A 71-year-old male patient presented with a 1-year history of productive cough with mild hemoptysis, progressive shortness of breath, and left-side ventilatory-dependent chest pain associated with 10kg weight loss in the past 6 months. He also reported night sweats associated with sporadic chills in the past 2 months, and use of amoxicillin for 7 days without symptom improvement. The patient denied fever and other symptoms. He had a past history of hypertension, diabetes, and a 30-pack-year smoking habit (he quit at 42 years of age). He denied a history of previous pneumonia or tuberculosis. The patient had a previous occupational history as a bricklayer, store watchman, farmworker, and roof tile cutter. He referred to past domestic bird maintenance, which he had stopped 3 years previously. On physical examination, his basal oxygen saturation was 98%; ectoscopy showed that he was emaciated and pulmonary auscultation revealed basal crepitant rales, prominent in the left hemithorax.
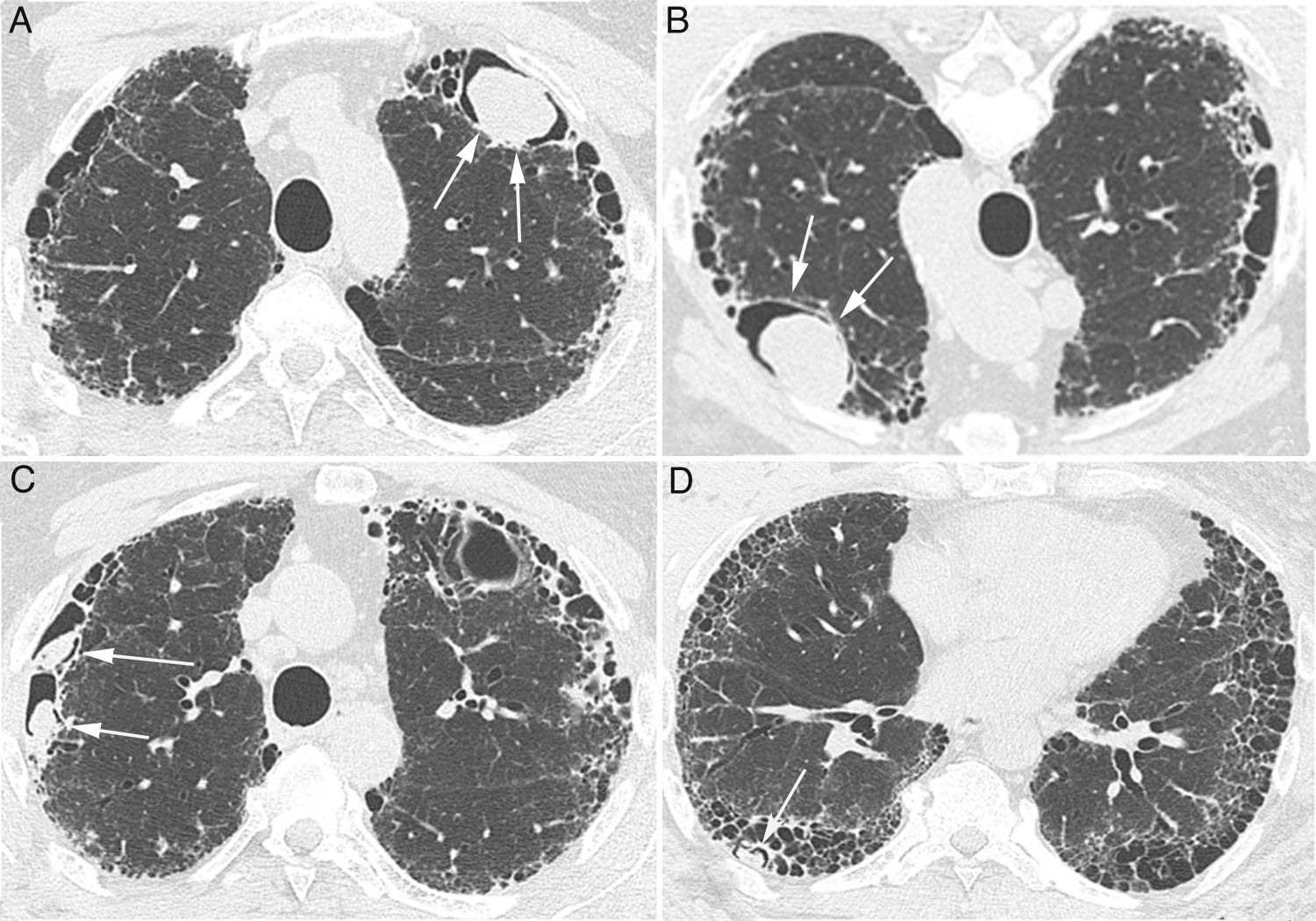
Laboratory test results were normal. A chest X-ray showed diffuse bilateral basal reticular infiltrates and nodular opacity in the left upper lobe. Computed tomography (CT) demonstrated peripheral cystic pattern with thick wall and basal honeycomb, and multiple intracavitary nodules of various sizes, the largest located in the left upper lobe. The larger nodule showed variation in position as the patient's decubitus was changed (Fig. 1), suggesting the diagnosis of aspergilloma (fungus ball). Bronchoalveolar lavage (BAL) was performed and demonstrated the absence of active or residual bleeding. Gram staining of the BAL sample showed paired gram cocci. The study of malignant cells, acid-fast staining and common bacterial culture were negative. Analysis of BAL fluid showed the presence of septate and branched hyphae and positivity for galactomannan (9.26ng/mL; normal, <0.5ng/mL). Serology results were negative for HIV, hepatitis B, and hepatitis C and normal for rheumatoid factor, antinuclear factor, and antineutrophil cytoplasmic antibody.
