To demonstrate the diagnostic accuracy of an integrated approach of blind trans-bronchial needle aspiration (TBNA) and 99mTc-2-methoxy-isobutyl-isonitrile single photon emission computed tomography (99mTc-MIBI-SPECT) in diagnosing mediastinal lymph adenopathy.
MethodsSixty-one consecutive patients with mediastinal lymph adenopathy undergoing both TBNA and 99mTc-MIBI-SPECT were prospectively enrolled. Mediastinoscopy was attended in case of negative TBNA.
ResultsEighty-three adenopathies were sampled (73 malignant and 10 benign). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of TBNA was 74%, 100%, 100%, and 34%, respectively; and of 99mTc-MIBI-SPECT were 96%, 80%, 97%, and 73%, respectively. Combining TBNA and 99mTc-MIBI-SPECT results sensitivity, specificity, PPV, NPV of 97%, 100%, 100%, and 83%, respectively, were obtained. TBNA alone avoided mediastinoscopy in 65% of cases, while an integrated approach could have potentially obviated mediastinoscopy in 76%.
Conclusions99mTc-MIBI-SPECT improved the sensitivity and the NPV of TBNA, reducing the need of mediastinoscopy.
Demostrar la exactitud diagnóstica de un abordaje integrado del diagnóstico de las adenopatías mediastínicas mediante aspiración por punción transbronquial (TBNA) ciega y tomografía computarizada de emisión fotónica única con 99mTc-2-metoxi-isobutil-isonitrilo (99mTc-MIBI-SPECT).
MétodosSe incluyó prospectivamente en el estudio a 61pacientes consecutivos con adenopatías mediastínicas a los que se practicó una TBNA y una 99mTc-MIBI-SPECT. En el caso de que la TBNA fuera negativa se realizaba una mediastinoscopia.
ResultadosSe obtuvieron muestras de 83adenopatías (73malignas y 10benignas). La sensibilidad, la especificidad, el valour predictivo positivo (VPP) y el valour predictivo negativo (VPN) de la TBNA fueron del 74, del 100%, del 100 y del 34%, respectivamente, y las de la 99mTc-MIBI-SPECT fueron del 96, del 80, del 97 y del 73%, respectivamente. La combinación de TBNA y 99mTc-MIBI-SPECT alcanzó una sensibilidad, especificidad, VPP y VPN del 97, del 100, del 100 y del 83%, respectivamente. La TBNA sola evitó la mediastinoscopia en el 65% de los casos, mientras que un abordaje integrado podría haber obviado la mediastinoscopia en el 76% de los casos.
ConclusionesLa 99mTc-MIBI-SPECT mejoró la sensibilidad y el VPN de la TBNA, reduciendo la necesidad de realizar mediastinoscopias.
Differential diagnosis of mediastinal lymph adenopathy ranges from various disease as infection, neoplasm, granulomatous, and reactive hyperplasia. Before the era of F-18-2-fluoro-2-deoxyglucose positron emission tomography (18FDG-PET), chest computed tomography (CT) was the conventional method used in evaluating the mediastinal lymph adenopathy. Currently, PET is routinely used as standard non-invasive tool in mediastinal staging of lung cancer with reported sensitivity of 61%–88%, and specificity of 77%–96%.1 Despite that, pathological diagnosis is still required to verify the lymph node positive on PET. Mediastinoscopy is generally considered the gold standard for sampling superior mediastinal lymph node (LN), despite the recent emergence of endobronchial ultrasound-transbronchial needle aspiration biopsy (EBUS-TBNA) as a valuable alternative.1 However, PET and EBUS are expensive and cumbersome methods, with limited availability, particularly in poor countries. 99mTc-2-methoxy-isobutyl-isonitrile (99mTc-MIBI), a myocardial perfusion imaging tracer, has been reported as an efficient tool in diagnosing indeterminate pulmonary lesion2 and anterior mediastinal mass3 using Single Photon Emission Computed Tomography (SPECT) acquisition. Conventional TBNA is a safe, efficient, and economical method for diagnosing mediastinal adenopathy, but it is underused due to unfounded fear of possible complications, inability to reproduce the high yields reported in the literature, fear of damaging the bronchoscope, and long learning curve. Probably, the only great flaw of TBNA is its “blindness“.4 The aim of this paper was to demonstrate (1) the diagnostic accuracy of traditional TBNA and 99mTc-MIBI- SPECT in diagnosing mediastinal LNs and (2) if a TBNA and 99mTc-MIBI-SPECT integrated approach improved the accuracy of TBNA alone and reduced the number of mediastinoscopies.
