The clinical and epidemiological implications of abnormal immune responses in COVID-19 for latent tuberculosis infection (LTBI) screening are unclear.
MethodsWe reviewed QuantiFERON TB Gold Plus (QFT-Plus) results (36,709 patients) from July 2016 until October 2021 in Asturias (Spain). We also studied a cohort of ninety hospitalized patients with suspected/confirmed COVID-19 pneumonia and a group of elderly hospitalized patients with COVID-19 who underwent serial QFT-Plus and immune profiling testing.
ResultsThe indeterminate QFT-Plus results rate went from 1.4% (July 2016 to November 2019) to 4.2% during the COVID-19 pandemic. The evolution of the number of cases with low/very low interferon-gamma (IFN-gamma) response in the mitogen tube paralleled the disease activity and number of deaths during the pandemic waves in our region (from March 2020 to October 2021). The percentages of positive QFT-plus patients did not significantly change before and during the pandemic (13.9% vs. 12.2%). Forty-nine patients from the suspected/confirmed COVID-19 pneumonia cohort (54.4%) had low/very low IFN-gamma response to mitogen, 22 of them (24.4%) had severe and critical pneumonia. None received immunosuppressants prior to testing. Abnormal radiological findings (P=0.01) but not COVID-19 severity was associated with low mitogen response. Immune profiling showed a reduction of CD8+T cells and a direct correlation between the number of EMRA CD8+T-cells and IFN-gamma response to mitogen (P=0.03).
ConclusionLow IFN-gamma responses in mitogen tube of QFT-Plus often occur in COVID-19 pneumonia, which is associated with a low number of an effector CD8+T-cell subset and does not seem to affect LTBI screening; however, this abnormality seems to parallel the dynamics of COVID-19 at the population level and its mortality.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (COVID-19) has become a worldwide public health emergency since its appearance in December 2019 1. Optimal treatment for COVID-19 remains challenging but some progress has been made 2. In severe COVID-19, the use of corticosteroids has been associated with improvement in treatment outcomes. Other immunosuppressive and biological agents have been used empirically or in clinical trials for severe and critical COVID-19. The risk of opportunistic infections and reactivation of tuberculosis (TB) in patients undergoing these treatments remains unclear but some TB cases have been reported 3–5. The use of Interferon gamma release assays (IGRAs) has become a routine practice for screening and diagnosis of latent tuberculosis infection (LTBI) in high-income and low-TB incidence settings 6.
IGRAs measure the release of interferon gamma (IFN-γ) in response to stimulation with specific M. tuberculosis (Mtb) antigens (i.e. ESAT-6 and CFP- 10) in peripheral blood samples. QuantiFERON TB Gold Plus™ (QFT-Plus) is the latest version of ELISA-based IGRA platform that contains two Mtb-antigen tubes that combined elicits both CD4 and CD8 antigen-specific T cell responses. This ex vivo diagnostic platform includes a negative control tube and a positive control tube (mitogen), the latter of which allows measuring IFN-γ release in blood in response to a non-specific lymphocyte activator (i.e. phytohemagglutinin [PHA], a lectin, a type of glycoprotein).
The QFT-Plus assay is currently the most commonly utilized IGRA test in Asturias, Spain. Since December of 2019, and especially in the winter and early spring of 2020, we have observed an unusual increase in the number of QFT-Plus test results with low IFN-γ responses in the mitogen control tube and indeterminate QFT-Plus test results. This period coincides with the time of the COVID-19 pandemic in our region in Spain (Asturias). In this context, we hypothesized that this unprecedented increase in the number of low IFN-γ responses to PHA was related to an unidentified biological effect of COVID-19 or its treatment. To investigate further, we measured the frequency of this unusual IGRA testing result and studied the potential factors associated with low IFN- γ responses to PHA. Specifically, we prospectively reviewed charts and measured sequential PHA responses in blood T cell subsets in a cohort of hospitalized patients with suspected or confirmed COVID-19 pneumonia during the peak of the COVID-19 pandemic.
MethodsStudy subjects and settingWe conducted an observational study at the Hospital Universitario Central de Asturias (Oviedo, Spain) in the Principado de Asturias, a region of northern Spain with a population of one million inhabitants, and with a TB incidence rate of 10 cases per 100,000 population. A research ethics committee of the Principado de Asturias approved this study, and all hospitalized patients in the prospective part of the study signed an informed written consent. In this region, all IGRA tests are centrally processed at the referral Mycobacteria laboratory of the Hospital Universitario Central de Asturias, which serves all 8 public hospitals in the region. We reviewed all testing results and ordering indications of all QFT-Plus (from 36,709 patients) conducted in our referral laboratory from July 2016 until October 2021. We also reviewed all charts of patients hospitalized in our referral center with clinical or radiological evidence of pneumonia, and/or acute respiratory distress for two weeks in March 2020, which coincided with the time of the first COVID-19 epidemic wave in the Asturias region.
SARS-CoV-2 diagnostic testingFor molecular COVID-19 diagnosis, we used a real-time reverse transcriptase-polymerase chain reaction (RT-PCR) directed to two targets located in the ORF1ab and N regions of the SARS-CoV-2. Samples from the upper (nasopharyngeal swab) and/or lower (sputum or tracheobronchial aspirate) respiratory tract were analyzed. The human beta-globin gene was utilized as the internal control for this RT-PCR assay.
For serologic diagnosis, a chemiluminescent immunoassay (CLIA) for the qualitative detection of IgM and IgG antibodies to SARS-CoV-2 was used (DiaSorin, LIAISON® SARS-CoV-2 IgM and LIAISON® SARS-CoV-2 S1/S2 IgG).
