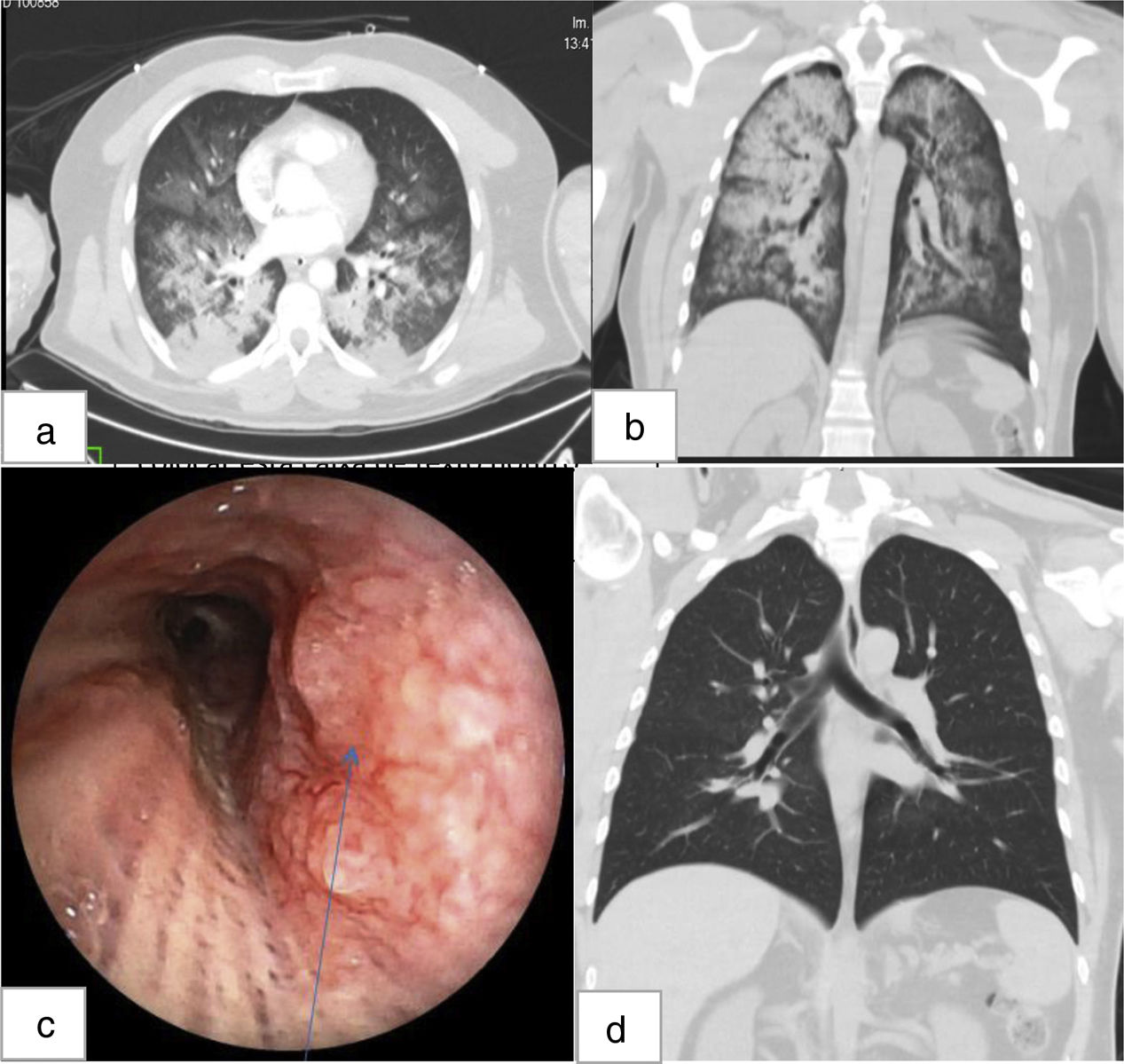
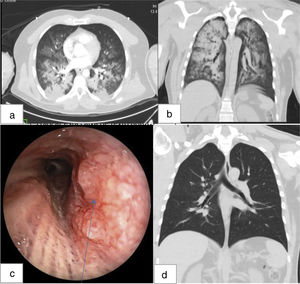
We report a case of a 38 years old male, smoker, without previous known pathologies and any assumed toxic habits. Pre-operative tests including coagulation, were normal. He was submitted to supraspinatus raffia through shoulder arthroscopy, under balanced general anesthesia with inhaled Sevoflurane. Orotracheal intubation (OI), performed with Macintosh laryngoscope, was smooth and easy with a 7.5mm reinforced tube. No trauma or other complications were reported during OI or surgery. Two minutes after extubation, the patient presented laryngospasm, desaturation, and massive hemoptysis. He was immediately reintubated and admitted to Intensive Care Unit, where a first diagnostic bronchofibroscopy was performed, reporting distal massive hemorrhage without any visible focus or trauma in the airways. Thorax Computed Tomography showed diffuse alveolar hemorrhage (DAH) and excluded pulmonary embolism (PE). After five days with OI, a new bronchofibroscopy showed a lesion in the posterior wall of trachea. An autoimmune screening was performed and excluded vasculitis. Patient was discharged after two weeks and a third bronchofibroscopy was made after one month, displaying good evolution.
In this case there were several different diagnostic possibilities: Airway trauma, PE, autoimmune diseases, negative pressure pulmonary edema (NPPE) and Sevoflurane induced DAH. The lesion found in the second bronchofibroscopy was not seen in the first exam, which could be related to the use of high pressure endotracheal cuff, during the five days of OI. In the other hand, in the first bronchofibroscopy, the presence of an orotracheal tube may have hindered the observation of tracheal trauma. NPPE after an upper airway obstruction such as laryngospasm is another plausible hipothesys.1 Still, preexisting pulmonary damage from smoking and administration of the irritating inhaled anesthetic Sevoflurane, could lead to DAH.1 There are, in literature, a few case reports1,2 of hemoptysis related to the association of inhaled Sevoflurane and NPPE after extubation, and this might be another one (Fig. 1).
Even though we didn’t find an unequivocal diagnosis, with this case we wanted to highlight the chance of Sevoflurane induced DAH or NPPE as hypothesis for immediate postoperative hemoptysis.