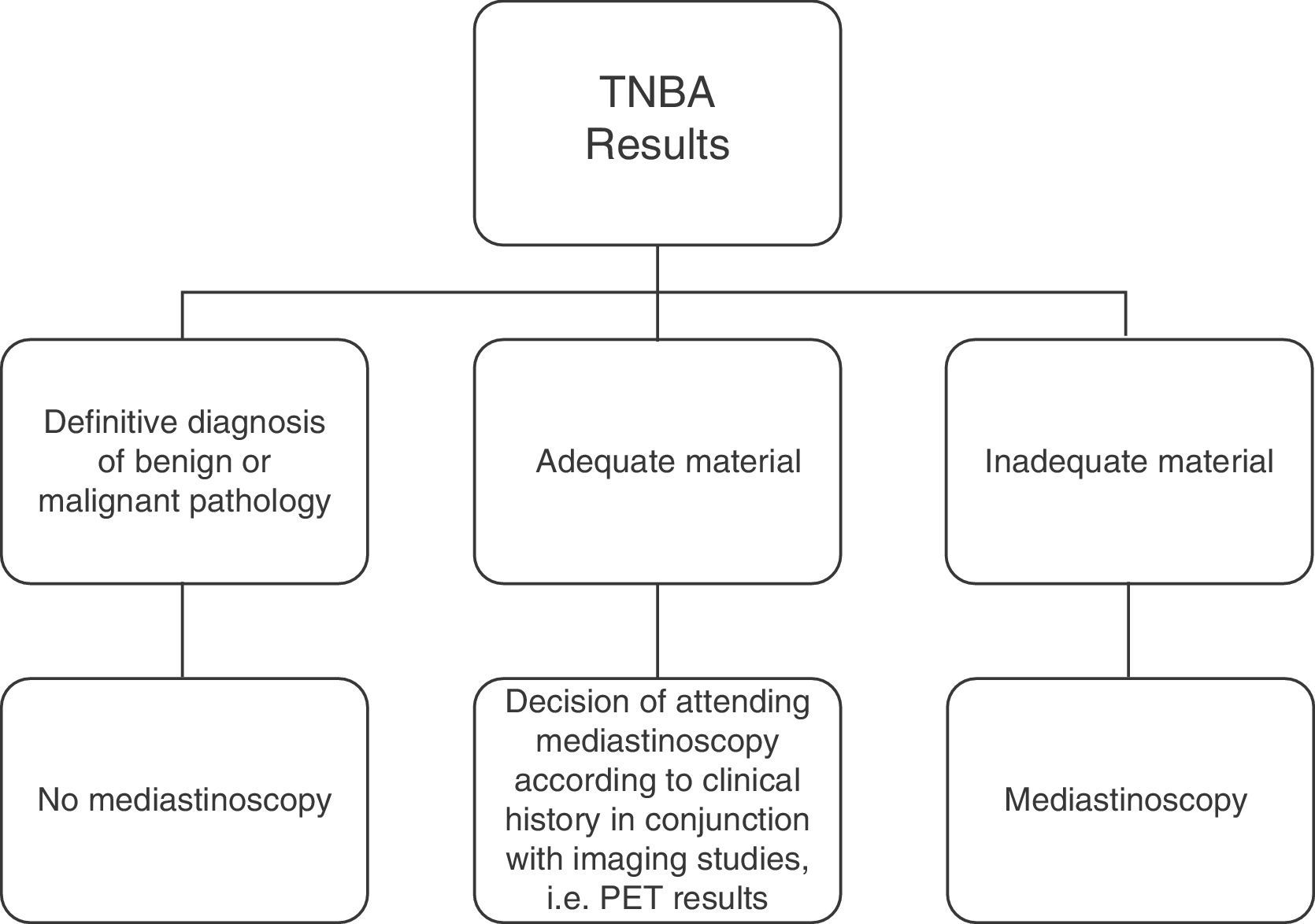
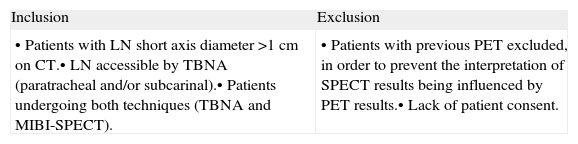
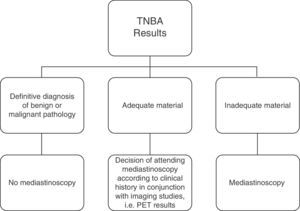
Materials and MethodsStudy DesignThis was a prospective, non-randomized, single-centre study performed in the Thoracic Surgery Unit of Second University of Naples. Selection criteria and decision making in the light of TBNA findings are reported in Table 1 and Fig. 1, respectively. The SPECT results did not alter the standard diagnostic work-up. The cytologist and nuclear medicine specialists were blind to the results of the other procedures. The TBNA and SPECT results were correlated with the final diagnosis of the adenopathies to assess the diagnostic yield. The protocol of this study was approved by our Hospital Ethics Committee.
Inclusion and Exclusion Criteria.
| Inclusion | Exclusion |
| •Patients with LN short axis diameter >1cm on CT.•LN accessible by TBNA (paratracheal and/or subcarinal).•Patients undergoing both techniques (TBNA and MIBI-SPECT). | •Patients with previous PET excluded, in order to prevent the interpretation of SPECT results being influenced by PET results.•Lack of patient consent. |
LN, lymph nodes; MIBI-SPECT, single-photon emission computed tomography with methoxyisobutylisonitrile; PET, positron emission tomography; TBNA, transbronchial needle aspiration, CT, chestcomputed tomography.
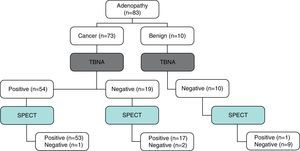
The diagram shows the diagnostic work-up. An “adequate” specimen was defined according to the presence of numerous benign lymphoid cells, indicating that the sample was obtained from a lymph node. A specimen was considered as “inadequate” when no tissue/cells were present, blood or bronchial mucosa cells only or suspicious malignant cells insufficient for a definitive diagnosis of cancer were found. TBNA=transbronchial needle aspiration; PET=positron emission tomography.
Between January 2006 and December 2011, of the 273 consecutive patients referred to our unit for diagnosis and/or treatment of mediastinal involvement, 63 met the inclusion criteria and were enrolled. All patients underwent a chest CT with contrast, and LNs with a short axis diameter >1cm were considered enlarged. 99mTc-MIBI SPECT was performed before invasive diagnostic exams in all patients. LNs were subcategorized as (i) paratracheal (stations 2R, 4R, 2L, and 4L) and (ii) subcarinal (station 7) according to Mountain-Dresler classification5 and as N2 or N3 depending on the side of the primary lesion. 18FDG-PET was performed only in selected cases to complete the diagnostic work-up, if required.
