The Montgomery T-tube (hereinafter referred to as “T-tube”) is a treatment option for tracheal stenosis.1 The indications for T-tube placement are typically temporary preoperative airway support, postoperative surgical reconstruction, or as an alternative method in case of surgical failure (restenosis or nonunion of anastomosis after surgery).2 However, this approach has become an option for patients with benign airway stenosis who are unsuitable or unwilling to undergo surgery, as T-tube placement involves less trauma, is lower risk, is well-tolerated, and allows surgical intervention in cases of failure.3,4 During T-tube insertion, the airway must be shared by a respiratory interventional physician and anesthesiologist, and the use of various modes of mechanical ventilation can complicate anesthetic management. There are few reports regarding anesthetic management during T-tube insertion in patients with complete tracheal stenosis (Myer-Cotton grade 4: occlusion).5 We describe 5 cases of T-tube insertion via rigid bronchoscopy (RB) under general anesthesia with subglottic complete stenosis (Myer-Cotton grade 4) and discuss their anesthetic management.
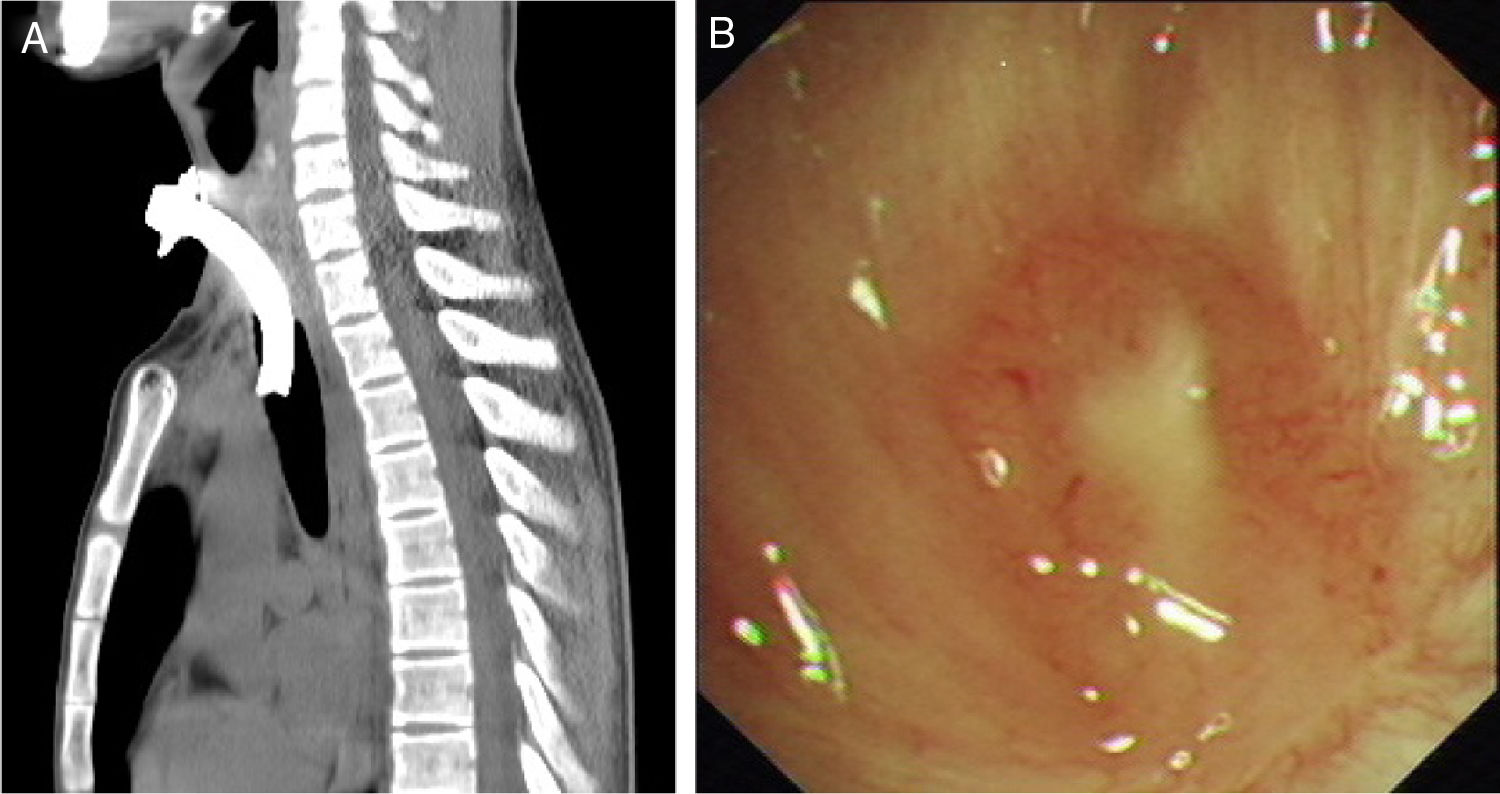
All patients provided written informed consent and the use of clinical data was approved by the Institutional Review Boards of Beijing Tiantan Hospital affiliated to Capital Medical University (JS2013-007-02). Table 1 shows the characteristics of the patients. All five patients refused to undergo surgery and chose T-tube placement (Fig. 1).
