We describe the case of a 73-year-old-man, non-smoker, with recurrent respiratory infections. He had a medical history of bronchiectasis and an asthma/COPD overlap syndrome.
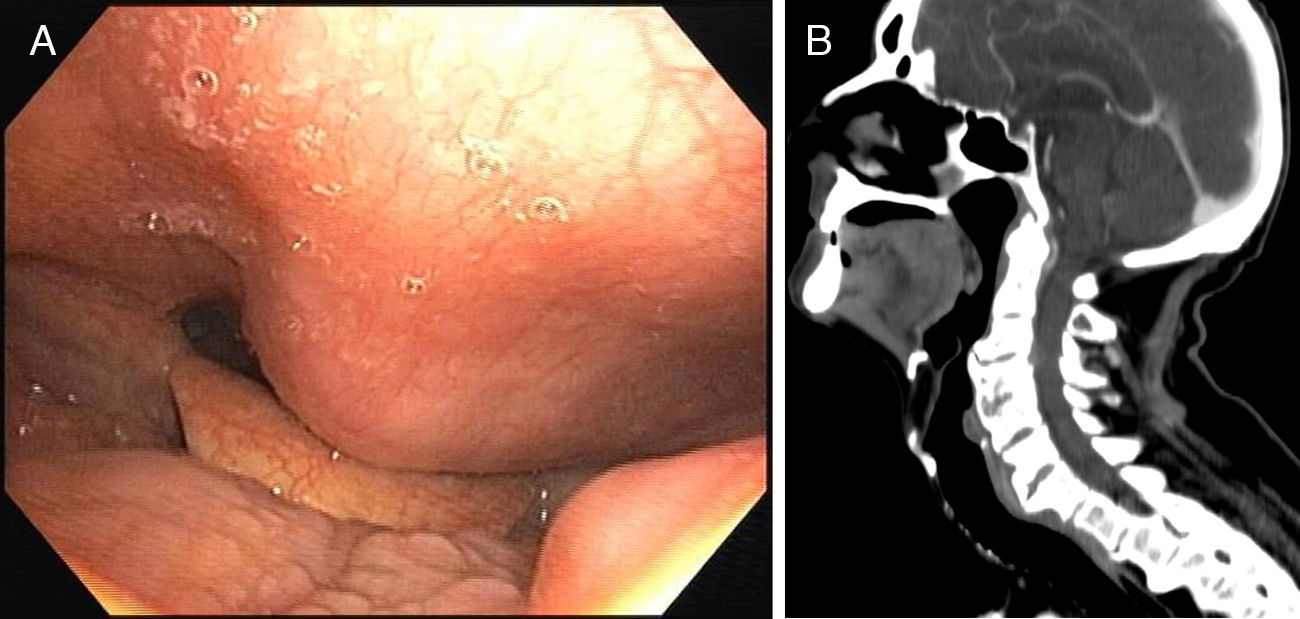
The patient was submitted to a fiberoptic bronchoscopy, which showed a tumefaction in the posterior wall of hypopharynx and inferior oropharynx, approximately 2cm in diameter, with hard consistency and preserved mucosa (Fig. 1A). Cervical computed tomography (CT) revealed extrinsic compression of the posterior wall of pharynx, caused by large osteophytes of the cervical vertebrae (Fig. 1B).
Anterior cervical osteophytes have a prevalence of 20–30% in the elderly population and are diagnosed on the basis of radiologic findings. They are generally asymptomatic; however, in rare cases, they can lead to dysphagia, dysphonia, and dyspnoea.1
Asymptomatic patients, like the case referred, don’t need treatment. Symptomatic patients should be treated according to the severity of disease. Initial conservative management includes diet modifications, muscle relaxants, antireflux and anti-inflammatory medications.2 Surgical intervention (osteophytectomy) is indicated in patients for whom conservative treatment fails and those with respiratory complaints. A tracheostomy is needed concurrently to surgery in individuals with presurgical respiratory complaints.2
Anterior cervical osteophytes can be an important cause of dysphagia and postoperative complications especially in the elderly. Thus, their recognition may be important in the preoperative evaluation of the elderly patient (namely those symptomatic) and in the differential diagnosis of dysphagia.