Exercise limitation is common in many respiratory diseases like chronic obstructive pulmonary disease (COPD), interstitial lung diseases (ILD), and pulmonary arterial hypertension (PAH).1–3 The six-minute walking test (6MWT) is widely used to assess exercise response in clinical practice.4 Also, previous studies have shown that 6MWT reflects equally well to the conventional constant-load test on the cycle ergometer the degree of impairment in hemodynamic response to exercise.5 The desaturation distance ratio (DDR) has recently been proposed as a potential integrative marker of exercise response that considers the distance walked during the test (6MWD) and the oxygen desaturation area estimated from the difference between the transcutaneous oxygen saturation value (SpO2) measured every minute vs. a theoretical maximum of 100%.6,7 We hypothesized that the difference between SpO2 and the SpO2 value determined at rest would better reflect the response to exercise in different diseases. This study tests this hypothesis by comparing the DDR values obtained using the original and the new method in patients (n=308) with three prevalent chronic respiratory diseases (COPD, ILD, and PAH). Besides, we sought to investigate the correlation of DDR with resting lung function measurements in these three diseases.
In this retrospective analysis, we included 104 patients with COPD, 104 with ILD, and 100 with PAH, all diagnosed according to international guidelines,8–10 who performed a 6MWT between October 2014 and May 2015. All patients were clinically stable, and none was participating in any rehabilitation program or clinical trial. We excluded patients on long-term oxygen therapy, mechanical ventilation, and/or tracheostomized. The study was approved by the Ethics Committee of our hospital (HCB/2017/0469).
Demographic and anthropometric parameters were recorded and resting lung function was measured following international standards.11,12 Reference values were those of Roca et al.13,14 In patients with PAH, pulmonary hemodynamics were determined by right heart catheterization, also following standard procedures.8 All participants performed a 6MWT according to the international guidelines.4 Reference values were those of Enright et al.15 During the test, SpO2 and heart rate (HR) were monitored continuously by Pulsox®-300 (Minolta Co., Tokyo, Japan). Absolute changes in SpO2 (ΔSpO2) were calculated by subtracting the values at baseline from those determined immediately after 6MWT was finished.16 DDR was calculated as the desaturation area (DA) over the 6MWD.7 DA was calculated using two different methods, the one proposed originally by Ijiri et al.7 (vs. a theoretical maximal SpO2 value of 100%), and the one tested in this study (vs. the actual SpO2 value determined in each patient at rest, before the 6MWT starts). Results are presented as mean±standard deviation for those distributed normally and as median and (25–75% percentile) for those non-normally distributed. Categorical variables are presented as proportions. ANOVA was used to compared groups. Correlations were assessed using Spearman's correlation test, and multivariable linear regression was used to explore the relationship of DDR with resting lung function variables, adjusted by age and BMI, in each of the three diseases studied here. A p value<0.05 was considered statistically significant.
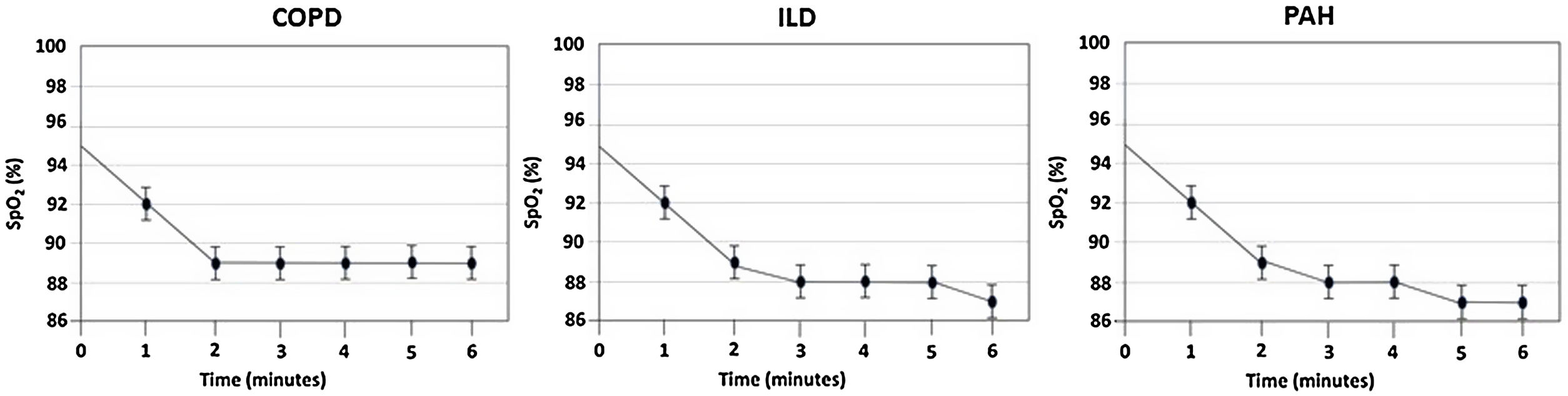
As shown in Table 1, most COPD patients were male, with a mean age of 66±8 years, and had moderate-severe airflow limitation and moderately decreased carbon monoxide diffusing capacity (DLCO). ILD patients were of similar age (68±11), but they included a higher proportion of females (45%) and showed a mild restrictive pattern with a moderate DLCO reduction. PAH patients were younger and mainly females, with normal spirometry and lung volumes but a moderately reduced DLCO; their mean pulmonary arterial pressure was 47 (39–54) mmHg (Table 1). The 6MWD was similar in all patients and generally well preserved. SpO2 at rest was lower in COPD and decreased during exercise in all diseases (Fig. 1). Using the calculation method initially proposed by Ijiri6,7 neither the DA nor DDR was significantly different across diseases (Table 1). By contrast, considering the resting SpO2 value in each individual as its own reference to calculate DA (and, therefore, DDR). Multivariable linear regression analysis showed that DLCO %pred. and resting SpO2 were independent determinants of DDR in all three diseases. Besides, we observed that, in COPD, the severity of airflow limitation (FEV1%ref) was also an independent DDR predictor.