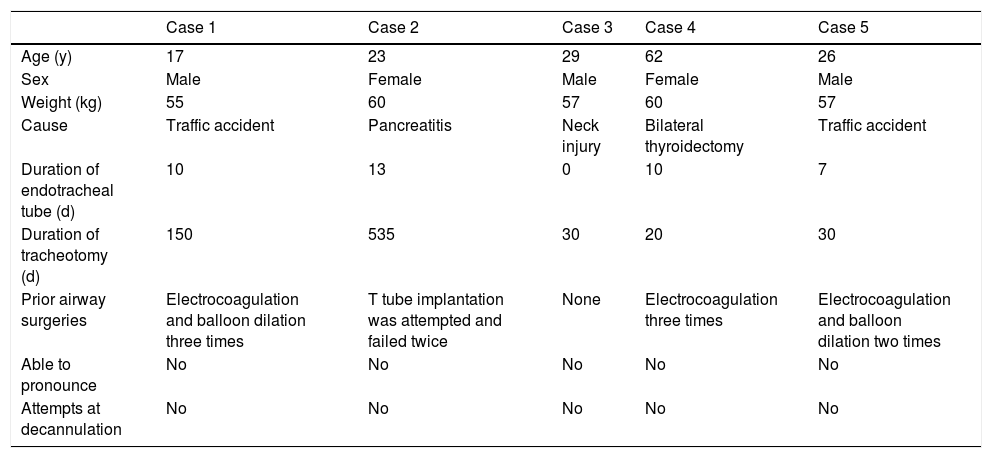
Patients’ characteristics.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Age (y) | 17 | 23 | 29 | 62 | 26 |
| Sex | Male | Female | Male | Female | Male |
| Weight (kg) | 55 | 60 | 57 | 60 | 57 |
| Cause | Traffic accident | Pancreatitis | Neck injury | Bilateral thyroidectomy | Traffic accident |
| Duration of endotracheal tube (d) | 10 | 13 | 0 | 10 | 7 |
| Duration of tracheotomy (d) | 150 | 535 | 30 | 20 | 30 |
| Prior airway surgeries | Electrocoagulation and balloon dilation three times | T tube implantation was attempted and failed twice | None | Electrocoagulation three times | Electrocoagulation and balloon dilation two times |
| Able to pronounce | No | No | No | No | No |
| Attempts at decannulation | No | No | No | No | No |
After intravenous administration of midazolam 0.03mg/kg and sufentanil 0.1–0.2μg/kg, the metal tracheotomy tube was replaced with a 7# disposable plastic cuffed tube connected to a Bain's circuit and attached to a capnometer sampler. Anesthesia was induced with sufentanil 0.1–0.2μg/kg, etomidate 0.3mg/kg, and cisatracurium 0.2mg/kg IV, maintained with propofol 4.5–6mg/kg/h, remifentanil 0.10–0.20μg/kg/min, sufentanil and cisatracurium as required. BIS was maintained 40–60 during operation. After induction of anesthesia, an RB was placed. In cases 2–5, the guide wire passed through the stenosis via RB. Balloon dilators were inserted along the wire to the stenosis segment, and then dilatations were performed. In Case 1, the guide wire was unable to pass through the stenosis via RB because of occlusion. After removal of the tracheotomy tube, the jugular vein needle was passed retrograde from the tracheotomy hole through the stenosis toward the cephalad direction. The guide wire was then placed through the needle. During this process, if SPO2 fell to 85%, the needle was removed and the tracheotomy tube was applied for ventilation until SPO2 returned to 100%. After the guide wire could be observed via RB, the needle was removed; then, the balloon dilator, electro cauterizer, and forceps were inserted via RB along the wire to relieve stenosis. The balloon dilator (No. 5842, Boston Scientific, diameter 12–13.5–15mm) was selected, and the corresponding pressure was 3–5.5–8atm. The times and duration of expansions generally depended on each patient's circumstances.