99mTc-2-methoxy-isobutyl-isonitrile Single Photon Emission Computed TomographyA commercial 99mTc-MIBI preparation (Cardiolite; Squibb International) was used. The labelling and quality control procedures were performed according to the manufacturer's instructions. SPECT data were acquired five minutes after injection of the tracer while using a large-field-of-view, double-head rectangular gamma camera (ECAM; Siemens, Erlangen-Germany) equipped with high-resolution, parallel-hole collimators; a 20% symmetric window at 140keV; a 128×128 word matrix, zoom 1.45; an elliptic orbit with step-and-shoot acquisition at 3° intervals over 360° (180° per head), and a 20s dwell time per stop. After pre-filtration with a count-optimised Metz filter, images were reconstructed with a ramp filter to produce 4-pixel-thick transaxial slices. Coronal, and sagittal, views were also obtained.
Imaging InterpretationThe results were independently assessed by two nuclear medicine specialists; disagreements were resolved by consensus with a third observer as referee.
The 99mTc-MIBI SPECT examinations were reconstructed in three orthogonal planes (transaxial, sagittal, and coronal). The analysis of 99mTc-MIBI uptake was based on the lesion count number on SPECT slices. The images were visually compared with the chest CT scan at the same time to aid in locating focal lesions which were not tracer-avid. The circular region of interest (ROI) was manually defined on the lymph node (L) in several transaxial slices and the lymph node with the highest activity was selected. The same ROI in the normal mediastinal tissue (N) was considered as background activity. Then, the uptake of the lymph node (L) was compared to the normal tissue (N) and the L/N ratio was calculated to define the metabolic activity of the lesions.
BronchoscopyTBNA was conducted by the same operator (AF) using disposable 21-gauge cytological needles and a standard flexible bronchoscope (BF-T160; Olympus; Tokyo, Japan). In the same setting of diagnostic bronchoscopy, TBNA was initially performed to avoid needle contamination. Subsequently, other procedures were performed as indicated. CT findings helped to visualize the anatomical location of LN during the procedure. Four passes per nodal station were applied. On removal of the needle, the aspirate was smeared onto microscopic slides. An on-site cytopathological examination was not performed.
Histological StudiesThe cytological samples were analyzed by routine morphological staining, and immunohistochemical staining methods were used, if indicated. According to cytological findings, TBNA specimen was defined as “adequate” or “inadequate” as reported in Fig. 1. Surgical biopsy was conducted by another operator (MS) in the week following the TBNA procedure if an inconclusive diagnosis was obtained from cytological study. The pathologist was blinded to the SPECT results.
Statistical AnalysisData are presented as mean±standard deviation (SD). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of TBNA were calculated in the standard manner. Comparison was assessed by Chi-square (qualitative data), and by Mann–Whitney U-tests (quantitative data). To evaluate correlation between lymph node size and MIBI uptake, we used the Spearman's rank correlation test. The accuracy of MIBI (variable) to distinguish malignant from benign lesions (classification variable) was calculated with receiver operating characteristics (ROC curve). The optimum cut-off point from the ROC analysis was established by selecting the value that provides the greatest sum of sensitivity and specificity. For the optimum cut-off point provided by ROC analysis, sensitivity, specificity, PPV, and NPV were calculated. To evaluate the diagnostic accuracy of combined TBNA and SPECT approach for prediction of lymph node metastasis, we considered that the result was “positive” for malignancy if one of the two procedures resulted positive; and “negative” for malignancy if both SPECT and TBNA were negative. Sensitivity, specificity, PPV, and NPV of the combined TBNA and SPECT were then calculated using the standard definitions. A value of P<.05 was considered statistically significant. MedCalc® statistical software was used for analysis.
ResultsOf the 63 patients enrolled, two were excluded (one refused bronchoscopy and in other patient the quantity of MIBI tracer was inadequate to complete the exam). Thus, our study population comprised 61 patients. There were 50 males and 10 females, with a mean age of 62±6.5 years (range 43–75 years). The total number of LNs sampled was 83, considering that in the same patient more than one LN station was biopsied if indicated. The mean size LN lesion punctured was 2.2±0.3cm. In all patients the procedure was applied under local anaesthesia, except two where intravenous sedation was required. No complication or deaths occurred. N2 patients (n=29) were referred for neoadjuvant chemotherapy. Patients with N3 disease (n=2) or stage IV (n=20) underwent chemotherapy and/or radiotherapy as indicated.
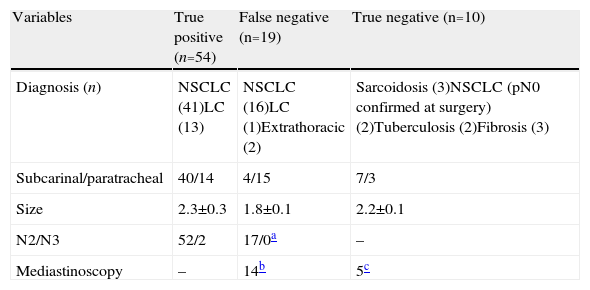
Trans-bronchial Needle Aspiration ResultsTBNA results were shown in Table 2. Sensitivity, specificity, PPV, and NPV were 74% (54/73; 95% CI: 62.8–82.6); 100% (10/10; 95% CI: 72.2–100); 100% (54/54); and 34% (10/29), respectively. Among malignant lesions, the positive aspirate was significantly higher in subcarinal than in paratracheal station (91% vs. 48%, respectively, P=.0004); and in LNs with a greater diameter (2.3±0.3 vs. 1.8±0.1, respectively, P<.0001).
Diagnosis of Lymphadenopathy (n=83) According to the TBNA Results.
| Variables | True positive (n=54) | False negative (n=19) | True negative (n=10) |
| Diagnosis (n) | NSCLC (41)LC (13) | NSCLC (16)LC (1)Extrathoracic (2) | Sarcoidosis (3)NSCLC (pN0 confirmed at surgery) (2)Tuberculosis (2)Fibrosis (3) |
| Subcarinal/paratracheal | 40/14 | 4/15 | 7/3 |
| Size | 2.3±0.3 | 1.8±0.1 | 2.2±0.1 |
| N2/N3 | 52/2 | 17/0a | – |
| Mediastinoscopy | – | 14b | 5c |
LC, lung cancer, NSCLC, non-small cell lung cancer.
