The patient was an 83-year-old non-smoker with B-cell chronic lymphocytic leukemia diagnosed in 2004. Treatment with chlorambucil and prednisone was started in 2010. High-resolution computed tomography of the chest did not reveal bronchiectasis. He had no prior respiratory comorbidities or other respiratory conditions.
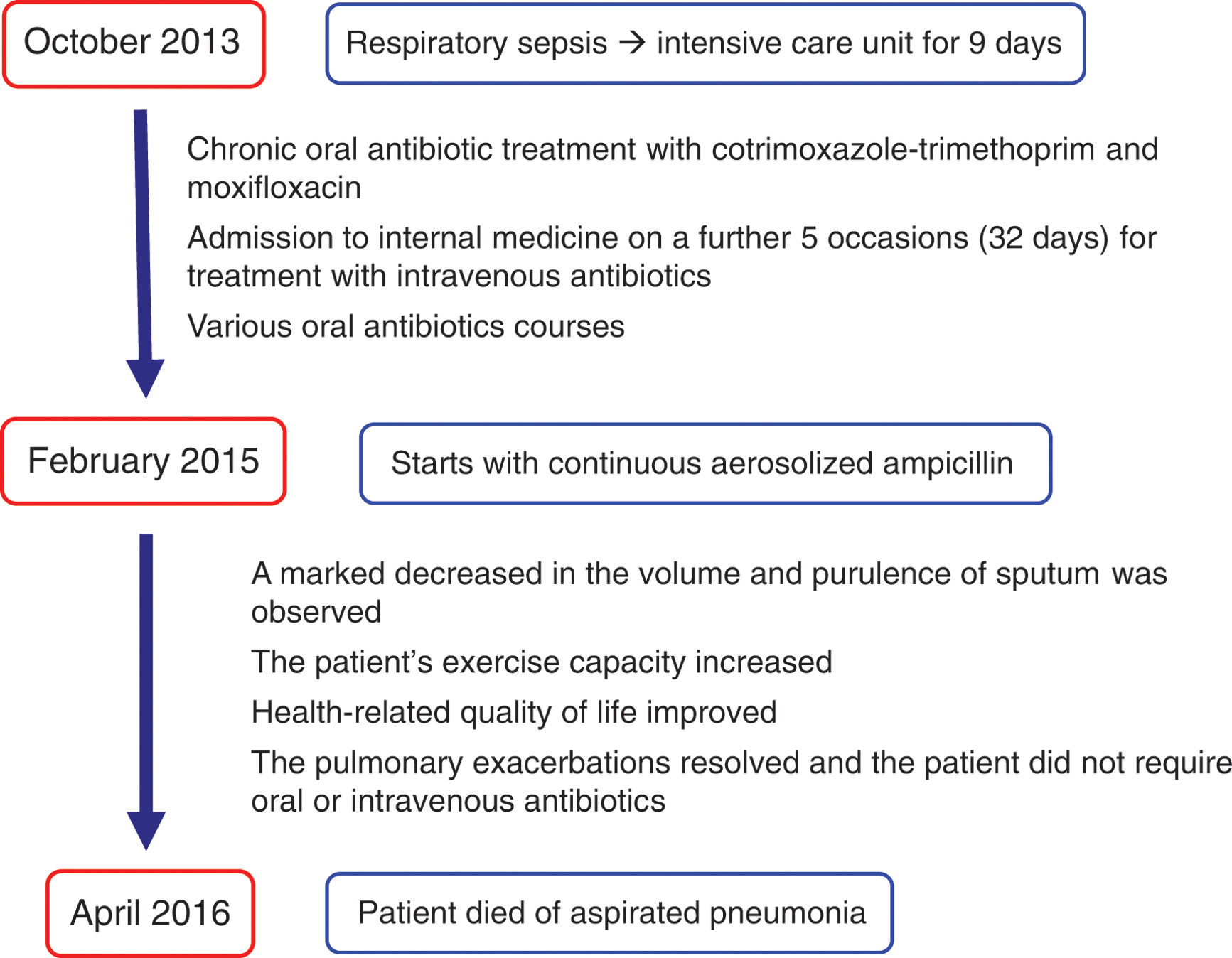
From October 2013, patient started with cough and daily purulent sputum, exertional dyspnea and weight loss. One month later, he was admitted to the intensive care unit for 9 days, followed by 6 days in the internal medicine department because of respiratory sepsis. During the following months, the patient experienced frequent respiratory infections. Hypogammaglobulinemia was discarded. Chronic oral antibiotic treatment with cotrimoxazole-trimethoprim every 2 days and monthly 10-day cycles of moxifloxacin were started in March 2014. The patient was re-admitted to the internal medicine department for 7 days in September 2014 with severe respiratory infection and respiratory insufficiency. From September 2014 onward, the patient continued to experience repeated respiratory infections that were treated with various oral antibiotics. Also, he was admitted to the internal medicine department on a further 3 occasions for treatment with intravenous antibiotics (19 days). None of these episodes were categorized as pneumonia. All acid-fast bacilli smears and sputum cultures for bacteria, mycobacteria, and fungi were consistently negative. Despite recurrent respiratory infections, leukemia treatment could not be suspended due to its progression; even patient had to receive other drugs such as fludarabine, cyclophosphamide, rituximab, bendamustine and pentostatin.