After relieving stenosis, the tracheotomy tube was removed; the RB, which was connected to a high-frequency ventilator (HFV), was then pushed to the tracheotomy hole. The T-tube was inserted through the tracheotomy hole and placed with the assistance of forceps passing through the RB. The horizontal extraluminal limb of the T-tube was connected to a Bain's circuit through a 7# tracheal tube connector for mechanical ventilation. The RB was removed, and a laryngeal mask (LMA) was placed for mechanical ventilation after closure of the horizontal limb of the T-tube. When EtCO2 reached <45mmHg and the patient had attained consciousness with spontaneous breathing, the LMA was removed. During surgery, dexamethasone 5mg was used to prevent airway edema; in the recovery room, neither intravenous corticosteroids nor other inhaled therapies were used; in the ward, intravenous antibiotics were administered to prevent infection, and neither corticosteroids nor mitomycin were routinely used postoperatively to prevent recurrence. All patients’ procedures were successful.
There are many challenges associated with anesthesia during T-tube implantation.
- 1.
Respiratory management: The primary concern is the selection of a respiratory management method that can both facilitate operation and ensure patient safety. Different teams have reported different methods. Chonchubhair et al.6 reported that before T-tube implantation, they allowed restoration of spontaneous breathing and then planted a piece of elastic colloid bougie along the endotracheal tube and protruded it through the tracheotomy orifice. The bougie was then dragged forcibly to bring the T-tube into the trachea. A tracheal tube for mechanical ventilation was then inserted into the T-tube. The disadvantage of this method was that it did not guarantee safety of the airway during T-tube placement; it increased airway resistance induced by a lesser endotracheal tube. Other studies have proposed several improvements. Sichel et al. used nasogastric tubes inserted into the T-tube for ventilation7; Guha et al. placed an LMA before placement of the T-tube.8 Uchiyama et al.9 used an extension corrugated tube and a carlens (Y) adapter connected to the LMA with one terminal and the horizontal limb of T-tube with the other for ventilation alternately during T-tube implantation. However, these approaches did not involve patients with complete or almost complete closure. To facilitate the use of electrocauterization, balloon dilators or forceps, the interventional physician chose RB for our patients. During elimination of subglottic stenosis, a tracheotomy tube was used for ventilation. During T-tube implantation, the HFV attached to the RB was used to guarantee oxygen supply. When the T-tube was placed, its extraluminal limb was connected to a Bain's circuit through 7# tracheal tube connector for ventilation. After the RB was removed, the extraluminal limb of the T-tube was closed and an LMA was placed for ventilation. The LMA was removed after patients attained spontaneous breathing and conditions for tracheal extubation were satisfied. No hypoxia or airway obstruction occurred.
- 2.
Anesthetic method: In previous reports, T-tube implantation was performed with spontaneous breathing or mechanical ventilation under different anesthetic methods.8,10 Although there are a few studies describing successful T-tube insertion while retaining spontaneous breathing, the obvious cough reflex and vigorous involuntary movements may complicate T-tube insertion and necessitate administration of muscle relaxants.11 We chose RB because of its advantages, such as airway control and provision for HFV, which can help avoid hypoxemia, and availability of operation channels convenient for using forceps to assist placement of T-tube. During this period, the stimulation caused by RB is sufficiently serious that it cannot be suppressed by sedation with topical anesthesia, and the patients’ obvious cough reflex and vigorous involuntary movements must be avoided, as they may complicate T-tube insertion. As the airway was open, we chose total intravenous anesthesia (TIVA), including muscle relaxants, instead of sedation and topical anesthesia. Based on observations from clinical practice, during T-tube insertion for tracheotomy patients with severe or complete subglottic stenosis, TIVA can help maintain an appropriate depth of anesthesia while avoiding intraoperative awareness and severe fluctuations of vital parameters, facilitate RB for HFV, and provide good operative conditions and avoid coughing.
The five patients all had stable vital parameters, depth of anesthesia, and no hypoxemia. This proves that during T-tube insertion for subglottic complete stenosis, TIVA can ensure anesthesia depth, and controlled ventilation or HFV by the tracheotomy tube, RB, T-tube, and LMA on demand can ensure oxygen supply. Thus, this approach is safe and effective.
FundingThis work was supported by a grant from Basic-Clinical Medicine (Tiantan project) Cooperation Fund of Capital Medical University [Grant number: 17JL(TTZX)06], Beijing, China. The funding agency had no role in the study design, the collection, analysis, or interpretation of data, the writing of the report, or the decision to submit the article for publication.