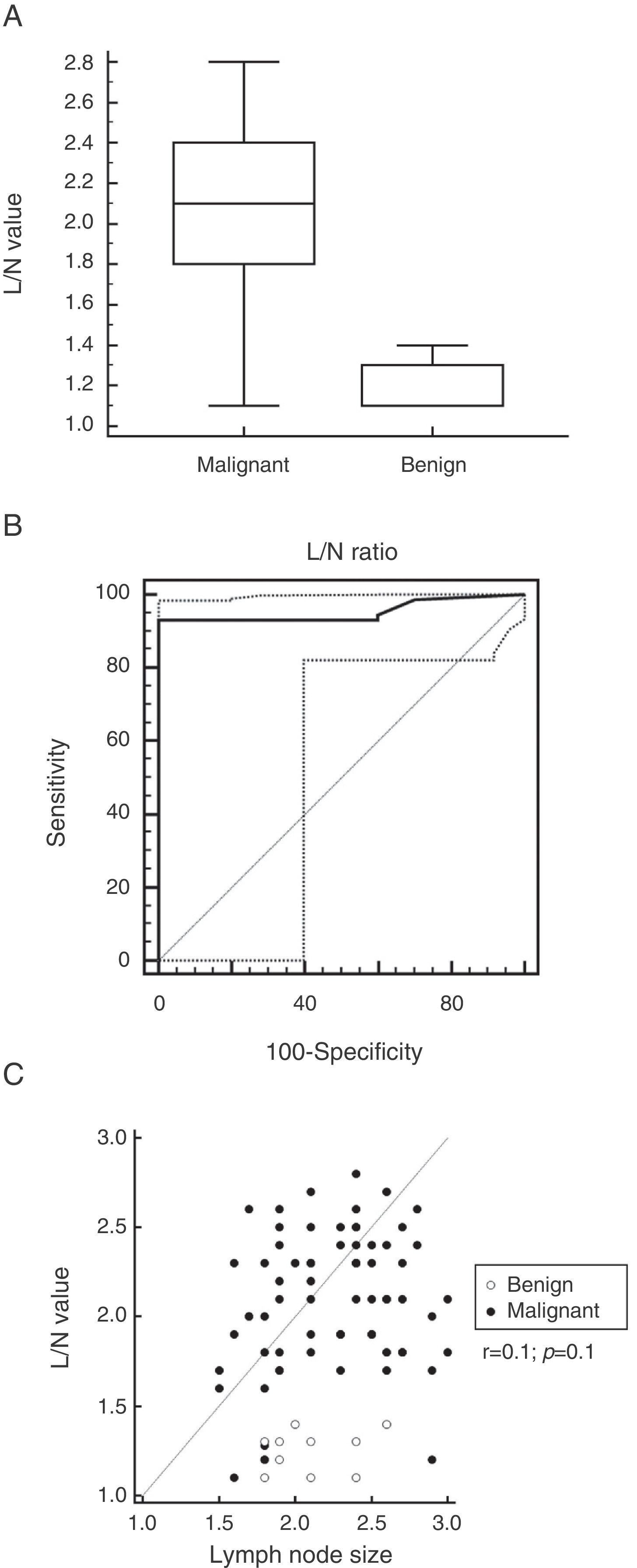
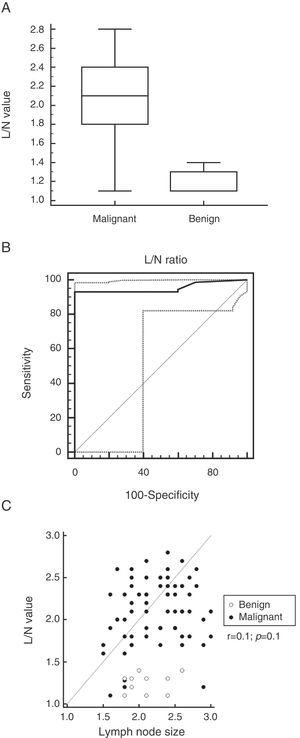
The L/N value was significantly higher in malignant than in benign LN (2.1±0.3 vs. 1.4±0.4, respectively, P=.0001; Fig. 2A). Sensitivity, specificity, PPV, and NPV were 96% (95% CI: 88.5–99.1); 80% (95% CI: 44.4–97.5); 97% (95% CI: 90.3–99.7); and 73% (95% CI: 39–94) for a cut-off value >1.4 (AUC: 0.860; 95% CI: 0.766–0.926; Fig. 2B). Three malignant lesions presented an L/N value <1.4, while only one benign adenopathy had a value >1.4. No correlation was found between size and MIBI uptake (r=0.1; 95% CI: 0.04–0.3; P=1, Fig. 2C); subcarinal compared to paratracheal LN had similar MIBI uptake (2±0.4 vs. 1.9±0.4, respectively, P=.4).
The L/N value was significantly higher in malignant than in benign lymph adenopathy (P=.0001; part A). ROC analysis showed that MIBI-SPECT had a sensitivity, specificity, PPV, and NPV for detecting malignant lymph adenopathy of 96%; 80%; 97%; and 73% for a cut-off value >1.4 (AUC: 0.860; 95% CI: 0.766–0.926; part B). No significant correlation was found between size and MIBI uptake (r=0.1; 95% CI: 0.04–0.3; P=.1, part C).
L/N: lymph node/normal tissue ratio; MIBI-SPECT, methoxy-isobutyl-isonitrile single photon emission computed tomography.