In an attempt to control the recurrent respiratory infections, the patient was informed about other treatment options and gave his informed consent to receive continuous aerosolized ampicillin (February 2015). The aerosolized formulation was administered twice a day after diluting a vial of intravenous sodium ampicillin (Gobemicin®, Normon Laboratories, Madrid, Spain) in 4 cc of sterile water, as previously reported.1 This formulation has an osmolality of 1250 mosmol/kg, with a pH ranging from 8 to 10. The drug was administered using a recommended nebulizer-compressor system for antibiotics (Pari LC Plus high efficiency jet nebulizer [Pari] in combination with a Pari Boy compressor [Pari] [PARI Pharma, Gräfelfing, Germany]). Salbutamol 200mg was administered 30minutes before inhaling ampicillin to prevent bronchoconstriction. Treatment with cotrimoxazole-trimethoprim and moxifloxacin was stopped. It was decided not to perform bronchoscopy with bronchoalveolar lavage due to the good response to inhaled antibiotics that other patients with recurrent respiratory infections had previously had without isolation of potentially pathogenic microorganisms. Two weeks after starting ampicillin, his clinical condition marked improve. After 14 months of treatment with ampicillin, the respiratory infections had resolved, and the patient did not require oral or intravenous antibiotics. A marked decreased in the volume and purulence of sputum was observed, and the patient's exercise capacity increased; no adverse effects were observed. Two of the many sputum cultures taken during treatment with ampicillin yielded Rothia mucilaginosa, Klebsiella pneumoniae, Candida tropicalis, and Aspergillus fumigatus. In April 2016, he was admitted because of urinary tract infection. He died of aspiration pneumonia 9 days later (Figure 1).
Recurrent respiratory infections can occur either because the body is too weak to fight infection, there is structural damage to the lung or the causative organism is difficult to eradicate. A bacterial population usually triggers a marked inflammatory response with persistent production of purulent sputum.2 Maintenance azithromycin was not administered because it was ineffective in several of the patient's acute respiratory infections.
Long-term inhaled antibiotics are an excellent therapeutic option. The advantages of inhaled antibiotics are that they can produce high local concentrations in the airway giving good local efficacy with minimal systemic absorption and toxicity. Also, in bronchiectasis patients, inhaled antibiotics significantly reduce the sputum purulence and the need for intravenous antibiotics and hospitalization. This treatment should be prescribed indefinitely, since many patients can worsen clinically when it is discontinued.3 Although Pseudomonas aeruginosa infection in cystic fibrosis is the only approved indication for inhaled antibiotics, current national and international guidelines and recommendations include these treatments for the management of chronic bronchial infection for cystic fibrosis, bronchiectasis and chronic obstructive pulmonary disease3. Because there is no evidence that specific antibiotic presentations for the inhaled route are more effective than intravenous formulations, and since these are more expensive, ampicillin was chosen. Although 30-40% of patients with clinically stable bronchiectasis had no pathogens according to standard culture methods, even when using bronchoscopy specimens, they can have purulent sputum and experience respiratory infections.4 Using pyrosequencing analysis, Rogers et al. found that even though culture-based diagnostic microbiology is useful for detection of specific respiratory pathogens, other bacterial species may go unreported.5 Consequently, the antibiotic response was not always predictable from the results of the sputum culture.
Our case report indicates that nebulized ampicillin is an effective, well-tolerated, and safe therapy in patients with recurrent respiratory infections without bronchiectasis, irrespective of whether or not bacterial pathogens are identified in the lower respiratory tract.
Funding of the researchNo funding was received for the present case report, which was written based on clinical observations.
Artificial intelligence involvementNo of the material has been partially or totally produced with the help of any artificial intelligence software or tool.
Contribution of each authorLM and RN drafted the manuscript.
Conflicts of interest of every authorThe authors declare that they have no conflicts of interest.
We are grateful to all the doctors who cared for the patient during admission and at the outpatient clinic, especially José Luis Calleja, form Internal Medicine Department.