Current evidence on the diagnostic yield and safety of pleural cryobiopsy (CB) is based on a series of heterogeneous studies with limited cohorts. A pooled analysis of these studies could improve the evidence and contribute to a better understanding of this new technique.
MethodologyWe performed a systematic review and meta-analysis of published studies that included data on the yield and diagnostic safety of pleural CB compared with procedures performed using conventional flexible forceps. The heterogeneity of the analysis was evaluated by determining the I2 index, while study quality was measured with the QUADAS-2 tool.
ResultsSeven studies involving 356 patients were used for the final evaluation. In 55.6%, the etiology of the pleural effusion was malignant, 61.1% of which were lung cancer. The diagnostic yield of pleural CB was 95% (95% CI 92-97) vs. 91% (95% CI 87-94) with conventional flexible forceps (P = .019). Mild bleeding was reported in 67% of CB procedures (95% CI 62-72) compared with 85% of conventional flexible forceps procedures (95% CI 79-90) (P < .001). CB specimens were larger, and fewer artifacts were detected. A pooled analysis of the detection of molecular changes could not be performed. Heterogeneity was moderate to high, although the quality of the studies was acceptable.
ConclusionsPleural CB is a safe technique with a high yield for etiological diagnosis of pleural effusion, and larger specimens with fewer artifacts are obtained. Molecular determinations should be investigated in more depth.
La evidencia disponible sobre la rentabilidad diagnóstica y la seguridad de la criobiopsia pleural (CB) está basada en una serie de estudios que presentan casuísticas limitadas y diferentes diseños. Un análisis agrupado de los mismos podría mejorarla y aportar una visión global de esta novedosa técnica.
MetodologíaRevisión sistemática y metaanálisis de los estudios publicados en los que se incluían resultados sobre rendimiento y seguridad diagnóstica de la CB pleural comparados con la realizada con pinzas flexibles convencionales. Se evaluó la heterogeneidad del análisis determinando el índice I2 y la calidad de los estudios mediante la herramienta QUADAS-2.
ResultadosPara la evaluación final se incluyeron 7 trabajos con 356 pacientes. En el 55,6% el derrame pleural fue de etiología maligna, 61,1% de ellos cáncer de pulmón. La rentabilidad diagnóstica de la CB pleural fue del 95% (IC 95% 92-97) frente al 91% (IC 95% 87-94) con las pinzas flexibles convencionales (p = 0,019). Se describió sangrado leve en el 67% (IC 95% 62-72) de las CB frente al 85% (IC 95% 79-90) de las realizadas con pinzas flexibles convencionales (p < 0,001). El tamaño de las muestras de CB fue superior y el porcentaje de artefactos menor. No fue posible realizar un análisis agrupado en la evaluación de la detección de alteraciones moleculares. La heterogeneidad observada fue moderada-alta, aunque la calidad de los estudios fue aceptable.
ConclusionesLa CB pleural es una técnica segura y con elevada rentabilidad para el diagnóstico etiológico del derrame pleural, obteniéndose muestras de mayor tamaño con menos artefactos. Son necesarios más estudios sobre determinaciones moleculares.
Medical thoracoscopy (MT), also called local anesthetic thoracoscopy or pleuroscopy, is a minimally invasive technique used to examine the pleural space and obtain targeted biopsies of the parietal pleura1–3. It is considered the technique of choice in the diagnosis of pleural effusion (PE) with criteria of exudate of uncertain etiology4,5. In a review published in 2010 that included several case series, MT with pleural biopsy using conventional forceps had a sensitivity of 92.6% for the diagnosis of malignant PE3. MT can be performed with a rigid thoracoscope or a semi-rigid pleuroscope1–3. The results of the major studies comparing diagnostic yield between rigid and semi-rigid MT showed no significant differences between the two techniques6–8. However, when thoracoscopy is performed with a semi-rigid pleuroscope, 6-8 biopsies should be obtained due to its smaller size1–3. The use of this technique is now expanding and it is considered safe, with a rate of serious complications of less than 5%1,3,9,10. However, the reported diagnostic efficacy and safety have not been uniform over all studies, especially in the case of malignant pleural involvement3,9,10. This factor, in addition to a growing need for larger histological samples for the molecular characterization of tumors11, has promoted the development of new pleural biopsy techniques such as cryobiopsy (CB). CB has been described as a safe endoscopic technique with a high diagnostic yield, initially in the diagnosis of endobronchial tumors and more recently in the study of interstitial lung disease12,13. Its validity and safety in the study of PE have been confirmed by several groups, although these studies have reduced case numbers and different designs14, which limits, at least individually, the value of their scientific evidence. Indeed, these new pleural biopsy techniques are not included in the clinical practice guidelines4,5.
In this setting, then, it seems an appropriate time to review the available evidence on this topic by performing a systematic pooled analysis of the published literature on the diagnostic yield and safety of parietal pleural CB in the diagnosis of PE versus conventional flexible biopsy forceps (FBF), and to evaluate some aspects such as the implementation of this novel diagnostic technique in routine clinical practice. This study was carried out with these objectives.