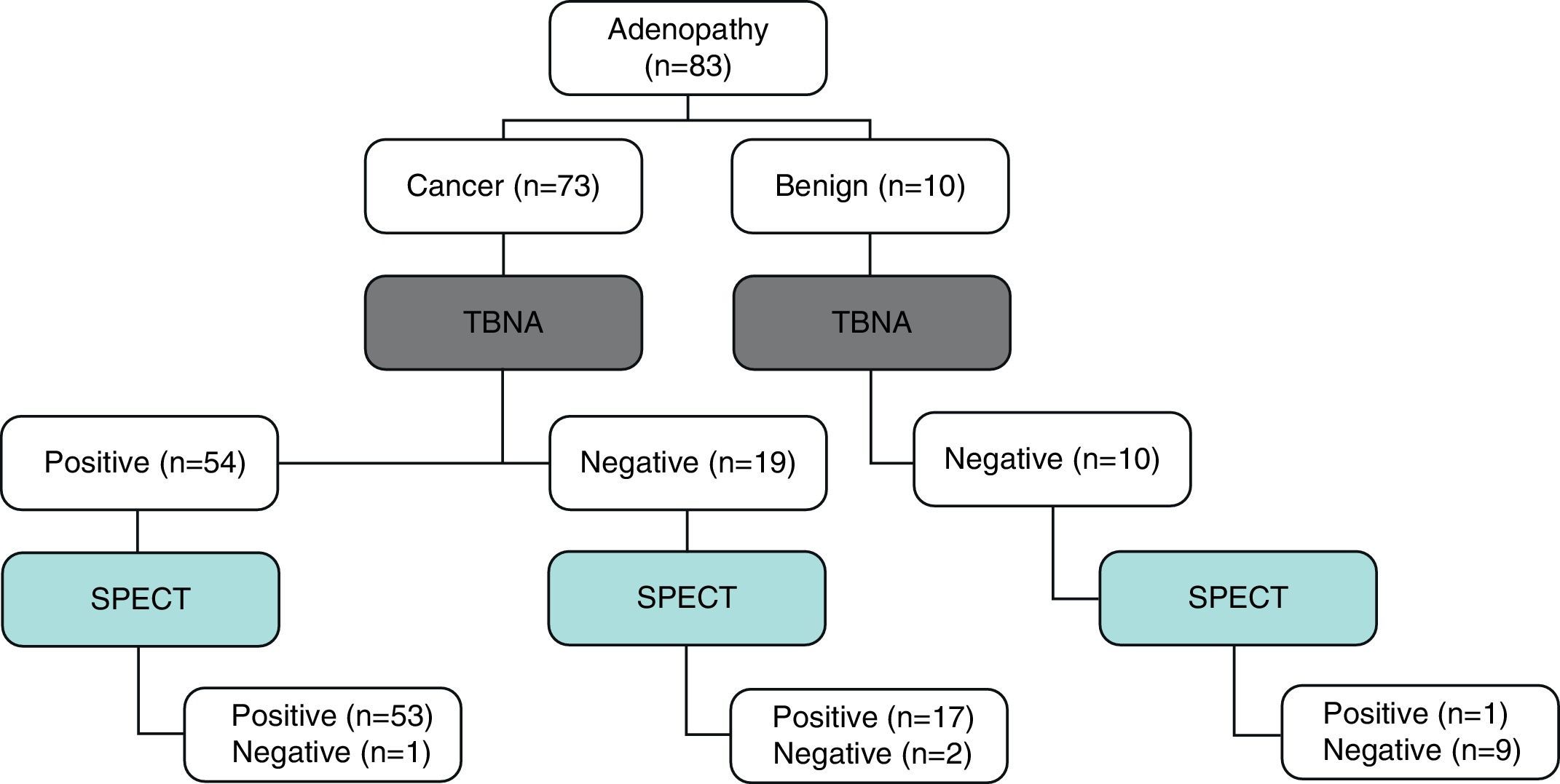
A diagram was reported in Fig. 3. Sensitivity, specificity, PPV, and NPV value of combined TBNA and SPECT approach were 97% (71/73; 95%CI: 90.5–99.2); 100% (10/10; 95%CI: 72.2–100); 100% (n=71/71); and NPV 83% (n=10/12). Clinical examples were reported in Figs. 4 and 5.
