Exacerbations of chronic obstructive pulmonary disease (COPD) impact the natural history of the disease.1 The latest edition of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) consensus document2 classified exacerbation severity by the treatment prescribed and/or the health resources used. However, new proposals for classifying the severity of COPD exacerbations have recently emerged. The 2021 Spanish COPD guidelines (GesEPOC)3 propose a new classification of exacerbations based on baseline risk stratification, modified Medical Research Council (mMRC) dyspnea grade, altered level of consciousness, respiration rate, and gas exchange. COPD exacerbations are classified using these variables as mild, moderate, severe, or very severe (the last 2 being defined as exacerbations requiring hospitalization). Recently, a group of experts proposed another classification based on 5 variables (dyspnea measured on a visual analogue scale [VAS], respiratory rate, heart rate, C-reactive protein, and gas exchange) that categorizes exacerbations as mild, moderate, or severe.4 This classification differs from GesEPOC in that it does not take into account the baseline situation of the patient and requires that at least 3 criteria be met to escalate severity from mild to moderate. As a result, discrepancies may be expected in the classification of COPD exacerbation severity. However, this hypothesis has not been explored.
The objectives of this study were (1) to evaluate the overall concordance between the GesEPOC 2021 criteria and the Rome proposal, and (2) to analyze the degree of agreement between the 2 proposals with respect to the number of serious events (admissions or in-hospital deaths) and the DECAF score.5 To this end, after obtaining approved from the Ethics Committee of our institution, we conducted a retrospective study in which we consecutively recruited patients with a previous diagnosis of COPD admitted for COPD exacerbation to a third-level hospital between 2020 and 2021. The following variables routinely collected in our hospital's medical records were analyzed: (1) the patient's baseline situation [age, sex, forced expiratory volume in 1 second (FEV1) % post-bronchodilator; classification according to their history of previous exacerbations as either an exacerbator (≥ 2 exacerbations treated with corticosteroids and/or antibiotics or an admission due to COPD exacerbation in the previous year) or a non-exacerbator (did not meet the above criteria); baseline dyspnea according to the mMRC scale, and quality of life according to the COPD assessment test (CAT). Patients were classified according to GesEPOC 2021 as high risk (meets any of the following criteria: FEV1%<50%, mMRC>1, exacerbator) or low risk (meets all the following criteria: FEV1%≥50%, mMRC 0–1, and non-exacerbator)]; and (2) their status upon arrival at the emergency department (extended mMRC dyspnea scale, blood eosinophilia, consolidation on chest X-ray, blood gas values, atrial fibrillation, level of consciousness, respiratory and heart rate, oxygen saturation, and C-reactive protein levels). The Rome scale classifies exacerbations on the basis of a VAS score. As this scale is not routinely used, this criterion was changed to a 1-point increase in the degree of dyspnea on the mMRC scale, based on a degree of correlation between the 2 scales.6 Patients were classified according to the different proposals, and the DECAF predictor score of in-hospital mortality associated with COPD exacerbation was calculated (DECAF: dyspnea, eosinopenia, consolidation, acidosis, and atrial fibrillation); a higher score on this scale is associated with higher mortality in patients admitted for COPD exacerbation. The number of patients who developed serious events (ICU admission or in-hospital death) was also recorded.
We included 200 patients who were admitted during the study period (10 cases were excluded because variables needed to calculate the scales were missing). Two-thirds (67.5%) were men, with an age of 75.1±10.9 years, FEV1% post-bronchodilator 49% (34–65%), CAT at last stable consultation 12.0±9.3 points; 24 patients (12%) were low-risk COPD according to GesEPOC, and 137 (68.5%) were exacerbators.
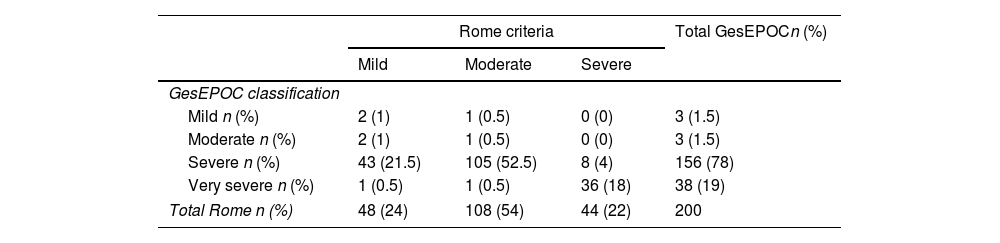
Table 1 shows the overall concordance between the classification of the COPD exacerbations according to the GesEPOC and the Rome criteria. The GesEPOC criteria categorized 3% of exacerbations requiring hospitalization as mild or moderate, while the Rome criteria categorized 24% as mild. The degree of concordance between the 2 classifications was Kappa: −0.157, 95% CI −0.109 to −0.205, p<0.001. When GesEPOC mild and moderate exacerbations were combined, the Kappa index was 0.481, 95% CI (0.382–0.585), p<0.001.