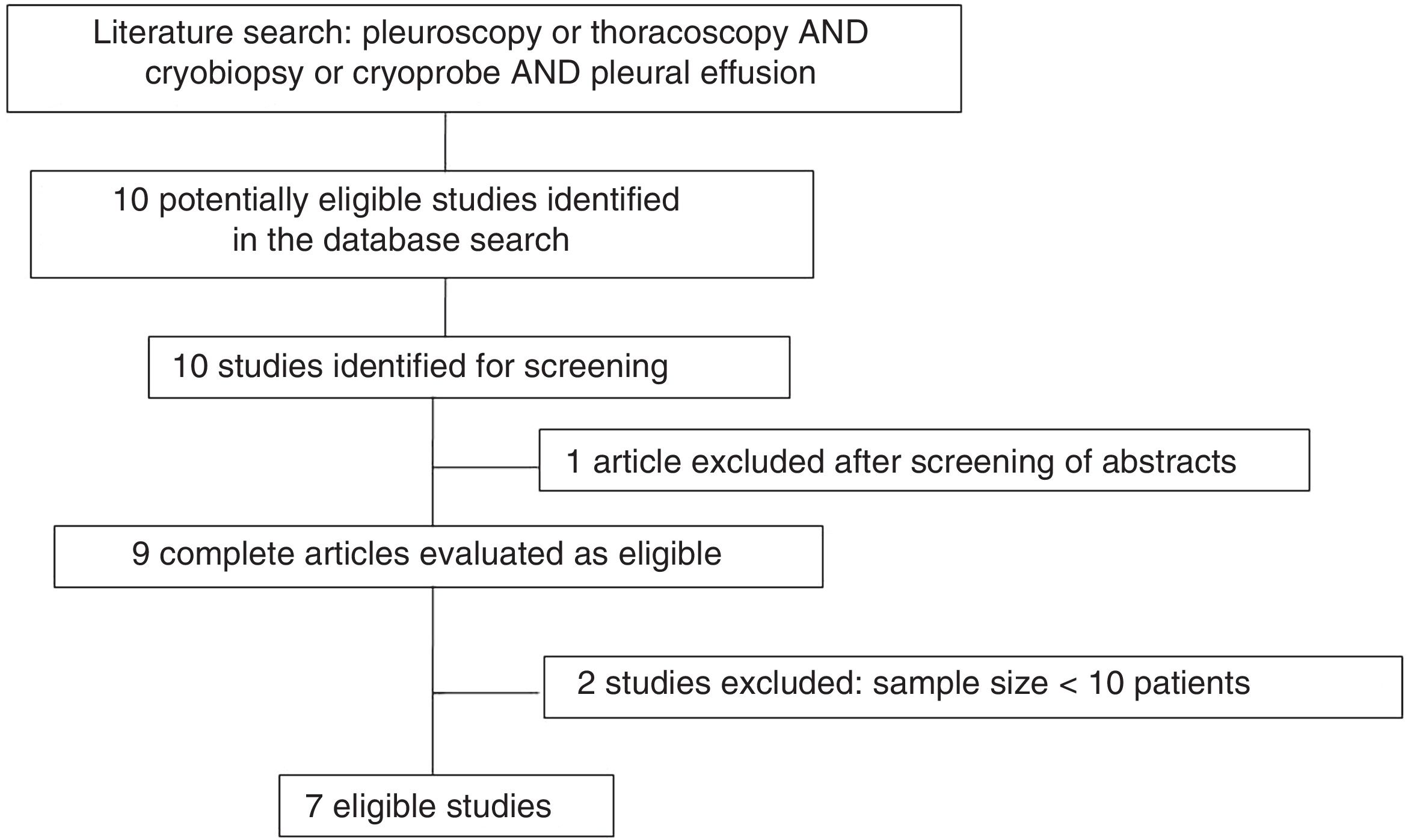
MethodsA systematic review and subsequent meta-analysis of existing evidence was performed from January 2010 to May 2019 following the recommendations of the PRISMA statement for reviews and meta-analyses. A search of the literature was conducted in the electronic databases PubMed (MEDLINE), Embase, The Cochrane Library, Web of Science, and TheClinicalTrials.gov for pleural CB during MT. The search terms were: «semi-rigid pleuroscopy», «rigid thoracoscopy», «medical thoracoscopy», «cryobiopsy», «pleural effusion», «cryoprobe biopsy». A manual search was also performed to capture studies or reviews that were not electronically selected. We included meta-analyses and systematic reviews, randomized, cohort, case-control, and case-series studies that described the yield of pleural CB in the study of PE during TM. Studies with fewer than 10 patients and isolated clinical cases were excluded. The search was not limited to any language.
The systematic review was complemented by analyzing the list of references of the studies included and the main clinical practice guidelines.
Two authors (MBR and CMR) independently selected abstracts to determine their eligibility and excluded studies that did not meet the inclusion criteria. Discrepancies were resolved through discussion with a third author (AFV). Eligible studies were retrieved in complete format and reviewed independently by 2 authors (MBR and CMR).
Relevant information from each of the studies was collected from evidence tables.
The main variables analyzed were the diagnostic yield of parietal pleura samples obtained by cryoprobe versus those obtained with FBF. Yield was calculated by dividing the number of subjects in whom biopsies showed definitive histological findings (including nonspecific pleuritis) for the final diagnosis of the patient. Complications, such as degree of bleeding from CB or FBF and procedure-related pain were also recorded as a primary variable. Bleeding was considered mild when it was self-limiting, moderate when the use of topical vasoactive drugs (adrenaline) was required, and severe when intervention with electrocautery or argon plasma was necessary1,3.
Secondary variables were the mean size of the CB (in mm), the depth of the sample, the artifact level, defined as crush affecting more than 25% of the sample area or interpretability, and degree of integrity14.
With respect to the procedure, the cryoprobe freeze time (in seconds) and duration were analyzed.
CB molecular diagnosis yield in malignant PE due to lung cancer was also analyzed as a secondary variable.
The clinical and epidemiological characteristics of the patients (age, sex) and the specific etiology of benign and malignant PE were also described in general terms.
The quality of the studies was assessed according to the levels of evidence and grades of recommendation described in the scientific guidelines15 and 27 items from the PRISMA statement for systematic reviews and meta-analysis were verified for the drafting of this manuscript16. The results of the QUADAS-2 evaluation of all the studies included in this systematic review and meta-analysis were also summarized.
The proportions and 95% confidence intervals (95% CI) of diagnostic yield and complications, particularly bleeding caused by the cryoprobe and FBF, were estimated in each study and jointly. This information was displayed using forest plots drawn up with the R 3.4.2. "meta" library statistical software package. The heterogeneity between the results of the studies was evaluated using the Cochran Q statistical test and the I2 statistic. Significant heterogeneity was considered if I2 was >50% and/or p < 0.1.