COVID-19 disease severity definitionFor the hospitalized patient cohort, COVID-19 disease severity was classified as either non-severe (mild to moderate) and severe (including critical) based on a modified version of the WHO interim guidance 7. Mild disease was defined as an uncomplicated upper respiratory tract infection (URI) with potential non-specific symptoms (e.g. fatigue, fever, cough and others) that does not require hospitalization. Moderate disease was defined as the presence of lower respiratory tract disease or pneumonia without respiratory distress and/or the need for supplemental oxygen, without signs of severe pneumonia. Severe disease was defined as severe lower respiratory tract infection or pneumonia with fever plus any one of the following: tachypnea (respiratory rate >30 breaths per minute), respiratory distress, or oxygen saturation less than 93% on room air, or PaO2/FiO2 ratio<300. Critical disease is defined as the need for intensive care unit admission or the presence of acute respiratory distress syndrome (ARDS), sepsis, or septic shock 7.
IGRA testingIn our region, the two main indications for requesting IGRA testing are TB contact-tracing and diagnosis of LTBI in immunosuppressed patients and/or candidates for biological therapies 8,9.
QFT-Plus was performed as recommended by the manufacturer (Qiagen GmbH, Hilden, Germany). A cut-off level of IFN-γ ≥ 0.35 IU/ml in TB1 (includes peptides ESAT-6 and CFP10 modified to stimulate CD4+T cells) and/or TB2 (includes peptides ESAT-6 and CFP10 modified to stimulate both CD4+and CD8+T cells) tubes and ≥ 25% than nil tube (negative control) is interpreted as a positive QuantiFERON (QFT) test result. We defined a low IFN-γ response to PHA in the QFT tests by an IFN-γ concentration ≥ 0.50 IU/mL (minimum level required by the manufacturer for a valid IGRA result) in the mitogen tube (positive control, includes PHA to stimulate T cells) and less than 50% below the average values of the majority of samples processed in the same batch. A very low IFN-γ response to PHA was defined by IFN-γ concentration <0.50 IU/mL in the mitogen tube.
Immune phenotypingPeripheral blood cells were surface-stained with anti-CD45-FITC/CD16+56-RD1/CD19-ECD/CD3-PC5 (Beckman Coulter, Brea, CA, USA) to define lymphocyte subsets, and anti-CD45RA-FITC, anti-CD8-PE, anti-CCR7-APC (Biolegend, San Diego, CA, USA) anti-CD3-ECD (Beckman Coulter), anti-CD4-PerCP (BD Bioscience, San Jose, CA, USA) to define differentiation degree of T lymphocytes. One hundred microliters of peripheral whole blood from volunteers were stained with different combinations of labeled monoclonal antibodies for 20min at room temperature. Samples were red-blood lysed with FACS Lysing Solution (BD Biosciences), washed in PBS, and analyzed using Kaluza software in a Navios cytometer (Beckman-Coulter, Brea, CA, USA). Appropriate isotype control antibodies were used for marker settings.
Statistical analysisCorrelations between variables were assessed using the nonparametric Spearman test. Analyses were performed using the PASW Statistics 17.0 statistical software package (IBM SPSS, NY, USA), and P-values of 0·05 or less were considered significant.
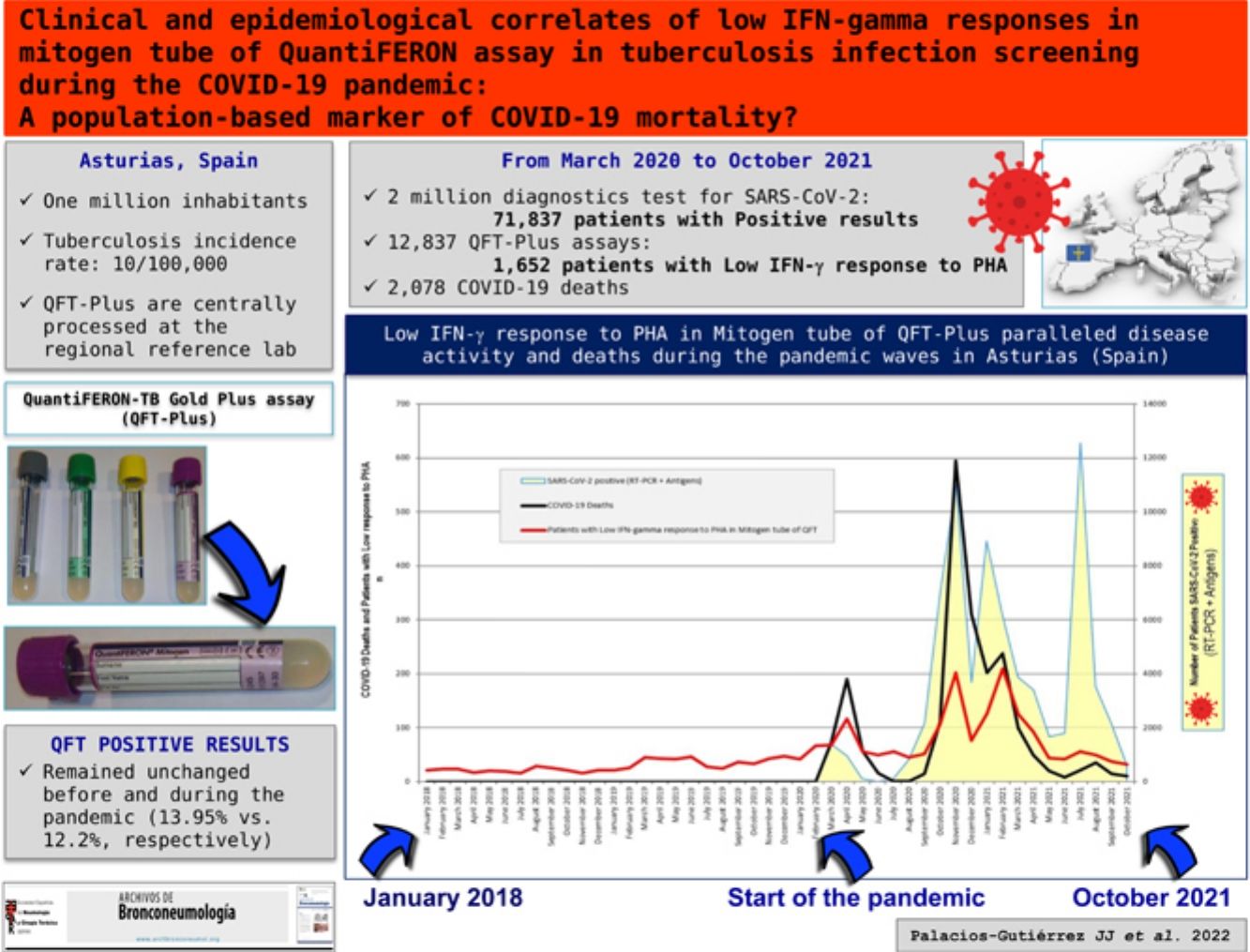
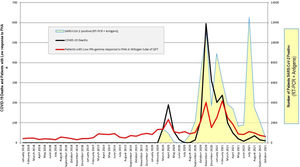