Summary of 83 lymph nodes evaluated with TBNA and MIBI-SPECT. Of 73 malignant lesions, 54 had positive TBNA for malignancy, and 70 were SPECT positive (L/N>1.4). Of three lesions with SPECT negative findings, only one had positive TBNA; while the other two malignant lesions were both TBNA and SPECT negative. Of 10 benign lesions, 9/10 cases had negative TBNA and negative SPECT (L/N value<1.4) results. Only one lesion with diagnosis of benignity on TBNA was SPECT positive. TBNA, trans-bronchial needle aspiration; MIBI-SPECT, methoxy-isobutyl-isonitrile single photon emission computed tomography; L/N: lymph node/normal tissue ratio
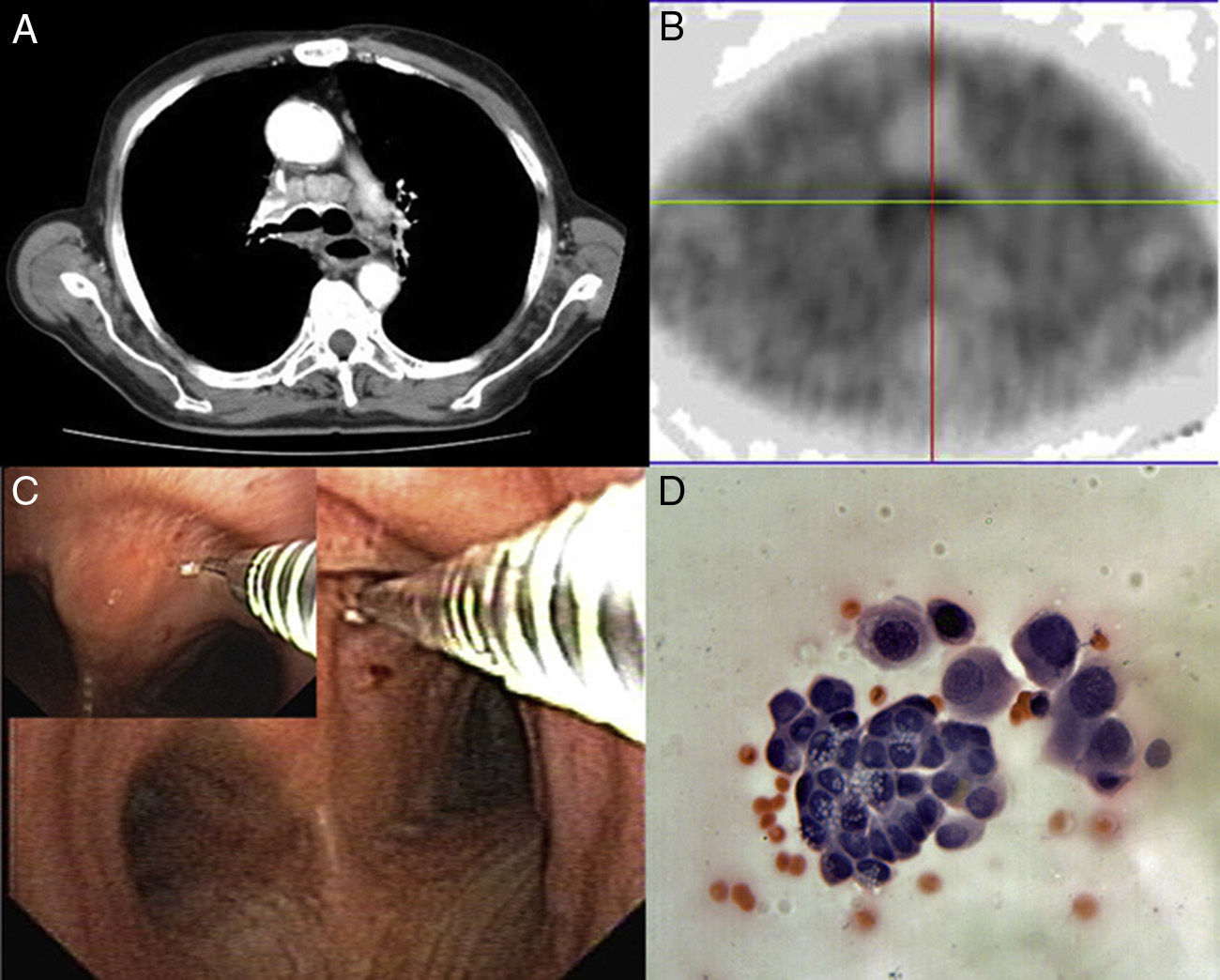
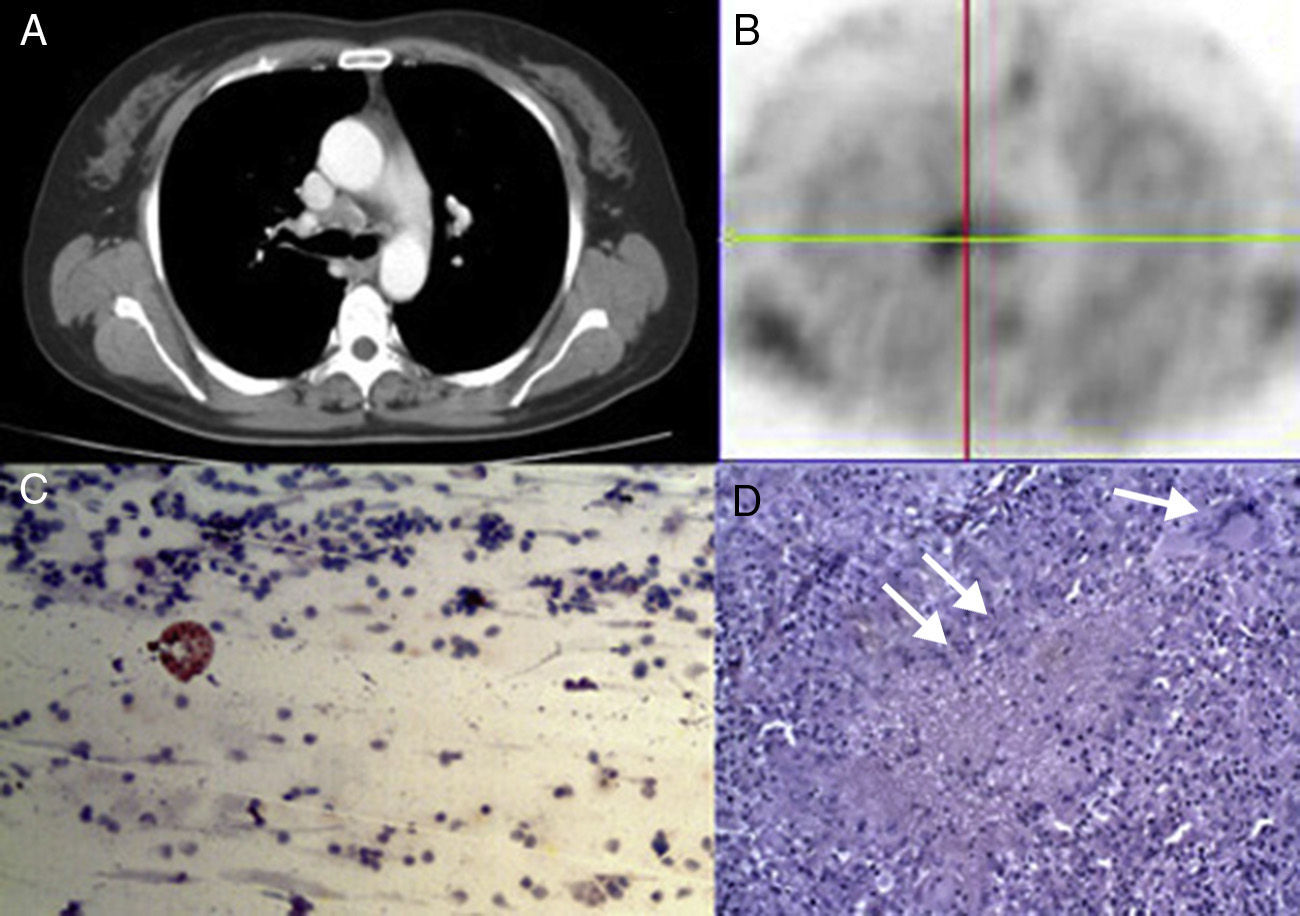
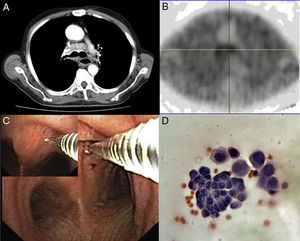
A 67-year-old man presented a mass within lower left lobe with mediastinal involvement on CT scan (part A). MIBI-SPECT showed an increased MIBI uptake to the anterior carina lymph node (part B). We performed a TBNA (part C) shown to be an adenocarcinoma (part D; haematoxylin and eosin; 200× magnification). TBNA, trans-bronchial needle aspiration; MIBI-SPECT, methoxy-isobutyl-isonitrile single photon emission computed tomography.
