Percutaneous with radiological monitoring gastrostomy (PRG) is indicated in amyotrophic lateral sclerosis (ALS) patients who present with symptomatic dysphagia, dehydration, body mass index <18.5kg/m2 or weight loss greater than 10%.1 The puncture site of choice for PRG insertion is located in the lower third of the stomach, equidistant between the greater and lesser curvature and lateral to the rectus muscle.2,3 In ALS patients with paresis or paralysis of the left hemidiaphragm, the stomach is secondarily elevated and may be located intrathoracic, which may make PRG difficult or even impossible to perform.2,4 When this complication occurs, other access routes may be used. Angled subcostal access is reserved for cases where the stomach is partially visible near the costal cartilage margin, while intercostal access is used when the stomach is not visible below the costal cartilage margin.3,4
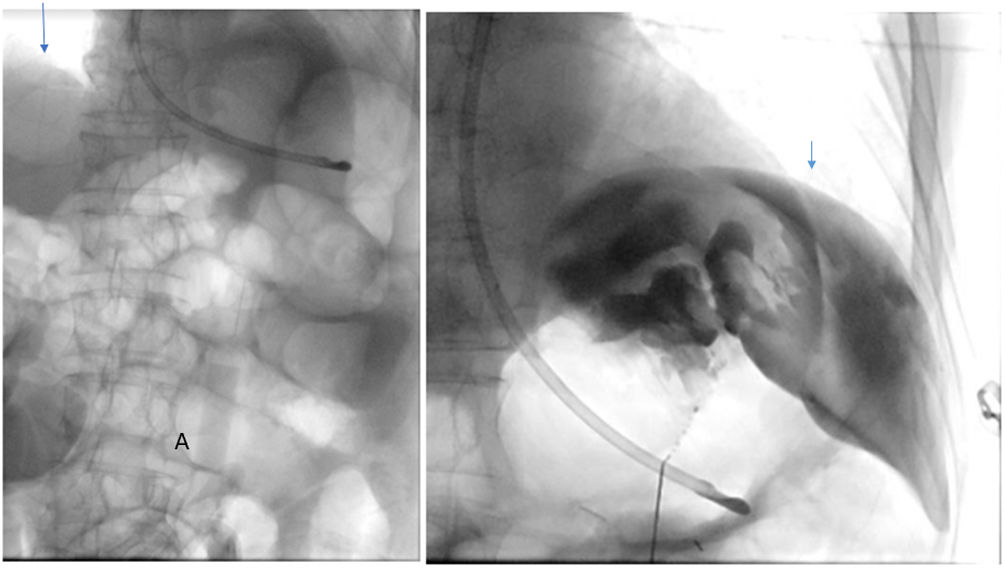
Two male patients, aged 79 and 69 years, with a diagnosis of ALS were admitted in our hospital for performing PRG. The first patient was using non invasive ventilation (NIV) at home while the second patient did not yet meet ventilation criteria. Diaphragmatic ultrasound in both patients showed bilateral diaphragmatic atrophy and paresis with muscle thickness <2mm and diaphragmatic excursion after deep breathing <6mm. In both cases, even after the introduction of air into the stomach, the intrathoracic location of the stomach and subcostal occupation by colonic structures was evident, and it was therefore decided to apply NIV in pressure support ventilation mode (PSV) in the patient already ventilated at home and with continuous positive airway pressure (CPAP) in the patient who was not chronically ventilated, increasing in both cases the positive end-expiratory pressure (PEEP) to 14cmH2O. Fig. 1 shows the different location of the gastric chamber with and without ventilation, achieving a stomach descent of up to 8cm. After administration of local anaesthetic, 2 gastropexies were inserted into the abdominal wall, and the PRG catheter was then placed. Once adequate location and patency had been verified, the patients were weaned from ventilation. In both cases, the procedure passed without incident or subsequent complications, and feeding through the gastrostomy could begin 24h after the procedure.
Fluoroscopy images performed during the radiological percutaneous gastrostomy (PRG) procedure. In the image on the left, the left diaphragmatic dome is not visible due to the very cranial location, which was maintained after air insufflation (the vertical arrow shows the right diaphragm and the letter A shows the procedure syringe), The second image shows the descent of the stomach after ventilation of the patient with an end-expiratory pressure of 14cmH2O (see arrow).
The main interest of the cases presented lies in the fact that there are no publications in the literature on the adjuvant indication of NIV to resolve the intrathoracic location of the stomach and facilitate subcostal access during PRG. By applying high PEEP, intrathoracic pressure is increased, which allows the descent of the diaphragm and consequently the abdominal viscera.
However, it should be noted that positive pressure ventilation has potentially harmful effects, the most important of which are on the patient's haemodynamics. Reducing venous return, decreasing cardiac output and systemic hypoperfusion are among the effects described.5
In view of the above, it is important to select well the patients to be treated with this technique. In conclusion, we believe that the use of NIV may be helpful during PRG in selected patients, although studies are needed to better evaluate the use and complications of the technique.
Conflict of InterestsThe authors state that they have no conflict of interests.