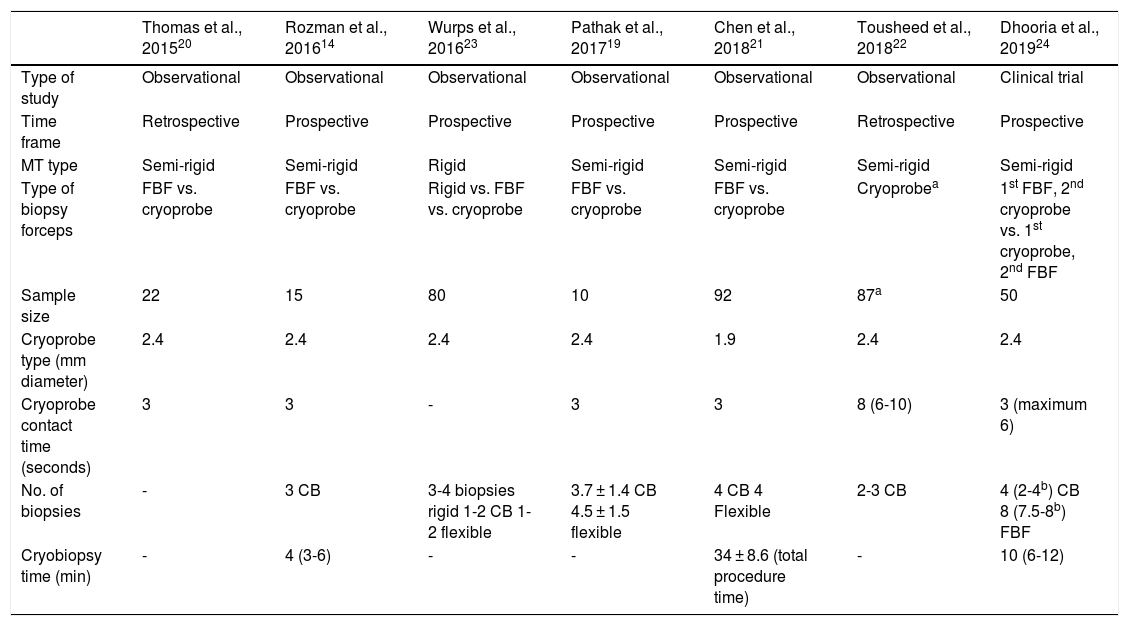
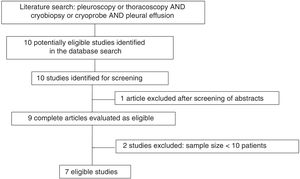
ResultsOverview of the reviewed studiesWe identified 10 studies potentially eligible for screening. One article was excluded after reading the abstract and the complete texts of 9 were read. After careful review of the complete text, 2 studies were excluded because they included less than 10 patients17,18, so 7 papers were finally included in the pooled analysis14,19–24. Fig. 1 shows the workflow diagram and Table 1 describes the general characteristics and procedural aspects of the studies. Four were prospective observational studies14,19,21,23, 2 retrospective observational studies20,22, and only 1 was a randomized controlled trial24 (Table 1). All were performed in a single center. No systematic reviews or meta-analyses were found on the subject.
Study design and characteristics of medical thoracoscopy with cryoprobe
| Thomas et al., 201520 | Rozman et al., 201614 | Wurps et al., 201623 | Pathak et al., 201719 | Chen et al., 201821 | Tousheed et al., 201822 | Dhooria et al., 201924 | |
|---|---|---|---|---|---|---|---|
| Type of study | Observational | Observational | Observational | Observational | Observational | Observational | Clinical trial |
| Time frame | Retrospective | Prospective | Prospective | Prospective | Prospective | Retrospective | Prospective |
| MT type | Semi-rigid | Semi-rigid | Rigid | Semi-rigid | Semi-rigid | Semi-rigid | Semi-rigid |
| Type of biopsy forceps | FBF vs. cryoprobe | FBF vs. cryoprobe | Rigid vs. FBF vs. cryoprobe | FBF vs. cryoprobe | FBF vs. cryoprobe | Cryoprobea | 1st FBF, 2nd cryoprobe vs. 1st cryoprobe, 2nd FBF |
| Sample size | 22 | 15 | 80 | 10 | 92 | 87a | 50 |
| Cryoprobe type (mm diameter) | 2.4 | 2.4 | 2.4 | 2.4 | 1.9 | 2.4 | 2.4 |
| Cryoprobe contact time (seconds) | 3 | 3 | - | 3 | 3 | 8 (6-10) | 3 (maximum 6) |
| No. of biopsies | - | 3 CB | 3-4 biopsies rigid 1-2 CB 1-2 flexible | 3.7 ± 1.4 CB 4.5 ± 1.5 flexible | 4 CB 4 Flexible | 2-3 CB | 4 (2-4b) CB 8 (7.5-8b) FBF |
| Cryobiopsy time (min) | - | 4 (3-6) | - | - | 34 ± 8.6 (total procedure time) | - | 10 (6-12) |
CB: cryobiopsy; FBF: flexible biopsy forceps; MT: medical thoracoscopy.
In all studies, an interventional pulmonologist performed MT in a technical room with local anesthesia and mild-moderate sedation. Semi-rigid pleuroscopies were performed with the Olympus LTF-160 semi-rigid pleuroscope (Olympus, Tokyo, Japan), with a working channel with an internal diameter of 2.8 mm. In only 1 study was a rigid 11 mm thoracoscope used (Storz, Tuttlingen, Germany)23. CBs in each patient were performed in selected areas of the parietal pleura suspected of malignancy, obtained using a 2.4 mm flexible cryoprobe (Erbokryo CA, Erbe, Germany). A 1.9 mm probe was used in only 1 study21. The cryoprobe tip was placed over the area of the parietal pleura to be biopsied, and was activated at −89 °C for a minimum of 3 s and a maximum of 10 s (Table 1). The number of CBs ranged from 2 to 4 (Table 1). The duration of the MT could not be estimated, as most of the studies included did not record the mean time of the procedure.