ResultsQFT-Plus results over time during the COVID-19 pandemicSince December 2019, we noted a significant increase in the number of samples with low IFN-γ responses to PHA in the mitogen tube (positive control) of the QFT-Plus assay with peaks overlapped with the COVID-19 epidemics waves registered in our region from March 2020 to October2021. This affected both the rate of very low (<0.50 IU/mL) and low (>0.50 IU/mL and less than 50% below the average values) IFN-γ response to PHA which respectively had never exceeded from 3% and 5% in the past (Figure 1A). The rate of indeterminate QFT-Plus results went from our historical average of 1.4% (from July 1, 2016, to November 30, 2019 [out of a total of 23,134 patients]) to 4.2% (from December 1, 2019, to October 31, 2021 [out of a total of 13,375 patients]). Specifically, 505 samples yielded indeterminate QFT-Plus results in that time period. There were no technical problems identified 10 or changes in testing practices that could explain these unexpected results. Of note, the number of QFT-Plus tests performed (Figure 1B) and patients with positive QFT-Plus results remained virtually unchanged before (March to November 2019) and during the pandemic (March 2020 to October 2021) (13.95% vs. 12.2%, respectively) (Figure 1A). The corresponding graphics to COVID-19 deaths evolution and from the number of patients with low IFN-gamma response to PHA in mitogen tube of QFT overlapped in time (Figure 2).
Low IFN-γ Response to Phytohemagglutinin (PHA) in QuantiFERON TB Gold Plus (QFT) Assays and COVID-19 Pandemic Evolution in the Principado de Asturias (Spain) from Spring of 2020 to Autumn of 2021 (Source: ASTURSALUD (www.astursalud.es), Principado de Asturias). A) Figure shows IFN-γ response to PHA measured in the mitogen tube of QFT assay in patients from January 2018 to October 2021 (27,480 patient-samples). Blue line: Patients with very low IFN-γ response to PHA (IFN-γ concentration (minus nil) in mitogen tube <0.5 IU/mL; QFT indeterminate result). Red line: Patients with low IFN-γ response to PHA (IFN-γ concentration (minus nil) ≥ 0.5 IU/mL in mitogen tube and less than 50% below the average values). Red and blue arrows indicate the historically maximal rate (%) of low and very low response to PHA (%) in relationship with the onset of the COVID-19 pandemic. Green line indicates % of patients with QFT-positive results. B) Figure shows distribution of the 27,480 QuantiFERON assays performed per month from January 2018 to October 2021 (monthly average=604.2; range: 398-842).
We studied a cohort of 90 sequentially hospitalized patients for two weeks in March 2020 (first epidemic wave) with suspected COVID-19 (33 patients had clinical and/or radiological evidence of pneumonia, or acute respiratory distress but with negative RT-PCR for SARS-CoV-2 results) or confirmed COVID-19 (57 patients with positive RT-PCR for SARS-CoV-2 results). There were 48 adult men and 42 women, and the average age was 63.9 years old (range 28-89). According to the WHO case definition, 68 patients (75.5%) presented mild/moderate disease (37 were RT-PCR-positive for SARS-CoV-2) and 22 (24.4%) severe/critical disease (20 were RT-PCR-positive test, P<0.05). Underlying comorbidities included hypertension (23%), diabetes mellitus (11%), chronic obstructive pulmonary disease (9%), ischemic heart disease (7%), and asthma (6%). We compared the clinical and laboratory characteristics of two groups of patients in accordance with RT-PCR SARS-CoV-2 results (Table 1). Statistical significant differences were observed in the number of days since symptoms onset, lymphocyte count, alanine aminotransferase, lactate dehydrogenase, and mitogen tube response (P <0.05).
