Be a good example: No/Yes |
| Smokes/Smoked father: No/Yes/Does not know |
| Smokes/Smoked mother: No/Yes/Does not know |
| Smokes/Smoked eldest brother: No/Yes/Does not know/Not applicable |
| The rest of the brothers smoke: They do not smoke, in a majority way/Smoke, in a majority way/There are the same number of smokers as there are non-smokers/Not applicable |
| Friends smoke: They do not smoke, in a majority way/Smoke, in a majority way/There are the same number of smokers as there are non-smokers |
| Coworkers smoke: They do not smoke, in a majority way/Smoke, in a majority way/There are the same number of smokers as there are non-smokers |
| COPD: No/Yes/Does not know |
| Asthma: No/Yes/Does not know |
| Diabetes mellitus: No/Yes/Does not know |
| Arterial hypertension: No/Yes/Does not know |
| Ischemic heart disease: No/Yes/Does not know |
| Lung cancer: No/Yes/Does not know |
| Bladder cancer: No/Yes/Does not know |
| Ictus: No/Yes/Does not know |
| Depression: No/Yes/Does not know |
| Anxiety: No/Yes/Does not know |
| Time since getting out of bed and smoking the first cigarette: More than 60min/From 31 to 60min/From 6 to 30min/Up to 5min |
| How many cigarettes do you smoke per day: ≤10/From 11 to 20/From 21 to 30/>30 |
| Fagerström Score Test 1: Low (≤3)/Moderate (4–7)/High (>7) |
| Fagerström Score Test 2: Low–moderate (≤7)/High (>7) |
| Heaviness Smoking Index: |
| Categorization versión 1: Very low (0–2)/Low to moderate (3)/Moderate (4)/High (>4) |
| Categorization versión 2: Low (0–1)/Moderate (2–4)/High (5–6) |
| Categorization versión 3: Low (<4)/High (≥4) |
| Richmond Test Score: |
| Categorization according to the Internet v. 1: Motivation not very high (0–4)/Motivation very high (5–10) |
| Categorization according to the Internet v. 2: Weak motivation (0–5)/Average motivation (6–8)/Strong motivation (≥9) |
| Categorization according to the Servicio Extremeño de Salud –Área Salud Badajoz: Motivation low (≤4)/Motivation moderate (5–6)/Motivation high (≥7) |
| Categorization according to the Servicio Andaluz de Salud: Null or low (0–3)/Doubtfull (4–5)/Moderate (6–7)/High (8–10) |
| Khimji-Watts Motivation Test Score: Weak motivation (3–6)/Motivation moderate (7–11)/Strong motivation (12–15) |
| Henri Mondor Hospital Motivation Score: It's the moment? (≤6)/Real opportunities but difficulties to take into account (7–12)/Many possibilities (13–15)/Many possibilities (≥16) |
| Quantitative variables: |
| Age (years) |
| Age of onset (years) |
| Number of years smoking (years) |
| Cigarettes smoking (cigarettes/day) |
| Cumulative consumption (Packs-years) |
| Number of previous quit attempts |
| Weight (kg) |
| Height (cm) |
| Carbon monoxide (CO) (ppm) |
| Visual analog scale |
| Richmond Score Test |
| Henri Mondor Hospital Motivation Score Test |
| Khimji-Watts Motivation Score Test |
| Fagerström Score Test |
| Heaviness Smoking Index Score Test |
COPD: chronic obstructive pulmonary disease; min: minutes; v.: versión.