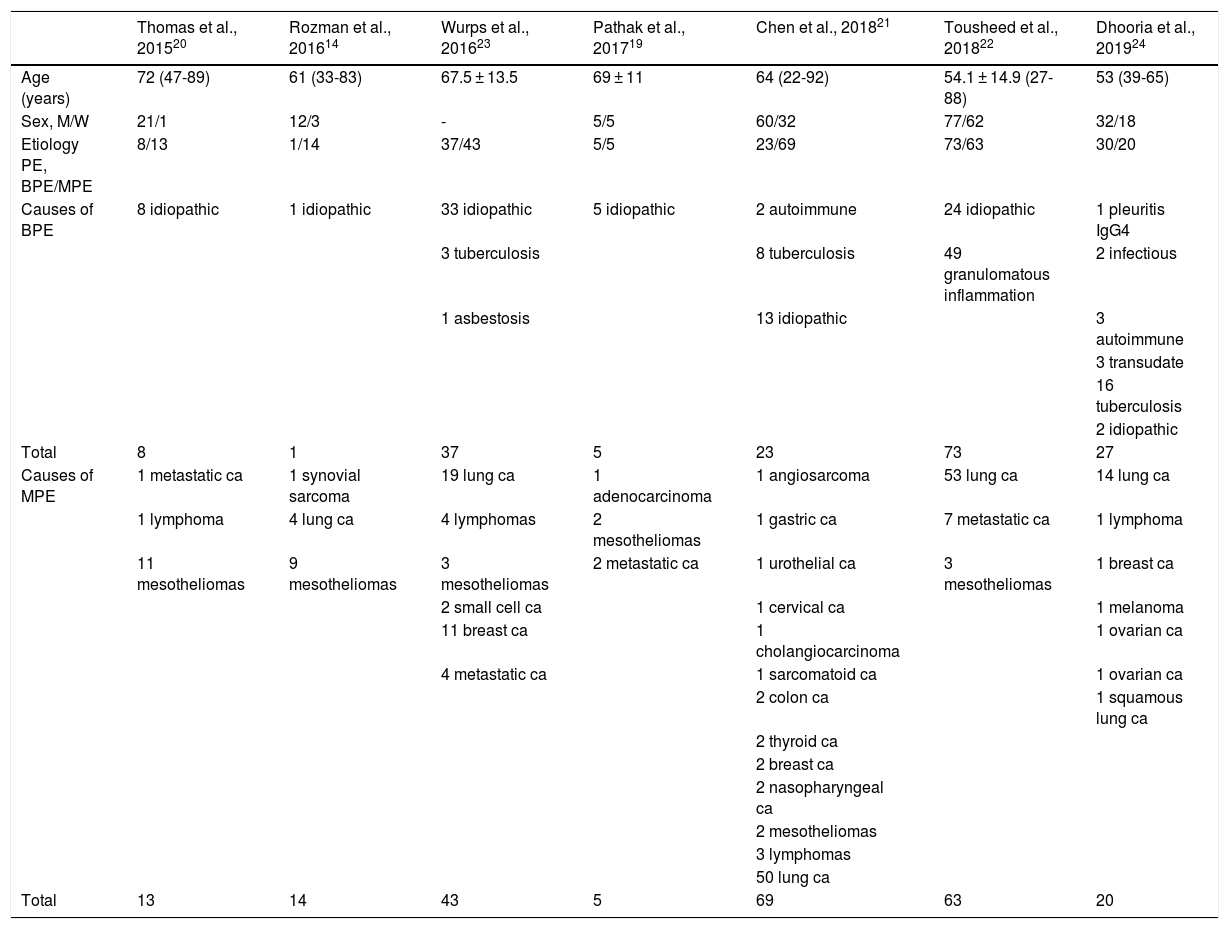
Table 2 summarizes the clinical and epidemiologic characteristics and etiology of PE in the subjects included in the studies. Most were men (207, 75%), all were adults, and ages ranged from 22 to 92 years. A total of 408 patients were included, and CB was performed in 356.
Clinical-epidemiological characteristics of all patients included in the studies of this revision.
| Thomas et al., 201520 | Rozman et al., 201614 | Wurps et al., 201623 | Pathak et al., 201719 | Chen et al., 201821 | Tousheed et al., 201822 | Dhooria et al., 201924 | |
|---|---|---|---|---|---|---|---|
| Age (years) | 72 (47-89) | 61 (33-83) | 67.5 ± 13.5 | 69 ± 11 | 64 (22-92) | 54.1 ± 14.9 (27-88) | 53 (39-65) |
| Sex, M/W | 21/1 | 12/3 | - | 5/5 | 60/32 | 77/62 | 32/18 |
| Etiology PE, BPE/MPE | 8/13 | 1/14 | 37/43 | 5/5 | 23/69 | 73/63 | 30/20 |
| Causes of BPE | 8 idiopathic | 1 idiopathic | 33 idiopathic | 5 idiopathic | 2 autoimmune | 24 idiopathic | 1 pleuritis IgG4 |
| 3 tuberculosis | 8 tuberculosis | 49 granulomatous inflammation | 2 infectious | ||||
| 1 asbestosis | 13 idiopathic | 3 autoimmune | |||||
| 3 transudate | |||||||
| 16 tuberculosis | |||||||
| 2 idiopathic | |||||||
| Total | 8 | 1 | 37 | 5 | 23 | 73 | 27 |
| Causes of MPE | 1 metastatic ca | 1 synovial sarcoma | 19 lung ca | 1 adenocarcinoma | 1 angiosarcoma | 53 lung ca | 14 lung ca |
| 1 lymphoma | 4 lung ca | 4 lymphomas | 2 mesotheliomas | 1 gastric ca | 7 metastatic ca | 1 lymphoma | |
| 11 mesotheliomas | 9 mesotheliomas | 3 mesotheliomas | 2 metastatic ca | 1 urothelial ca | 3 mesotheliomas | 1 breast ca | |
| 2 small cell ca | 1 cervical ca | 1 melanoma | |||||
| 11 breast ca | 1 cholangiocarcinoma | 1 ovarian ca | |||||
| 4 metastatic ca | 1 sarcomatoid ca | 1 ovarian ca | |||||
| 2 colon ca | 1 squamous lung ca | ||||||
| 2 thyroid ca | |||||||
| 2 breast ca | |||||||
| 2 nasopharyngeal ca | |||||||
| 2 mesotheliomas | |||||||
| 3 lymphomas | |||||||
| 50 lung ca | |||||||
| Total | 13 | 14 | 43 | 5 | 69 | 63 | 20 |
BPE: benign pleural effusion; ca: carcinoma; M: men; MPE: malignant pleural effusion; W: women.
Data are expressed as median (range) or mean ± standard deviation.
The most frequent cause of PE was malignant PE, with a total of 227 (55.6%) cases, of which 141 (61.1%) were PE caused by non-small cell lung cancer (Table 2).