Prospective Cohort, Patients Characteristics (N=90).
| Suspected COVID-19 pneumonia with negative or indeterminate COVID-19 testingaNo. (%) | Laboratory-confirmed COVID-19 pneumoniaNo. (%) | P valuea,b | |
|---|---|---|---|
| Demographic information | |||
| Total No. | 33 | 57 | |
| Age, Mean [SD] | 59.5 [17.7] | 66.5 [11.7] | 0.05 |
| Sex | |||
| Male | 16 (48.5) | 32 (56.1) | 0.51 |
| Female | 17 (51.5) | 25 (43.9) | |
| Symptoms | |||
| Days since symptoms onset, Mean [SD] | 5.81 [3.74] | 7.17 [2.59] | 0.04 |
| Upper airways symptoms | 23 (69.7) | 49 (86.0) | 0.12 |
| Fever | 20 (60.6) | 45 (78.9) | 0.20 |
| Dyspnea | 19 (57.6) | 37 (64.9) | 0.81 |
| Syncope | 3 (9.1) | 2 (3.5) | 0.34 |
| Comorbidities | |||
| Hypertension | 10 (30.3) | 20 (35.1) | 0.81 |
| Diabetes Mellitus | 10 (30.3) | 8 (14.0) | 0.06 |
| Radiological findings | |||
| Normalc | 6 (18.2) | 6 (10.5) | |
| Unilateral infiltrate | 9 (27.3) | 36 (63.2) | <0.01 |
| Bilateral infiltrate | 18 (54.5) | 15 (26.3) | |
| Laboratory findings | |||
| Leucocyte counts | |||
| Mean [SD] | 9440 [6450] | 6330 [2690] | 0.05 |
| Missing | 4 (12.1) | 2 (3.5) | |
| Lymphocyte count | |||
| Mean [SD] | 2150 [2920] | 1000 [652] | 0.04 |
| Missing | 9 (27.3) | 7 (12.3) | |
| Aspartate aminotransferase, U/L (4·0 – 41·0) | |||
| Mean [SD] | 98.7 [179] | 49.5 [33.4] | 0.94 |
| Missing | 24 (72.7) | 35 (61.4) | |
| Alanine aminotransferase, U/L (4·0 – 41·0) | |||
| Mean [SD] | 61.6 [113] | 56.5 [40.7] | 0.04 |
| Missing | 9 (24.3) | 9 (15.8) | |
| Lactate dehydrogenase, U/L (40·0 – 480·0) | |||
| Mean [SD] | 438 [202] | 538 [232] | 0.03 |
| Missing | 8 (24.2) | 6 (10.5) | |
| C-reactive protein, mg/L (0·0 – 5·0) | |||
| Mean [SD] | 74.0 [59.1] | 83.0 [73.5] | 0.87 |
| Missing | 1 (3.0) | 5 (8.8) | |
| Procalcitonin, ng/mL (0·0 – 0·50) | |||
| Mean [SD] | 0.727 [1.30] | 0.244 [0.426] | 0.31 |
| Missing | 22 (66.7) | 36 (63.2) | |
| Fibrinogen, mg/dL (150·0 – 600·0) | |||
| Mean [SD] | 692 [59.2] | 649 [136] | 0.29 |
| Missing | 25 (75.8) | 32 (56.1) | |
| D-dimer, ng/mL (208·0 – 500·0) | |||
| Mean [SD] | 1220 [1480] | 989 [901] | 0.94 |
| Missing | 10 (30.3) | 10 (17.5) | |
| Ferritin, ng/mL (30·0 – 400·0) | |||
| Mean [SD] | 633 [621] | 789 [578] | 0.15 |
| Missing | 16 (48.5) | 27 (47.4) | |
| Treatmentd | |||
| HCQ | 17 (51.5) | 48 (84.2) | |
| AZM | 17 (51.5) | 47 (82.4) | |
| LPV/RTV | 16 (48.4) | 49 (85.9) | |
| CRO | 0 (0) | 35 (61.4) | |
| LFX | 0 (0) | 6 (10.5) | |
| BMPr | 0 (0) | 12 (21.0) | |
| IFN | 0 (0) | 5 (8.7) | |
| TOZ | 0 (0) | 5 (8.7) | |
| QFT results in each tube, IU/mL | |||
| Nil tube | |||
| Mean [SD] | 0.297 [0.754] | 0.124 [0.106] | 0.52 |
| Tb1 tube | |||
| Mean [SD] | 0.979 [2.25] | 0.512 [1.26] | 0.17 |
| Tb2 tube | |||
| Mean [SD] | 0.985 [2.27] | 0.557 [1.38] | 0.81 |
| Mitogen tube | |||
| Mean [SD] | 5.04 [2.80] | 3.35 [2.80] | 0.03 |
Abbreviations: PHA, phytohemagglutinin; HCQ, hydroxychloroquine; AZM, azithromycin; LPV/RTV, lopinavir/ritonavir; CRO, ceftriaxone; LFX, levofloxacin; BMPr, bolus 6-methylprednisolone; IFN, interferon alpha-2b; TOZ, tocilizumab; QFT, QuantiFERON™ TB Gold Plus.
Suspected COVID-19 pneumonia was based on clinical and/or radiological evidence of pneumonia, or acute respiratory distress but with negative or indeterminate RT-PCR for SARS-CoV-2 results from respiratory specimens during the first peak of COVID-19 pandemic in Asturias (March 2020).
A total of 49 out of 90 patients (54.4%) showed low or very low IFN-γ response to PHA, including 16 with QFT-Plus indeterminate results (due to very low IFN-γ response to PHA) and another 33 patients who, although they met the manufacturer criteria to validate the QFT results as negative (N=29) or positive (N=4), showed low IFN-γ response to PHA. The age range was very similar in both groups (17 and 32 patients vs. 17 and 24 patients, for <65 years old and elderly respectively). In Table 2, we compared both the RT-PCR SARS-CoV-2 results and the response to PHA in the QFT assay. Abnormal radiological findings but no disease severity or other laboratory abnormalities showed statistical significance association with low mitogen response in the QFT assay. No patients received immunosuppressive drugs prior to the blood collections for the QFT assay.