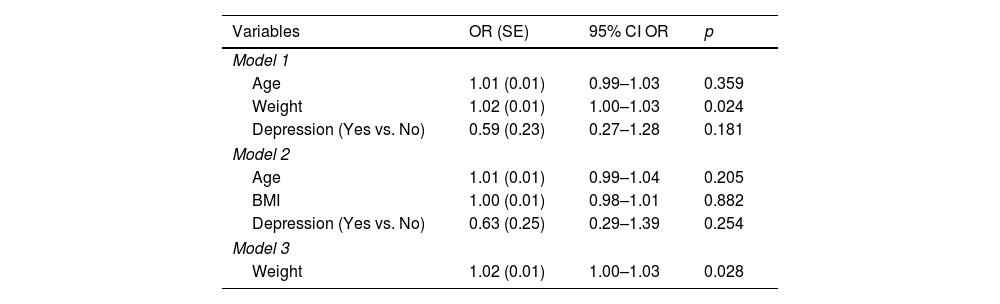
375 subjects were included, 195 females (52.0%), with a mean age of 51.7 (10.7 SD), with no differences between sexes, of whom 98 (26.1%) did not attend after the first visit. Of the qualitative variables, only depression showed an association with the dependent variable. Subjects with depression attended subsequent follow-up visits more frequently by 8.6% (3.5 SD) (95% CI 0.8–16.3). Of the quantitative variables only age, weight and body mass index (BMI) showed a statistically significant association with the dependent variable. Subjects who did not attend after the first visit were 2.8 years (1.4 SD) (95% CI 0.1–5.5) older and were slightly more obese (4.4kg [1.9 SD], 95% CI 0.5–8.2) than subjects who continued follow-up. In the multivariate analysis, only the weight showed an association between the probability of continuing or not with the follow-up visits (Table 2). For every kilogram of weight gain, the probability of not attending the second visit is multiplied by 1.02 (increases by 2%). We conclude that a statistically significant association was only found with the probability of attending or not attending the following visits in a smoking treatment program with the weight variable; so that, as the subject's weight increases, the probability of not attending the first follow-up visits in the treatment of the subject's smoking increases.
Logistic Regression Models That Relate the Dependent Variable «Attended After the First Visit» and the Statistically Significant Independent Variables in the Bivariate Analysis.
| Variables | OR (SE) | 95% CI OR | p |
|---|---|---|---|
| Model 1 | |||
| Age | 1.01 (0.01) | 0.99–1.03 | 0.359 |
| Weight | 1.02 (0.01) | 1.00–1.03 | 0.024 |
| Depression (Yes vs. No) | 0.59 (0.23) | 0.27–1.28 | 0.181 |
| Model 2 | |||
| Age | 1.01 (0.01) | 0.99–1.04 | 0.205 |
| BMI | 1.00 (0.01) | 0.98–1.01 | 0.882 |
| Depression (Yes vs. No) | 0.63 (0.25) | 0.29–1.39 | 0.254 |
| Model 3 | |||
| Weight | 1.02 (0.01) | 1.00–1.03 | 0.028 |
OR: odds ratio; SE: standard error; 95% CI OR: confidence interval 95% for OR; p: degree of significance; vs.: versus; BMI: body mass index.
In a recent study,3 in which they evaluated the factors associated with adherence to treatment and success in quitting smoking in a smoking clinic found that an increase in the number of visits to the clinic, the absence of side effects with the medication and the use of varenicline were each associated with greater adherence to treatment (p<0.001) and being in the treatment-adherent group was associated with quit success (OR=3.01, 95% CI 1.88–4.81, p=0.001). These findings indicate that for successful outcomes of smoking cessation interventions, patients’ adherence to cessation program plays the key role. In another study,4 that have evaluated the effect of short message service (SMS) via telephone in the compliance of patients with smoking cessation clinics follow-up visits and smoking cessation success found that there was increased success of smoking cessation in patients coming to control visits (in this study smoking cessation rate of the patients invited by SMS but who did not attend any control visits was 19.1%, and it was 34.5% in patients coming to a control visit at least once [p=0.001]). In another study,5 smokers who had more than one smoking cessation outpatient visit or seen by physicians who, on average, delivered more than one smoking cessation consultations per week also led to a higher success rate. So, authors suggest that physicians should put more efforts and encourage follow-up visits for some smokers by knowing their characteristics at the first visit.