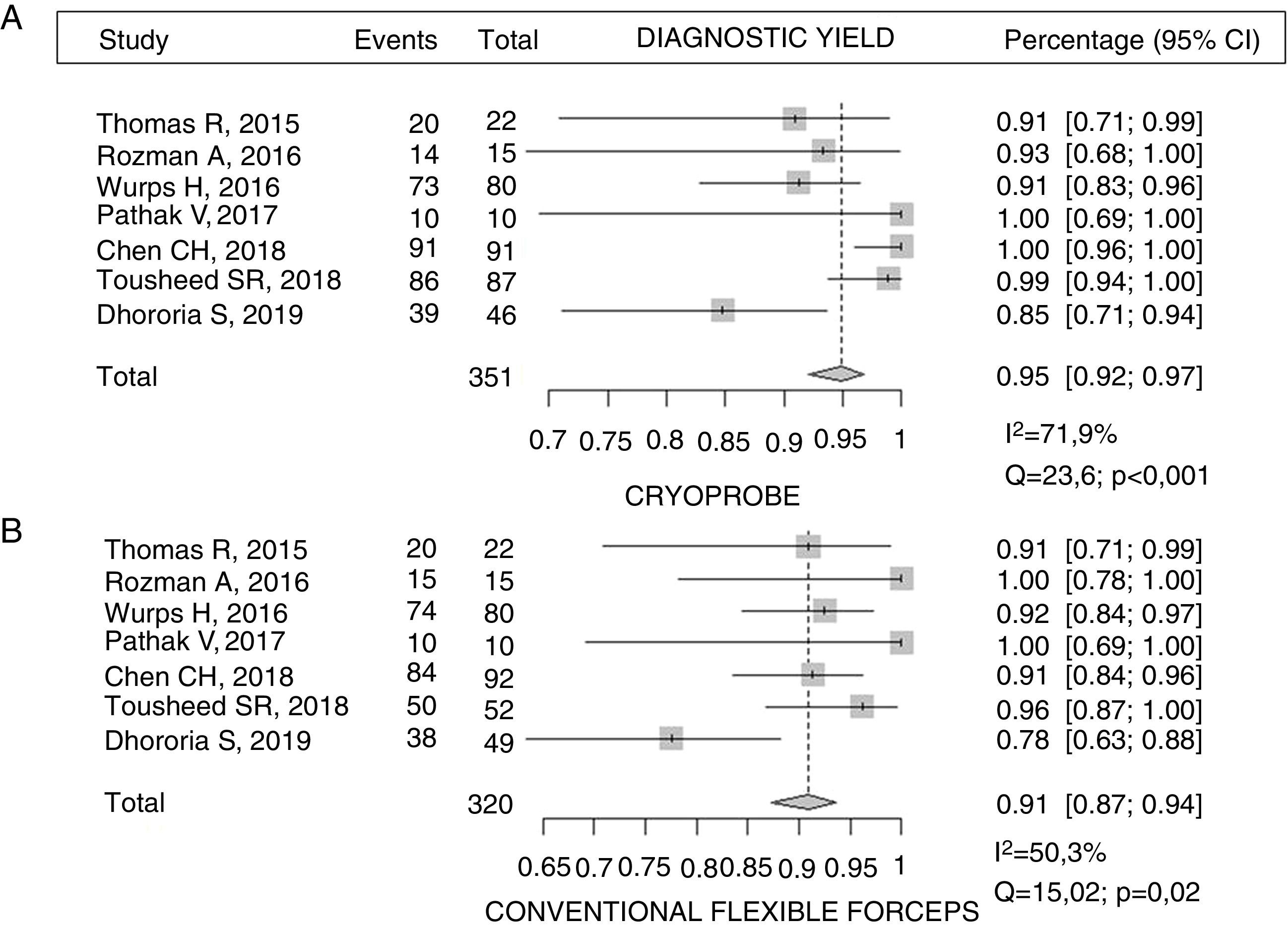
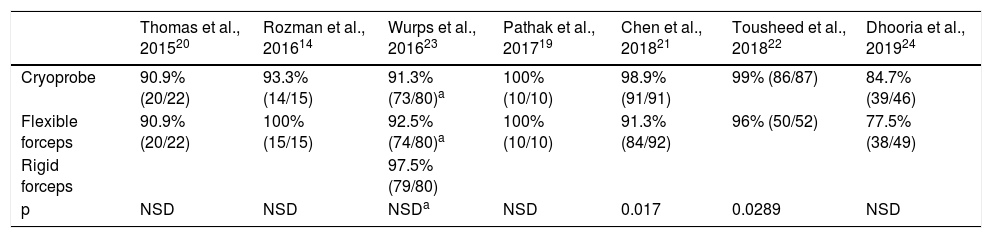
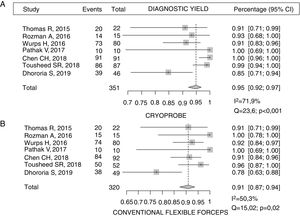
Diagnostic yieldTable 3 shows the diagnostic yield of the different samples obtained by cryoprobe and FBF. The diagnostic yield of rigid forceps in the only study that used a rigid thoracoscope is also described23. Chen et al.21 reported a yield for CB of almost 99% compared to 91% for FBF (p = 0.017). Similar results were described by Tousheed et al.22, 99% versus 96% (p = 0.02), although that study compared the results of CB with a historical cohort of MT performed with FBF22. The diagnostic yield of pleural CB obtained in this pooled analysis was 95% (95% CI 92-97) versus 91% for FBF (95% CI 87-94), with a statistically significant difference (p = 0.019), but the results showed moderate-high heterogeneity, due to the low sample size (Fig. 2). With respect to one of the secondary objectives of the meta-analysis, only 2 studies analyzed the possibility of establishing a molecular characterization of non-small cell lung cancer from the CB14,22. In the first, which included 14 cases of malignant PE (4 lung adenocarcinomas), EGFR gene mutations were analyzed in all samples14. In the second study, which included 139 patients, 87 of whom underwent CB, 29 were diagnosed with non-small cell lung cancer, and all samples were valid for the molecular study22, although none of these studies analyzed the yield of FBF for DNA analysis in tumor samples.
Diagnostic yield of pleural cryobiopsy versus with conventional forceps biopsy of the parietal pleura
| Thomas et al., 201520 | Rozman et al., 201614 | Wurps et al., 201623 | Pathak et al., 201719 | Chen et al., 201821 | Tousheed et al., 201822 | Dhooria et al., 201924 | |
|---|---|---|---|---|---|---|---|
| Cryoprobe | 90.9% (20/22) | 93.3% (14/15) | 91.3% (73/80)a | 100% (10/10) | 98.9% (91/91) | 99% (86/87) | 84.7% (39/46) |
| Flexible forceps | 90.9% (20/22) | 100% (15/15) | 92.5% (74/80)a | 100% (10/10) | 91.3% (84/92) | 96% (50/52) | 77.5% (38/49) |
| Rigid forceps | 97.5% (79/80) | ||||||
| p | NSD | NSD | NSDa | NSD | 0.017 | 0.0289 | NSD |
NDS: no significant differences.