Prospective Cohort, PHA Responses in QFT by Radiological, COVID-19 Disease Severity, and Laboratory Abnormalities Accord to RT-PCR SARS-CoV-2 Results.
| Number of patients included | RT-PCR-SARS-CoV-2 results | PHA normal response | PHA low/very low response | P valuec | QFT-Positive | |
|---|---|---|---|---|---|---|
| Chest radiographn=90 | Chest X-rays findings of pneumonia78/90 | 51 Positive4 Indeterminate23b Negative | 19115 | 3238b | 0.01d | 6 (1 PHA normal, 5 PHA low/very low)1 (1 PHA normal)2 (2 PHA normal) |
| Normal chest radiograph12/90 | 6 Positive2 Indeterminate4 Negative | 123 | 501 | 0.11 | 1 (1 PHA low/very low)01 (1 PHA normal) | |
| COVID-19 disease severityn=90 | Mild/Moderate disease68/90 | 37 Positive6 Indeterminate25 Negative | 17316 | 2039 | 0.38 | 5 (1 PHA normal, 4 PHA low/very low)1 (1 PHA normal)3 (1 PHA normal) |
| Severe/Critical disease22/90 | 20 Positive0 Indeterminate2 Negative | 400 | 1602 | 1.00 | 2 (2 PHA low/very low)00 | |
| Lymphocyte count (109L)n=74 | ≥1.033/74 | 20 Positive2 Indeterminate11 Negative | 1105 | 926 | 0.48 | 2 (2 PHA low/very low)01 (1 PHA normal) |
| <1.041/74 | 31 Positive2 Indeterminate8 Negative | 814 | 2314 | 0.23 | 5 (1 PHA normal, 4 PHA low/very low)00 | |
| Ferritinn=47 | ≥400 ng/mL35/47 | 27 Positive1 Indeterminate7a Negative | 704 | 2013a | 0.24 | 5 (1 PHA normal, 4 PHA low/very low)00 |
| <400 ng/mL12/47 | 4 Positive2 Indeterminate6 Negative | 404 | 022 | 0.09 | 002 (1 PHA normal, 1 PHA low/very low) | |
| D-dimern=70 | ≥1 ng/mL25/70 | 19 Positive0 Indeterminate6a Negative | 303 | 1603a | 0.12 | 5 (1 PHA normal, 4 PHA low/very low)01 (1 PHA normal) |
| <1 ng/mL45/70 | 28 Positive3 Indeterminate14a Negative | 1519 | 1325a | 0.63 | 2 (1 PHA normal, 1 PHA low/very low)00 | |
| Procalcitoninn=32 | ≥0.5 ng/mL4/32 | 2 Positive0 Indeterminate2 Negative | 000 | 202 | 1.00 | 000 |
| <0.5 ng/mL28/32 | 19 Positive3 Indeterminate6 Negative | 623 | 1313 | 0.51 | 3 (1 PHA normal, 2 PHA low/very low)01 (1 PHA normal) | |
| Alanine aminotransferasen=72 | ≥40 U/L35/72 | 26 Positive1 Indeterminate8 Negative | 905 | 1713 | 0.22 | 4 (1 PHA normal, 3 PHA low/very low)01 (1 PHA normal) |
| <40 U/L37/72 | 22 Positive1 Indeterminate14 Negative | 1008 | 1216 | 0.61 | 3 (3 PHA low/very low)1 (1 PHA normal)1 (1 PHA normal) | |
| Lactate dehydrogenasen=76 | ≥480 U/L32/76 | 25 Positive1 Indeterminate6 Negative | 500 | 2016 | 0.62 | 4 (1 PHA normal, 3 PHA low/very low)00 |
| <480 U/L44/76 | 26 Positive3 Indeterminate15 Negative | 15112 | 1123 | 0.15 | 3 (3 PHA low/very low)01 (1 PHA normal) |
Abbreviations: PHA, phytohemagglutinin; QFT, QuantiFERON TB Gold Plus; PHA very low, very low IFN-gamma response to PHA when IFN-gamma concentration (minus Nil) in mitogen tube <0.5 IU/mL; PHA low, low IFN-gamma response to PHA when IFN-gamma concentration (minus Nil) ≥ 0.5 IU/mL in mitogen tube and less than 50% below the average values; PHA normal, normal IFN-gamma response to PHA when IFN-gamma concentration (minus Nil) ≥ 0.5 IU/mL in mitogen tube and at least more than half of the average value.
P value for comparison of clinical, radiological or laboratory findings between group with normal vs. low-response to PHA in QFT assay in patients with confirmed COVID-19 pneumonia diagnosis (i.e. positive RT-PCR and/or serum anti-SARS-CoV-2 IgG-IgM results) and patients with negative or indeterminate RT-PCR SARS-CoV-2 test results by the r x c Exact contigency test.
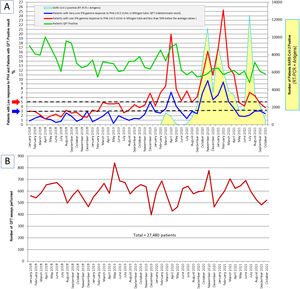
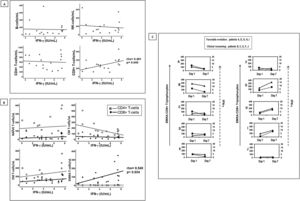
We studied seventeen elderly patients (fifteen of them lived in the same nursing home) that were admitted to the hospital for observation after being diagnosed of COVID-19. Study subjects underwent serial blood testing for QFT and whole-blood immune profiling. We found that production of IFN-γ in whole blood stimulated with PHA varied greatly in these COVID-19 patients. We quantified the different lymphocyte subsets to attempt to identify cells associated with abnormal IFN-γ response to PHA. PHA is a polyclonal activator of T-cells and thus, B and NK-cell counts were not related to IFN-γ production. The number of CD4+T-cells subsets also did not correlate with IFN-γ response to PHA in these patients; however, the total number of CD8+T-cells showed an statistical significant correlation with IFN-γ levels (rho=0.491, P=0.04) (Figure 3A). Then, we analyzed functionally different populations of T-cells separated by using combinations of cell surface markers CD45RA and the chemokine receptor CCR7. Using these markers, we subdivided the T-cells into naïve (naïve, CD45RA+CCR7+), central memory (CM, CD45RA-CCR7+), effector memory (EM, CD45RA-CCR7-), and effector memory RA (EMRA, CD45RA+CCR7-) from less to more differentiated T cell stages 11 (Figure 3B). The analysis of the CD4+T-cells subsets revealed no statistically significant correlations; however, the number of EMRA CD8+T-cells also showed an statistical significant correlation with IFN-γ response levels to PHA in whole blood of these patients with COVID-19 and abnormal QFT-Plus results (rho=0.540, P=0.03).