Chest CT images showing peripheral cysts pattern with honeycomb at the lung bases with an intracavitary nodule positioned anteriorly in the upper left lobe (A) that shifts position when the patient's decubitus is changed (B) (arrows). In C and D, small intracavitary nodules are visible inside cysts in the right lung (arrows).
This patient was diagnosed with saprophytic aspergillosis (aspergilloma) in honeycomb cysts based on imaging characteristics – mainly the characteristic shift of intracavitary nodule positions as the patient's decubitus was changed–along with the demonstration of fungus and positivity for galactomannan, with high values on BAL fluid analysis. The diagnostic hypothesis for the underlying pulmonary disease that caused cysts and honeycomb included pulmonary idiopathic fibrosis, asbestosis, chronic hypersensitivity pneumonia and combined fibrosis and emphysema. The patient was discharged from the hospital with oral itraconazole and levothyroxine, and was managed on an outpatient basis.
Pulmonary aspergillosis can be divided into five types: saprophytic aspergillosis (aspergilloma), hypersensitivity reaction (allergic bronchopulmonary aspergillosis), semi-invasive (chronic necrotizing) aspergillosis, airway-invasive aspergillosis, and angioinvasive aspergillosis. Saprophytic aspergillosis usually develops in a preexistent cavity or ectatic bronchus from underlying disease.1 Tuberculosis is its main cause, followed by conditions such as sarcoidosis, emphysema, bullae or lung cysts, cavitated bronchogenic carcinoma, and pulmonary infarction. Any cavity or cystic space created by underlying pulmonary disease can, theoretically, harbor aspergilloma.2–5 However, studies of the association between aspergilloma and honeycomb cysts are scarce.6–9
Recognition of typical aspergilloma signs is of paramount importance. On CT, the presence of an intracavitary nodule or mass that hangs down as the patient's decubitus is changed strongly suggests this diagnosis. Other findings include the “air crescent sign,” a sponge-like appearance, amorphous calcification within the lesion, and adjacent pleural thickening.