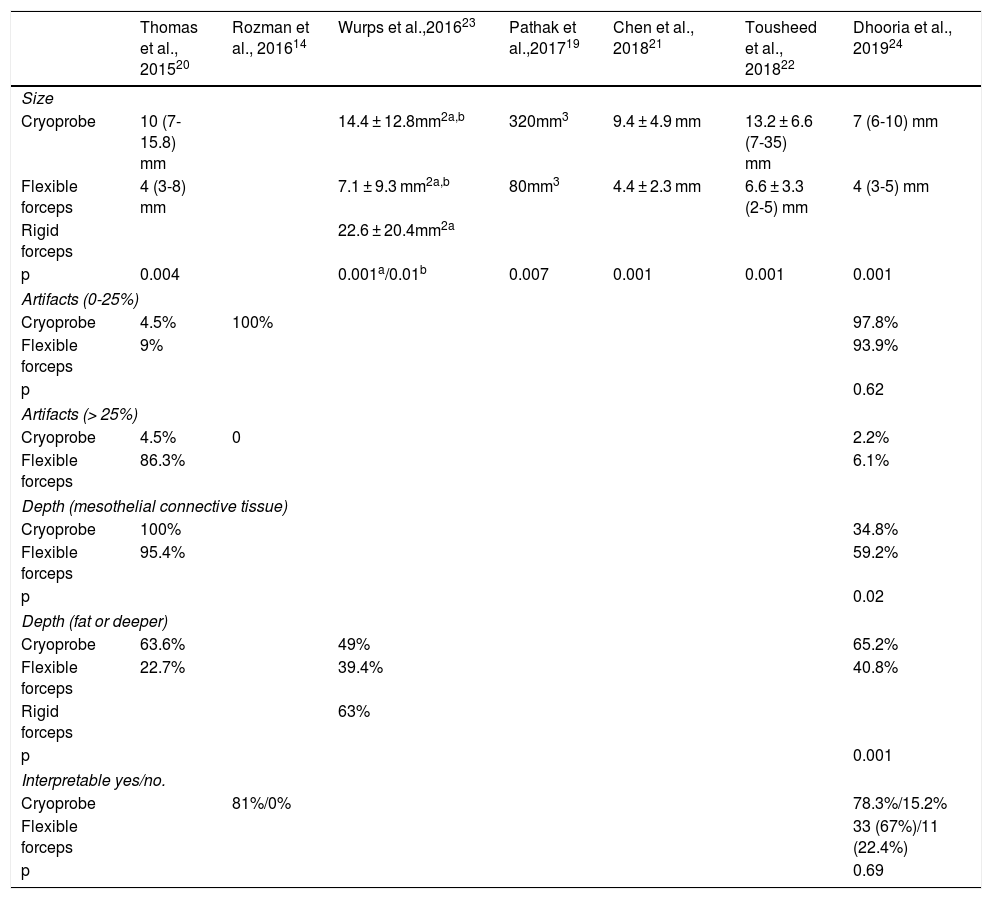
Table 4 describes the average size of the CB (in mm or mm2), the depth of the samples obtained, and artifacts. CBs measured 7-35 mm, significantly larger than the samples obtained by FBF independently in 6 of the 7 studies that recorded this variable in their results19–24.
Characteristics of the samples obtained according to the type of forceps used: cryoprobe vs. conventional forceps
| Thomas et al., 201520 | Rozman et al., 201614 | Wurps et al.,201623 | Pathak et al.,201719 | Chen et al., 201821 | Tousheed et al., 201822 | Dhooria et al., 201924 | |
|---|---|---|---|---|---|---|---|
| Size | |||||||
| Cryoprobe | 10 (7-15.8) mm | 14.4 ± 12.8mm2a,b | 320mm3 | 9.4 ± 4.9 mm | 13.2 ± 6.6 (7-35) mm | 7 (6-10) mm | |
| Flexible forceps | 4 (3-8) mm | 7.1 ± 9.3 mm2a,b | 80mm3 | 4.4 ± 2.3 mm | 6.6 ± 3.3 (2-5) mm | 4 (3-5) mm | |
| Rigid forceps | 22.6 ± 20.4mm2a | ||||||
| p | 0.004 | 0.001a/0.01b | 0.007 | 0.001 | 0.001 | 0.001 | |
| Artifacts (0-25%) | |||||||
| Cryoprobe | 4.5% | 100% | 97.8% | ||||
| Flexible forceps | 9% | 93.9% | |||||
| p | 0.62 | ||||||
| Artifacts (> 25%) | |||||||
| Cryoprobe | 4.5% | 0 | 2.2% | ||||
| Flexible forceps | 86.3% | 6.1% | |||||
| Depth (mesothelial connective tissue) | |||||||
| Cryoprobe | 100% | 34.8% | |||||
| Flexible forceps | 95.4% | 59.2% | |||||
| p | 0.02 | ||||||
| Depth (fat or deeper) | |||||||
| Cryoprobe | 63.6% | 49% | 65.2% | ||||
| Flexible forceps | 22.7% | 39.4% | 40.8% | ||||
| Rigid forceps | 63% | ||||||
| p | 0.001 | ||||||
| Interpretable yes/no. | |||||||
| Cryoprobe | 81%/0% | 78.3%/15.2% | |||||
| Flexible forceps | 33 (67%)/11 (22.4%) | ||||||
| p | 0.69 | ||||||
The proportion of artifacts affecting more than 25% of the CB sample ranged from 0% to 4.5%, less than that of FBF samples in the 3 studies in which it was analyzed14,20,24. Similar observations were made regarding the depth of the samples obtained with both techniques20,23,24. The depth of tissue, defined as the presence of fat or muscle tissue, a factor that is particularly relevant for determining tumor invasion, was greater in cryoprobe biopsies -- 65% of all samples versus 40% of FBF, depending on the series24.