The question is, why do these smokers who came to the consultation to quit smoking only go to the first visit and do not continue the treatment? Factors that could be the cause of not returning to the consultation could be that the patients are not really motivated to quit, relapsed into consumption or were not able to quit smoking. Motivation to quit is important because the treatments that have been shown to help subjects stop smoking do not work as well in smokers who are not highly motivated,6 and it no depends on who refers the subject.7 About the theory of motivation, we can distinguish into the intrinsic motivation, which refers to doing something because it is inherently interesting or enjoyable, and extrinsic motivation, which refers to doing something because it leads to a separable outcome.8 Benson et al.9 found that the desire to quit be a factor in attendance, however, intrinsic motivation seemed to be an equally important factor in attendance and these two factors were not typically mentioned together, so this factor seems to be as important as a desire to quit. Intrinsic motivation is defined as the doing of an activity for its inherent satisfactions rather than for some separable consequence, so intrinsic motivation seems to be an important motivator of continued attendance. Motivation to attend behavioural support, as distinct from motivation to quit smoking, is an important factor in attendance of smoking cessation and increasing motivation to attend may help to prevent participants missing sessions.8,9
Between the causes for relapsed into consumption has been found: insufficient willpower and self-discipline, contact with smokers, exposure to stressful situations, lack of family support, weight gain, and insufficient improvement in one's mental and physical well-being, enjoyable social events, in addition to professional life, critical events, and encouragement to smoke from family members.10 As we found a recurring problem mentioned in connection with relapsing to smoking was weight gain, which was perceived as a deterioration of their physical appearance and besides weight gain is also a barrier to attempting to cease smoking.10,11 It is well known that smokers who make a serious attempt to quit smoking with pharmacological therapy gain less weight in the process.12 Perhaps, those who gain weight and therefore do not attend the follow-ups visits do not follow the pharmacological treatments, nor do they follow the dietary advice or not are subjected to strict control of their weight evolution throughout the smoking cessation process.12–14
Regarding the beliefs of why smokers believe that they are not capable of quitting, they have been indicated, addiction, habit, willpower and motivation, as causes of the inability to stop smoking.10
The present work has several limitations: 1. The findings were obtained using smokers who voluntarily attended smoking cessation clinics, and the surveys were performed in different scenarios and geographical locations, which might not reflect the general population. 2. The use of questionnaires in patients is not always accurate. 3. The sampling strategy and the dimensions of the sample may not have sufficient statistical strength to identify differences. This variability could lead to other results.
In conclusion, weight gain was the only differential characteristic found between those who only attended the first visit to quit smoking and those who completed the treatment program. We have to increase focus on interventions targeting weight gain while quitting smoking cause as we know it is a barrier for get abstinence. Besides we must analyze in more depth the causes related to the lack of adherence to a smoking cessation program.
FundingThe project was funded by an unrestricted grant from The Spanish Society of Pneumology and Thoracic Surgery 2013 (SEPAR 46/2013).
Authors’ ContributionsAll authors have introduced patients to the study in our smoking cessation clinics. JIG-O: Conception and design of the study, writing the core content of the study, analysis and interpretation of data, drafting the article and revising it critically for important intellectual content. JFP-L: Statistical analysis and interpretation of data, preparation and critical review of the manuscript. SA-S, SS-R, MG-R, MAM-M, LL-A, DB, RP, SL, IC-A, and CAJ-R: critical review of the manuscript. All authors approve the current version of the manuscript.
Conflicts of InterestJIG-O has received honoraria for lecturing, scientific advice, participation in clinical studies or writing for publications for the following (alphabetical order): AstraZeneca, Chiesi, Esteve, Faes, Gebro, Menarini, and Pfizer. CAJR has received honoraria for advisory and talks for pharmaceutical companies trading smoking cessation medications. LL-A has received honoraria for lecturing, participation in clinical studies and writing for publications for the following (alphabetical order): AstraZeneca, Boehringer, Chiesi, Esteve, Ferrer, Grifols, GSK, Menarini, Novartis, and Pfizer. SS-R has received honoraria for lecturing, participation in clinical studies and writing for publications for the following (alphabetical order): Boehringer, Esteve, Pfizer, and Sandoz. The rest of the authors have no conflicts of interest.