Overall agreement between groups according to the Rome and GesEPOC classifications in patients admitted for COPD exacerbation.
| Rome criteria | Total GesEPOCn (%) | |||
|---|---|---|---|---|
| Mild | Moderate | Severe | ||
| GesEPOC classification | ||||
| Mild n (%) | 2 (1) | 1 (0.5) | 0 (0) | 3 (1.5) |
| Moderate n (%) | 2 (1) | 1 (0.5) | 0 (0) | 3 (1.5) |
| Severe n (%) | 43 (21.5) | 105 (52.5) | 8 (4) | 156 (78) |
| Very severe n (%) | 1 (0.5) | 1 (0.5) | 36 (18) | 38 (19) |
| Total Rome n (%) | 48 (24) | 108 (54) | 44 (22) | 200 |
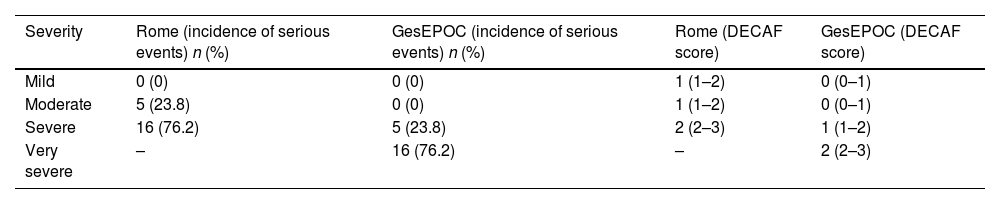
Table 2 shows that the incidence of serious events (admission to ICU or in-hospital death) associated with moderate exacerbations according to Rome and severe exacerbations according to GesEPOC is the same [5 (23.8%)] and is also the same in severe cases according to Rome and very severe cases according to GesEPOC [16 (76.2%)]. The DECAF score was the same for both moderate exacerbations according to Rome and severe exacerbations according to GesEPOC [1 (1–2)] and for severe exacerbations according to Rome and very severe exacerbations according to GesEPOC [2 (2–3)].
Incidence of severe events during hospital stay and DECAF score in patients according to the different classifications.
| Severity | Rome (incidence of serious events) n (%) | GesEPOC (incidence of serious events) n (%) | Rome (DECAF score) | GesEPOC (DECAF score) |
|---|---|---|---|---|
| Mild | 0 (0) | 0 (0) | 1 (1–2) | 0 (0–1) |
| Moderate | 5 (23.8) | 0 (0) | 1 (1–2) | 0 (0–1) |
| Severe | 16 (76.2) | 5 (23.8) | 2 (2–3) | 1 (1–2) |
| Very severe | – | 16 (76.2) | – | 2 (2–3) |
Serious event=ICU admission or in-hospital death.
Our study reveals a mismatch between the 2 scales, especially with regard to COPD exacerbations classified as mild. This may be for 2 reasons: (1) GesEPOC, unlike the Rome scale, takes into account the patient's baseline situation to categorize patients as mild, a variable that is used in clinical decision-making; and (2) in the Rome scale, to escalate severity, 3 of its severity criteria must be met, while GesEPOC increases in severity when only 1 of its criteria is met. This would explain the lower DECAF scores in the group of patients with mild GesEPOC exacerbations, compared with the Rome proposal.
Our study has several limitations: (1) it is a retrospective study based on data from a single center and may be subject to local influences; (2) it only allows the applicability of the criteria to be assessed in the hospital setting and not in the primary care setting; (3) the VAS scale recommended by the Rome scale was not used to classify patients; instead, an alternative definition based on modification of the baseline functional grade was used. This modification has a low impact on our series since it would only change the classification of an exacerbation from mild to moderate (0.5%), so the classification of 19 patients (9.5%) may have changed from moderate to mild if the VAS had been used.
This is the first study to evaluate the differences between the 2 new scales used to classify the severity of COPD exacerbations. It assesses the incidence of serious events in the classifications, and helps interpret both scales. If we combine the mild and moderate exacerbations of GesEPOC, there is moderate agreement between the 2 classifications. However, when the Rome proposal was applied, we found a significant number of mild exacerbations among hospitalized patients, along with a considerable number of moderate exacerbations, that subsequently developed serious events during their stay. The differentiation between severe and very severe exacerbations offered by GesEPOC may be useful in the setting in which our study was conducted, as it clearly separates serious events from the DECAF index, while the Roma classification lacks this capacity. The authors of these proposals only partially define the usefulness of severity levels in clinical decision-making. GesEPOC specifies the level of care at which each level of severity should be treated, but the Rome proposal does not, and neither clearly states the therapeutic options available at each step. The patient's baseline situation is often used in clinical practice for decision-making, and this approach seems to confer greater precision to GesEPOC, although it may be more relevant for exacerbations treated on an outpatient basis, which were not the focus of this study. A prospective validation of the different proposals and a deeper exploration of their prognostic utility and their applicability in making therapeutic decisions remains pending.
Conflict of interestsThe authors declare conflict of interests in the manuscript: Juan Marco Figueira Gonçalves has received honoraria for speaking engagements and funding for conference attendance from Laboratories Esteve, MundiPharma, AstraZeneca, Boehringer Ingelheim, Ferrer, Menarini, Rovi, GlaxoSmithKline, Chiesi, Novartis, and Gebro Pharma. Rafael Golpe has received honoraria for speaking engagements and funding for conference attendance from Laboratorio Esteve, Mundipharma, AstraZeneca, Boehringer Ingelheim, Ferrer, Menarini, Rovi, GlaxoSmithKline, Chiesi, Novartis, and Gebro Pharma. Cristóbal Esteban has received speaker fees and research grants from GlaxoSmithKline, Menarini, and AstraZeneca. Carlos Amado Diago has received honoraria for speaking engagements and/or scientific consultancy from Boehringer Ingelheim, Pfizer, AstraZeneca, Novartis, Chiesi, Faes Farma, Esteve, and GlaxoSmithKline. Ignacio Garcia Talavera has received honoraria from GSK, AstraZeneca, Pfizer, Chiesi, and Grifols for speaking engagements, studies and/or scientific consultancy. Sergio García Martín declares no conflict of interests.