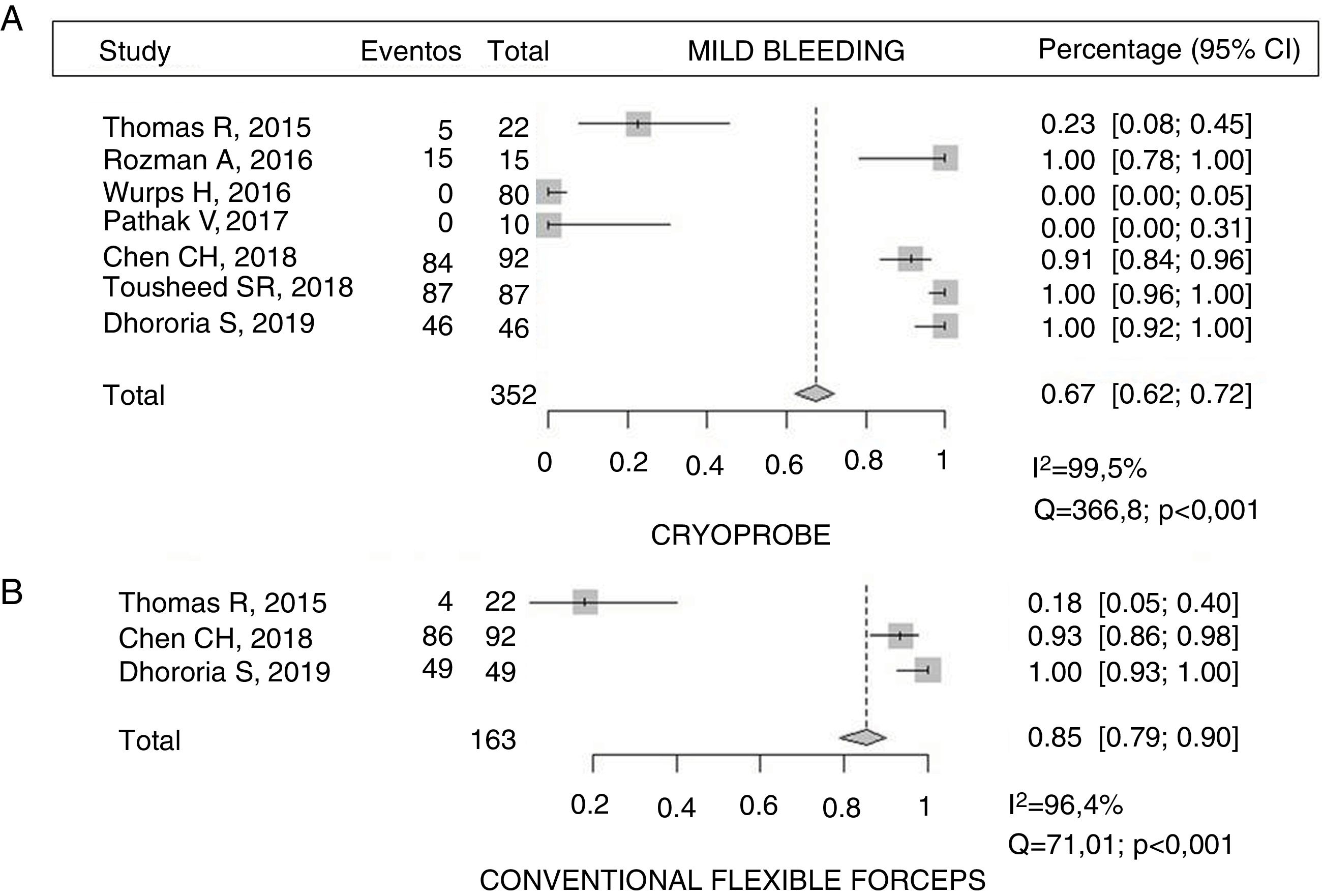
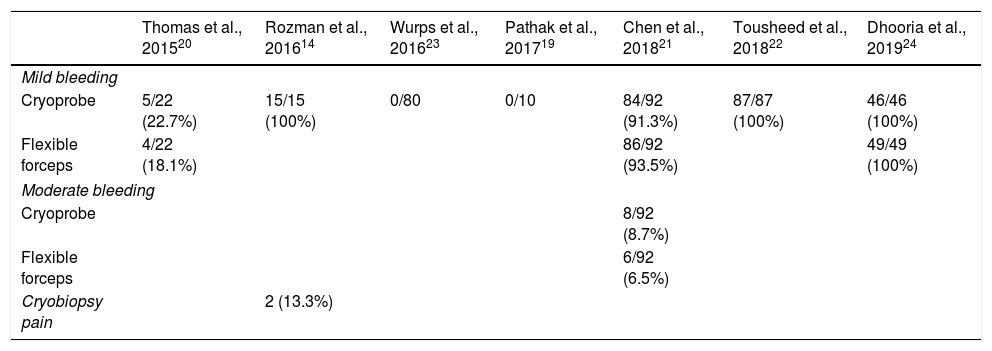
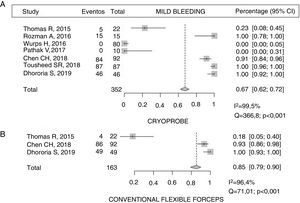
ComplicationsA total of 67% (95% CI 62-72) of patients undergoing CB had mild bleeding compared with 85% (95% CI 79-90) of those in whom the sample was obtained with FBF14,20–22,24, with statistically significant differences (p < 0.001). However, a high I2 was calculated, indicating a wide variability in the results of the studies (Fig. 3). Moderate bleeding was described in 8.7% (8/92) and 6.5% (6/92), respectively21. No cases of bleeding associated with CB were described in 2 of the studies21,23(Table 5). Only 1 study described acute pain during the CB procedure, which was reported by less than 14% of subjects14.
Complications.
| Thomas et al., 201520 | Rozman et al., 201614 | Wurps et al., 201623 | Pathak et al., 201719 | Chen et al., 201821 | Tousheed et al., 201822 | Dhooria et al., 201924 | |
|---|---|---|---|---|---|---|---|
| Mild bleeding | |||||||
| Cryoprobe | 5/22 (22.7%) | 15/15 (100%) | 0/80 | 0/10 | 84/92 (91.3%) | 87/87 (100%) | 46/46 (100%) |
| Flexible forceps | 4/22 (18.1%) | 86/92 (93.5%) | 49/49 (100%) | ||||
| Moderate bleeding | |||||||
| Cryoprobe | 8/92 (8.7%) | ||||||
| Flexible forceps | 6/92 (6.5%) | ||||||
| Cryobiopsy pain | 2 (13.3%) | ||||||
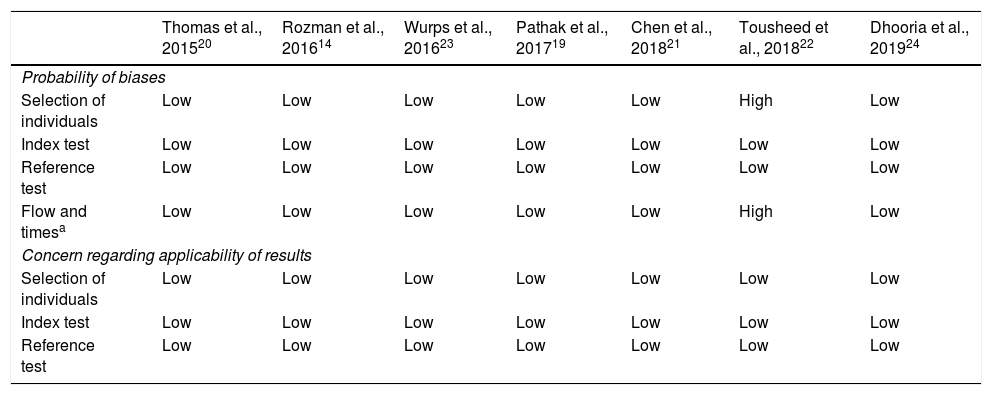
We assessed the quality of the studies included in a systematic review using the QUADAS-2 tool (Table 6). With regard to the 4 key domains for assessing the possibility of biases, the risk of bias was judged to be low in most studies. Only in 1 retrospective study, which included a historical series of MTs with FBF as a control group, was it considered high22.