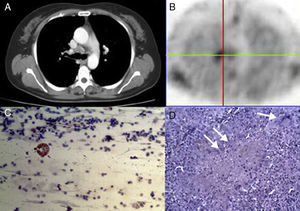
A 57-year-old woman presented with mediastinal involvement of anterior carina on CT scan (part A). The adenopathy was MIBI-avid (part B). TBNA findings showed normal lymphoid tissue suggestive of benign disease (part C; haematoxylin and eosin; 200× magnification). Specimen obtained by mediastinoscopy diagnosed to be a tuberculosis. Langhan's giant cells (white arrow) and inflammatory granulation tissue (double white arrow) were clearly evident (part D; haematoxylin and eosin; 50× magnification). CT, chest tomography; MIBI-SPECT, methoxy-isobutyl-isonitrile; TBNA, transbronchial needle aspiration.
Applying the approach of combining TBNA and SPECT, mediastinoscopy may be avoided in 63/83 (76%) cases; of these, 54 had positive TBNA for malignancy (as all would have required mediastinoscopy in the absence of TBNA), and 9 had both negative TBNA and SPECT results.
DiscussionConventional TBNA is a safe and cost-effective procedure for sampling mediastinal lymph nodes adjacent to the tracheobronchial wall. It may be performed during a routine diagnostic bronchoscopy avoiding more invasive procedure in case of positive results. Notwithstanding, TBNA is underused by the pulmonologist and thoracic surgeon. In theory, its main limit is the impossibility to see the sampled lymph node in real time. A negative TBNA result does not definitely rule out malignant disease and further invasive procedures should be performed.
MIBI is a radio-pharmaceutical originally developed for myocardial perfusion studies as an alternative to 201Tl. The mechanism of MIBI uptake in malignant tumours is not completely understood. It may be favoured by (i) stronger negative mitochondrial and plasma membrane potentials or (ii) increase of blood flow and capillary permeability of tumour cells due to their increased metabolism. Several reports described the role of 99mTc-MIBI in diagnosing lung cancer, but only three papers investigated its role in mediastinal staging. Chiti et al.6 and Komori et al.7 reported an accuracy value of 86% and 95.2%, respectively, of SPECT for detecting mediastinal involvement; Nosotti et al.8 showed that SPECT had a sensitivity, specificity, PPV and NPV value of 54.5%; 100%; 100%, and 86.6% in diagnosing metastatic adenopathy. To our knowledge, no paper has investigated if 99mTc-MIBI-SPECT can enhance the sensitivity and the NPV of the TBNA alone, and if an integrated approach of both methods can reduce the number of mediastinoscopy.
Firstly, the sensitivity value (74%) seen in the present study was similar to that reported in several studies,9–11 in contrast with other papers12,13 that reported a lower level of sensitivity. It is well known that the sensitivity of TBNA improved substantially in patients in whom malignancy was suspected14; therefore, the high sensitivity observed in our population may be due to the higher incidence of malignant (88%) than benign lesions evaluated. Conversely, we registered a low value of NPV (34%). Thus, in case of negative TBNA, mediastinoscopy should be performed (especially if LNs are PET positive) because only in 34% of cases might it be a true negative result. There were 19 false negative TBNA results, despite the fact that in 4/19 (21%) cases the material sampled was adequate (presence of lymphocytes indicating that the sample was obtained from LN) but negative for malignancy. The LNs sampled probably had a small number of malignant cells making it difficult to provide a cytological diagnosis of malignancy. Among benign lesions, in 8/10 cases the TBNA correctly identified the lesion as benign (adequate material with the presence of benign lymphocytes and inflammatory cells) but it did not allow a specific diagnosis. In theory, the diagnosis of sarcoidosis (n=2) and tuberculosis (n=3) was difficult because we used a 21-gauge needle, and better results have been reported with larger calibre needles.15 Because the positive TBNA results were not confirmed by other invasive procedures, the value of specificity and PPV of TBNA in the present paper were 100%.