Immunophenotyping of Lymphocytes and T Cell Subsets and IFN-γ Level Responses to Phytohemagglutinin (PHA).
A) Pearson correlations between lymphocyte subsets counts and IFN-γ level responses to PHA in whole blood of patients with COVID-19 pneumonia, including statistical significant correlations in CD8 T-cell counts and IFN-γ level responses to PHA (lower right-side quadrant; P <0.05). B) Statistical significant positive correlations in EMRA CD8 T-cell counts and IFN-γ level responses to PHA (lower right-side quadrant; P <0.05). C) EMRA CD8+T-cell Counts (solid line with triangles) and IFN-γ Response Levels (IU/mL) to PHA (dashed line with squares) at Days 1 and 7 After Hospital Admittance of Ten QFT-monitored Patients (named A to J). Their Clinical Evolution is Also Included. Left, 5 patients with initial normal response to PHA at day 1 (four of them had low/very low response to PHA at day 7); Right, 5 patients with initial low/very low response to PHA at day 1 (three of them had normal response to PHA at day 7).
Ten out of seventeen study patients had a follow-up QFT testing and immune profiling a week later (Table-3; Figure 3C). A statistical significant positive correlation was again observed with EMRA CD8+T-cell counts and IFN-γ response levels to PHA (data not shown). In those patients with more than 100 EMRA CD8+T-cells/μL (5 out 10), the increase or decrease in the levels of IFN-γ and in this lymphocyte subpopulation occurred in the same direction. On the contrary, those patients with less than 100 cells/μL showed no recovery in either the number of cells or IFN-γ response levels to PHA (Figure 3C).
DiscussionSince December 2019, we observed an unprecedented increase in the rate of low IFN-γ responses to PHA in the QFT-Plus assay. These abnormal immune response findings were especially pronounced during the first four waves of the COVID-19 epidemic in our region from March to May 2021 (Figure 1A), suggesting that the findings were related to biologic effects of COVID-19. We have also observed that this low mitogen response in the QFT assay is more often present in patients with confirmed COVID-19 pneumonia compared with patients with suspected COVID-19 pneumonia but with negative RT-PCR test for SARS-CoV-2 virus, further supporting the association between COVID-19 and low mitogen responses. Further, subgroup analysis showed that the presence of chest x-ray abnormalities were associated with abnormal QFT mitogen response in our univariate analysis, again suggesting that the low IFN-γ responses to PHA were associated with true COVID-19 pneumonia.
Other studies have also reported a similar increase frequency of low IFN-γ response to mitogen and indeterminate QFT results in hospitalized patients with COVID-19, including patients with severe and critical COVID-19 and hyperinflammatory syndrome 12,13. Interestingly, indeterminate QFT results were more frequent among COVID patients who died during hospitalization in a retrospective study from Spain (29.1% vs. 64.7%) 13, but these abnormal QFT results were not associated with increased mortality in a study from the United States 12. However, these studies did not adjust these survival analyses to other known factors associated with increased mortality in COVID-19, including older age, male sex, and various comorbidities 14.
Reduced IFN-γ responses to PHA stimulation are common in certain clinical scenarios. Most often, they are observed in immunosuppressed patients, both those with underlying immunodeficiency and those on immunosuppressive treatments 15,16. Importantly, none of the patients in our cohort received immunosuppressive drugs for the treatment of COVID-19 prior to undergoing IGRA testing. Specific immune dysfunctions are also well-established to increase the rate of indeterminate IGRA tests, including the low CD4 counts of HIV and the T cell exhaustion exhibited among critically-ill patients and patients with active lupus erythematosus 17,18. However, in our study, patients with low IFN- γ responses did not have reduced CD4 counts, and we did not find an association between severity of COVID-19 and low mitogen response, which argues against T-cell exhaustion. However, T-cell exhaustion and complex immune activation are common in patients with COVID-19 pneumonia, and we cannot exclude these pathophysiological factors playing a role 19. In addition, in patients with inflammatory bowel disease, low serum albumin, lymphopenia, and corticosteroid therapy have been associated with increased odds to have indeterminate IGRA results with low mitogen response in a multivariate analysis 20. In our study, we did not analyze serum albumin levels but the presence of lymphopenia had a trend towards statically significant association with a low mitogen response in the QFT assay. Another study with critical COVID-19 patients found no direct association between lymphopenia, inflammatory markers, or severity of COVID-19 with QFT indeterminate results 12; however, some of those critically-ill COVID-19 patients received immunosuppressive treatments, which was not a cofounder in our study. Occasionally, indeterminate response can be seen related to technical problems inherent to the assay variability of any immunodiagnostic test (pre-analytical, analytical and post-analytical phases). However, we were unable to identify any analytical laboratory factor or patient-related immunosuppressive factors to explain these study laboratory findings.