Quality of studies according to the QUADAS-2 tool.
| Thomas et al., 201520 | Rozman et al., 201614 | Wurps et al., 201623 | Pathak et al., 201719 | Chen et al., 201821 | Tousheed et al., 201822 | Dhooria et al., 201924 | |
|---|---|---|---|---|---|---|---|
| Probability of biases | |||||||
| Selection of individuals | Low | Low | Low | Low | Low | High | Low |
| Index test | Low | Low | Low | Low | Low | Low | Low |
| Reference test | Low | Low | Low | Low | Low | Low | Low |
| Flow and timesa | Low | Low | Low | Low | Low | High | Low |
| Concern regarding applicability of results | |||||||
| Selection of individuals | Low | Low | Low | Low | Low | Low | Low |
| Index test | Low | Low | Low | Low | Low | Low | Low |
| Reference test | Low | Low | Low | Low | Low | Low | Low |
However, we must emphasize that no concerns regarding the applicability of the results emerged in our evaluation.
DiscussionThis systematic review and meta-analysis evaluates the efficacy and safety of pleural CB versus FBF biopsy techniques performed during MT in the study of PE. Although variability is high, the level of quality is acceptable. CB is shown to be a safe technique, with an overall yield of 95% for establishing the etiology of PE. Pleural samples obtained with cryoprobe are larger, deeper, better quality, and more interpretable, and have fewer artifacts than those obtained with FBF. However, the data are insufficient to draw firm conclusions about a potential advantage in the molecular characterization of samples obtained in lung cancer patients with PE.
In one of the studies, special difficulties were described for the performance of CB in patients with a very dense pleural surface14,24, so it is highly likely that the macroscopic appearance and consistency of metastatic implants is important in the choice of this biopsy technique compared to conventional methods.
A limitation of semi-rigid MT is the small sample size, so many experts recommend 6 to 10 biopsies1–3. As described in this pooled analysis, the samples obtained by CB from the parietal pleura are significantly larger than those obtained with FBF14,19,20,22–24. This may be of particular importance in the diagnosis of malignant PE, as a large sample is needed to perform not only morphological, immunohistochemical and molecular studies, but also to differentiate metastatic PE from different organs or hematological effusion from pleural mesothelioma. In a very recent study, not included in this review since it only included 5 cases with pleural mesothelioma, the size of the samples obtained with cryoprobe was 3 times greater than with FBF. The depth needed to establish the diagnosis of mesothelioma was achieved in 4 cases using CB compared to 1 using FBF, and the percentage of artifacts was significantly lower for CB compared to FBF (9% vs 35%, p < 0.001)18. With CB, the diagnosis of mesothelioma could be established successfully in all cases, while with FBF, diagnosis was only achieved in 1 case18. Despite these results, further studies seem necessary to determine the optimal biopsy technique for the diagnosis of pleural mesothelioma.
With the development of new targeted therapies, including immunotherapy for the treatment of non-small cell lung cancer, the demand for better quality tumor samples has increased11. In a small descriptive study conducted by our group on the diagnostic yield of semi-rigid MT for the molecular characterization of malignant PE in non-small cell lung cancer, molecular testing was performed on 14 adenocarcinomas. Sufficient useful material was obtained to determine the EGFR mutation status in 100% and ALK translocation in 90%25. Only 2 studies in this meta-analysis analyzed cryoprobe samples for the detection of EGFR gene mutation, but this was achieved in all tumor samples analyzed. Given the growing importance and development of targeted therapies, whenever new molecular alterations or conduction mutations are identified, new studies are needed to establish the indication of parietal pleural cryoprobe as a new biopsy technique for optimizing the sample and identifying the greatest number of molecular alterations possible26,27.
The methodology of this review has been rigorous, with independent double screening of abstracts, review of articles, data extraction, and evaluation of the quality of studies. The rigorous and evidence-based process used in the construction of the QUADAS-2 tool allowed us to assess and qualify the risk of bias and concerns regarding applicability. As such, the authors consider that this review provides a reliable summary of the existing bibliography. However, it has limitations. The studies included were mainly observational and there is a remarkable rate of heterogeneity in the main objectives studied.
A systematic review describing similar results has recently been published28. However, one of its limitations is that the only randomized controlled trial published so far was not included among the selected studies24.
The results of this meta-analysis show that CB of the parietal pleura during MT is a safe procedure with a high diagnostic yield for PE. Obtaining larger, better quality samples with fewer artifacts would shorten the procedure time, because fewer biopsies are needed than with FBF, and obtaining larger tissue specimens may help reduce the number of tests and avoid repeat procedures. If we take into account that tissue is now the standard material for establishing the diagnosis of non-small cell lung cancer and, given the continuous search for new molecular markers, the most significant limiting factor is the amount of tumor available, pleural CB may be considered the best option for establishing morphological, immunohistochemical, and molecular diagnosis in this group of patients, although a greater body of scientific evidence that is more homogeneous and higher quality is required.
Another limitation of the technique is that it is not standardized. Probe type and freeze time vary between hospitals, and all studies in this meta-analysis were performed in single centers. Multicenter studies with a rigorous methodology are needed to evaluate the routine use of this new technique as a tool during MT and its application in routine clinical practice.
Conflict of interestsThe authors state that they have no conflict of interests.
Please cite this article as: Rial MB, Rodríguez IL, Roibás CM, Fernández VL, Delgado MN, Barreira AS et al. Rentabilidad diagnóstica y seguridad de la criobiopsia pleural durante la toracoscopia médica en el estudio del derrame pleural. Una revisión sistemática y metaanálisis. Arch Bronconeumol. 2020. https://doi.org/10.1016/j.arbres.2019.12.001