The diagnostic yield of TBNA was related to size and lymph node station. Among malignant lesions, a greater short-axis nodal diameter increased the risk of positive results because small adenopathies are more difficult to biopsy using a blind procedure, such as conventional TBNA without EBUS. However, the rate of positive aspirates was significantly higher in subcarinal than in paratracheal stations, in line with the data of Medford et al.9 The proximity of major vessels to the left paratracheal area and the more acute angulation of the TBNA needle may also have contributed to the inferior performance of paratracheal TBNA, although this is not supported by other studies.
Secondly, MIBI uptake correlated significantly with the nature of the lesion (benign vs malignant), while the size and the LN stations did not affect SPECT results. Three malignant LNs were SPECT negative. Of these, two were necrotic lesions; thus, the poor vascularization and the low mitochondrial content may explain the low MIBI uptake considering that 99mTc-MIBI is used as a sensitive indicator of myocardial cell viability because it does not accumulate in the ischaemic myocardial tissue. In the other case, a biological tumour factor, such as altered PGP expression, may explain the negative SPECT findings because PGP mediates MIBI uptake in neoplastic cells.4 Conversely, only one benign adenopathy, an active tuberculosis, was SPECT positive (Fig. 5). Active tuberculosis is well known to give a false positive on 99mTc-MIBI uptake, as reported by Onsel et al.16
Thirdly, the combination of both techniques improved the sensitivity and the NPV value of TBNA alone (97% vs 74%, respectively, and 83% vs. 34%, respectively), and its application in clinical practice may potentially reduce the number of mediastinoscopy. In our series, TBNA alone permitted a diagnosis of malignancy in 54/83 (65%) patients who were excluded from mediastinoscopy. Conversely, mediastinoscopy could have been potentially obviated in two-third (63/83) of the cases using a combined approach; of these, 54 had positive TBNA for malignancy, and 9 were negative on TBNA (normal lymphoid tissue in sample) and SPECT findings. These results were similar to those of Nosotti et al.17 with EBUS-TBNA that requires more sophisticated, expensive equipment and specific training compared to conventional TBNA. The advantages of TBNA compared to mediastinoscopy are the low cost, the low invasiveness, and the better utilization of clinical resources that is of paramount importance particularly in this time of economic recession and limitations on funding. In addition, IIIA N2 patients with mediastinal downstaging after neoadjuvant chemotherapy may require a repeat mediastinoscopy that could be avoided if TBNA is applied as first choice for mediastinal staging.
Thus, a NSCLC patient with mediastinal adenopathy that is TBNA (normal lymphoid tissue in tissue sample) and SPECT (low MIBI uptake) negative might be referred directly to surgery. A patient with lung cancer and N2 involvement who has an enlarged N3 station that is both TBNA and SPECT negative might be referred directly to neo-adjuvant chemotherapy and followed by surgery in case of N2 down-staging. A patient with previous history of cancer and a mediastinal adenopathy which is both TBNA and SPECT negative should undergo careful and frequent clinical follow-ups. The decision to proceed to a surgical biopsy may be guided by (i) an increased lymph node size on CT imaging or (ii) positive results on SPECT findings. Conversely, every patient with positive SPECT and negative TBNA results needs tissue confirmation via mediastinoscopy or other invasive strategies.
This study has some limitations, as follows:
- 1)
Our study population presented a higher incidence of malignant than benign lesions (88% versus 12%, respectively). All patients of our study group were referred from a chest surgery unit with a probably higher cancer rate than would be expected from referral from a pulmonary medicine clinic. In addition, the mean size of lymph adenopathy evaluated was 2.2cm with a high risk of being malignant. Thus, the selection of our study population may affect the results and the diagnostic yield of both techniques should be tested in evaluating sub centimetres adenopathy.
- 2)
The assumption that all of the positive TBNA are true positive, leading us to accept some approximations in the calculation of the statistical variables such as sensitivity and specificity.
- 3)
The main drawback of SPECT is the poor quality of anatomical resolution. In certain cases, it is difficult to identify the exact LN stations if the SPECT findings are not visually correlated with CT scan findings. An integrated SPECT-CT unit was not available in this trial. It is certainly possible that such a method may improve the identification of individual LN.
- 4)
The absence of pathologist during bronchoscopy and the use of 21-gauge needle may reduce the diagnostic accuracy of TBNA especially in benign lesions.
- 5)
The small sample size does not permit definitive conclusions. We enrolled only 61 patients in the last six years (10/year) and several reasons may explain the small sample size. In our hospital, SPECT equipment was routinely used for myocardial scintigraphic examinations and its use for evaluating mediastinal lymph adenopathy was limited to a few days a week. Before admission, most patients underwent PET, so they were excluded. Finally, other patients presented lymph adenopathy in multiple stations also not accessible by TBNA (station 5 and 6), so samples were obtained by videothoracoscopy.
In conclusion, our study confirms that traditional TBNA is a reasonable initial step in the diagnosis of mediastinal adenopathy. TBNA positive results avoid more aggressive procedures as mediastinoscopy. The combined TBNA and SPECT approach improves the NPV of TBNA alone, and significantly reduces the need for mediastinoscopy in patients with both negative TBNA and SPECT results. Conversely, tissue confirmation is mandatory in case of negative TBNA but positive SPECT. If our results are corroborated by larger studies, TBNA and SPECT may be routinely used in diagnosing of mediastinal adenopathy particularly in poor countries where more expensive and sophisticated methods such as PET and EBUS are available at very few centres only.
Conflict of InterestNone.
The authors thank Prof. Giuseppe Signoriello for the statistical review of the manuscript.
Please cite this article as: Fiorelli A, Rambaldi P, Vicidomini G, di Serio U, Accardo M, Rotondo A, et al. Uso combinado de aspiración por punción transbronquial y tomografía computarizada de emisión fotónica única con 99mTc-2-metoxi-isobutil-isonitrilo para el diagnóstico de ganglios linfáticos mediastínicos agrandados. Arch Bronconeumol. 2014;50:3–9.