In our prospective study cohort with T cell immune profiling data, a reduction in total CD8 T cell counts and differentiated CD8 EMRA T-cell subset were statistically associated with the observed reduction in IFN-γ responses to PHA stimulation in the QFT-Plus assay. Lymphopenia with preferential peripheral blood CD8+T-cell reduction has been described in COVID-19, but the mechanism of the observed frequent reduction in IFN-γ responses to PHA activation in the QFT-Plus assay is not entirely clear 21. Recent reports suggest the presence of T cell and NK cell dysfunction and exhaustion phenotypes associated with a hyperactivation immune state during COVID-19. This phenomenon is suggested by overexpression of CD69, a marker of activation, and TIM-3 on NK, CD4 and CD8 T cells. TIM-3 is a negative regulator of immune cell function and its ligands induces T and NK cell exhaustion in viral infections 22. Along these lines, another study showed that a small subset of critically-ill COVID-19 patients with indeterminate QFT results had increased IL-10 levels and reduced Th1-related cytokine levels, which the authors suggest a relationship with Th2 immune responses in this setting. However, recent immune profiling data in patients with COVID-19 pneumonia showed not only increase Th2 response can be observed but also a global immune and inflammatory activation process that includes complex immunoregulatory mechanisms and T-cell exhaustion that can affect Th1-immune response, including IFN-γ responses to activating factors 19. In addition, there is CD8 T cell dysfunction in elderly patients with COVID-19, and EMRA CD8+T-cell subsets also display a senescence-associated secretory phenotype that may contribute to age-related inflammation in COVID-19 23,24. Interestingly, there was a trend towards an older age in the study group with low mitogen response in the QFT compared with the group with normal mitogen response in our study (Table 1). In this context, there are increasing numbers of reported cases of COVID-19 and TB co-infection 25,26. In fact, there is also a concern that viral infections, including COVID-19, could have a pathophysiologic effect on TB progression and TB reactivation in LTBI 27–30. However, the clinical implications of these abnormal CD8+T cell responses associated with COVID-19 for other infections, including potential for TB reactivation in the future, are unclear at this time of the pandemic.
Importantly, some experts suggested that the use of IGRA to screen for TB infections in patients with severe COVID-19 has limited value11,31. Our study results show the overall number of patients with a positive QFT result remained unchanged before and during the pandemic (13.95% vs. 12.2%, respectively). We also did not find there any significant difference in rates of “positive” response to the QFT Mtb specific antigens in those patients with low/very low PHA response in the mitogen tube before and during the pandemic (6.2% vs. 7.9%; and 1.3% vs. 2.1%; for low and very low response to PHA, respectively). Moreover, some of our hospitalized COVID-19 patients showed “positive” Mtb antigen-specific responses (≥0.35 IU/mL) despite transiently or persistent low response to mitogen in repeat QFT testing (Table 3). Overall, our results suggest considering repeating QFT testing in 3-7 days in patients with COVID-19 pneumonia with risk factors for Mtb infection, particularly in those patients with “positive” Mtb specific antigen response.
Clinical Data From 10 (named A to J) Patients* With Follow-up QuantiFERON TB Gold Plus During COVID-19 Pandemic.
| Patient | Symptoms at disease onset | Chest X-rays findings | Gender | Age | Comorbidity | PO2 sat. | Flu-vaccine | RT-PCR | PHA response | Leucocytes | Lymphocytes | QFT | D-dimer | LDH | Ferritin | Procalcitonin | ALT | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ID | % | SARS-CoV-2 | Day 1 | Day 1 | Day 1 | |||||||||||||
| Day 3 | - | - | ||||||||||||||||
| Day 7 | Day 7 | Day 7 | ||||||||||||||||
| A | Asymptomatic | Basal right infiltrate | Female | 83 | UTIs | 92 | yes | Pos | 7.61 Normal | 5590 | 960 | Pos | 3524 | 199 | 180 | 0.06 | 21 | HCQ |
| 2.65 Low | - | - | AZM | |||||||||||||||
| 2.67 Low | 3340 | 360 | ||||||||||||||||
| B | Abdominal pain | Bilateral infiltrate | Female | 76 | Diabetes | 97 | yes | Pos | 6.97 Normal | 4210 | 900 | Neg | 1033 | 260 | 733 | 0.05 | 24 | Non-specific treatment |
| HTN | 2.95 Low | - | - | |||||||||||||||
| Psoriasis | 1.97 Low | 4010 | 840 | |||||||||||||||
| CRF | ||||||||||||||||||
| C | Myalgia | Bilateral infiltrate | Male | 56 | None | 93 | yes | Pos | 5.61 Normal | 2650 | 270 | Neg | 228 | N | 578 | 0.08 | 19 | HCQ |
| Fever | 1.04 Low | - | - | AZM | ||||||||||||||
| 0.69 Very Low | 5230 | 430 | LPV/RTV | |||||||||||||||
| D | Fever | Basal left infiltrate | Female | 91 | Atrial fibrillation arrhythmia | 98 | yes | Pos | 5.31 Normal | 5930 | 1260 | Neg | 5583 | N | 198 | 0.08 | 7 | HCQ |
| Osteoporosis | 5.66 Normal | - | - | AZM | ||||||||||||||
| 4.33 Normal | 7620 | 1420 | ||||||||||||||||
| E | Asymptomatic | Bilateral infiltrate | Female | 85 | Diabetes type 2 | 97 | yes | Pos | 4.51 Normal | 2840 | 810 | Pos | 269 | 227 | 529 | 0.1 | 21 | HCQ |
| HTN | 2.98 Low | - | - | |||||||||||||||
| CRF | 1.04 Very Low | 3520 | 680 | |||||||||||||||
| Basal cell carcinoma | ||||||||||||||||||
| F | Dyspnea | Bilateral infiltrate | Male | 86 | Prostate cancer | 95 | yes | Neg | 3.68 Low | 4530 | 1380 | Neg | 3274 | 345 | 223 | 0.07 | 18 | HCQ |
| Ictus | (IgM/IgG pos) | 2.98 Low | - | - | LPV/RTV | |||||||||||||
| CRF | 0.30 Very Low | 7180 | 1610 | CRO | ||||||||||||||
| HTN | ||||||||||||||||||
| G | Asymptomatic | Bilateral infiltrate | Female | 91 | Ischemic cardiomyophaty | 95 | yes | Pos | 3.28 Low | 4120 | 1860 | Pos | 547 | 326 | NR | 0.09 | 14 | HCQ |
| Ovarian cancer | 0.18 Very Low | - | - | LFX | ||||||||||||||
| 7.87 Normal | 9380 | 1910 | ||||||||||||||||
| H | Cough | Bilateral infiltrate | Female | 74 | HTN | 98 | yes | Pos | 2.93 Low | 5370 | 1350 | Neg | 6367 | 211 | 122 | 0.04 | 13 | HCQ |
| Primary hypothyroidism | 5.75 Normal | - | - | AZM | ||||||||||||||
| 8.12 Normal | 6390 | 2060 | LPV/RTV | |||||||||||||||
| I | Asymptomatic | Rx normal findigns | Female | 81 | Diabetes type 2 | 95 | yes | Pos | 0.83 Low | 7600 | 1100 | Neg | 6327 | 408 | 0.06 | 17 | HCQ | |
| HTN | 4.53 Normal | - | - | AZM | ||||||||||||||
| 8.15 Normal | 5400 | 1470 | ||||||||||||||||
| J | Asymptomatic | Bilateral infiltrate | Male | 71 | HTN | 100 | yes | Pos | 0.07 Very Low | 5350 | 1830 | Pos | 2524 | 169 | 838 | 0.42 | 15 | HCQ |
| Hyperuricemia | 0.19 Very Low | - | - | AZM | ||||||||||||||
| Biliary cirrhosis Ischemic cardiomyophaty | 0.14 Very Low | 5260 | 1220 |
Abbreviations: Rx, chest X-rays; HTN, hypertension; CRF, chronic renal failure; UTIs, urinary tract infections; PHA, phytohemagglutinin; QFT, QuantiFERON TB Gold Plus; LDH, lactate dehydrogenase; ALT, alanine aminotransferase; Pos, positive; Neg, negative; N, normal; HCQ, hydroxychloroquine; AZM, azithromycin; LPV/RTV, lopinavir/ritonavir; CRO, ceftriaxone.
Of note, the first confirmed COVID-19 case in Spain was officially reported in February 2020 but we observed an unexpected high rate of abnormal QFT mitogen response since December 2019 in our study. If our hypothesis holds true, our study laboratory findings also suggest that the COVID-19 epidemic may have started earlier in our region (Figure 1 A). This study finding also suggests that monitoring the rate of low mitogen response in the QFT-Plus assay can be utilized as an epidemiological screening tool for early detection of COVID-19 epidemics that could trigger more specific testing of suspected cases and undiagnosed patients with pneumonia in the community. The complexity (logistics and cost) inherent to a mass COVID-19 screening strategy is unquestionable. In our region, the results observed (at least with regard to the evolution of the number of deaths due to COVID-19 and the temporal correlation with the different pandemic waves) were, surprisingly, identical to those registered with about 2 million diagnostic tests performed for COVID-19 between March 2020 and October 2021, compared to 12,837 QFT assays (mean 642 test/month). Moreover, in contrast with previous epidemic waves, during the fifth wave, the number of cases with RT-PCR SARS-CoV-2 positive increased in our region, while severe cases and mortality were significantly reduced, and also the number of patients with low IFN-gamma response to PHA in the mitogen tube. This situation could be explained because in most cases were young people with mild symptoms, as well as by the high degree of vaccination coverage in our region. We think that these findings support the hypothesis of a potential population-based marker of COVID-19-related mortality but additional studies would be needed to determine if this marker is sensitive and specific for early detection and prediction of COVID-19-related mortality at the population based level.
Our study has some potential limitations, including the observational nature of the study design and the relatively limited number of hospitalized patients studied in the cohort part of the study. A small number of subjects can lead to suboptimal power to differentiate true differences in the study subgroups. Multiple comparison analysis can also increase the risk of false discovery rates. However, we believe that our study cohort was representative of patients suspected of and confirmed COVID-19 pneumonia in our region during the first peak of the pandemic given the referral nature of our laboratory and hospital services. Our study also has several strengths, including the centralized nature of our laboratory services that allow us to capture the high frequency of QFT testing utilization and LTBI screening results in our entire region during the pandemic. In addition, our study benefited from the excellent epidemiological tracking of COVID-19 cases and their laboratory results in our region in Spain. In addition, the prospective nature of our multifactorial and immune profiling investigations is another important strength of our study.
In conclusion, our study findings suggest that low IFN-γ responses in the mitogen control tube of the QFT-Plus assay often occur in COVID-9 pneumonia, which can be utilized as a surveillance tool to track the COVID-19 pandemic waves. These abnormal QFT-Plus results were likely related to a suboptimal number and response of a subset of differentiated CD8 T cells to PHA associated with SARS-CoV-2 infections. The clinical implications of these abnormal immune responses in COVID-19 for other infections, including the potential for an increase in TB reactivation rates in the future, are unclear at this time of the pandemic. However, this abnormal mitogen response does not seem to affect the IFN-γ response to specific Mtb antigens in COVID-19 patients, and thus, we propose to revisit and redefine the QFT-Plus indeterminate test results criteria in this setting.
Ethics approval:Ethical clearance was approved by the Comité de Ética de la Investigación del Principado de Asturias, Spain
Transparency declaration:The authors have no conflicts of interest to declare.
Funding:None