Characteristics of participants and parameters determined during the 6MWT. Results are expressed as the mean±SD if data is normally distributed or as the median (25–75% percentile) if not.
| COPD (n=104) | ILD (n=104) | PAH (n=100) | |
|---|---|---|---|
| Age, years | 66±8 | 68±11 | 57±16* |
| Gender, n (% males) | 85 (82) | 57 (55) | 26 (26)* |
| BMI, kg/m2 | 27±5 | 29±5 | 27±5* |
| Smoking exposure, pack-years | 46 (35–71) | 1 (0–34) | 0 (0–14)* |
| FVC, % predicted | 75±16 | 69±18 | 85±18* |
| FEV1, % predicted | 46±17 | 71±17 | 78±19* |
| FEV1/FVC, ratio | 45±12 | 76±8 | 70±10* |
| TLC, %predicted | 106 (94–121) | 70 (55–82) | 90 (82–100)* |
| DLCO, %predicted | 51 (38–62) | 46 (33–59) | 54 (42–68)* |
| mPAP, mmHg | – | – | 47 (39–54) |
| 6MWD, meters | 456±98 | 473±113 | 452±119 |
| Borg dyspnea score at rest | 0 (0–2) | 0 (0–1) | 0 (0–1) |
| ΔBorg dyspnea score with exercise | 2 (1; 4) | 3 (1; 4) | 3 (1; 4) |
| SpO2 at rest, % | 95 (93–96) | 96 (94–97) | 96 (95–97)* |
| SpO2 at end, % | 91 (86–93) | 91(82–94) | 89 (83–93) |
| ΔSpO2 (at rest - at end), % | −4 (−8; −2) | −6 (−13; −2) | −7 (−11; −4)* |
| Original DA | 55 (40–77) | 54 (35–98) | 61 (40–83) |
| Original DDR | 0.121 (0.09–0.17) | 0.118 (0.07–0.21) | 0.133 (0.10–0.23) |
| New DA | 25 (11–38) | 28 (14–62) | 34 (21–55)* |
| New DDR | 0.052 (0.021–0.090) | 0.063 (0.029–0.144) | 0.075 (0.044–0.133)* |
Abbreviations: BMI, body mass index; FVC, forced vital capacity; FEV1, forced expiratory volume in the first second; TLC, total lung capacity; DLCO, diffusion capacity for carbon monoxide; mPAP, mean pulmonary arterial pressure; 6MWD, six-minute walking distance; SpO2, peripheral capillary oxygen saturation; DA, desaturation area; DDR, desaturation distance ratio.
The main findings of this study are that: (1) the calculation of DDR considering the resting SpO2 is more sensitive than the initially proposed method (that considered a theoretical reference value of 100% SpO26,7); and (2) DLCO and resting SpO2 were independent determinants of DDR shared by the three diseases studied here, plus the severity of airflow limitation in patients with COPD.
A few previous studies have investigated DDR (using the original method 6,7) in patients with ILD6 or COPD.17 Like in these previous studies, we found that the new DDR calculation in patients with ILD and COPD was significantly related to DLco and, to a lesser extent, to FEV1. To our knowledge, this is the first study to investigate DDR in patients with PAH, to contrast it with patients with ILD and COPD, and to investigate potential DDR correlations with lung function at rest in these three diseases.
We could not explore the potential prognostic value of DDR in these diseases because this study was retrospective. However, DLCO is a well-established prognostic factor in different chronic respiratory diseases,10,18 so its significant and independent relationship with DDR suggests that DDR may also be a good prognostic factor. This will have to be tested prospectively, but it is of note that Hsieh et al. have recently reported that the distance-desaturation product, an index similar to DDR, predicted 6-year mortality in a prospective study of 69 patients with stable non-CF bronchiectasis.19 Also, In 81 patients with IPF, Lettieri et al. found that each component of the 6MWT independently predicted mortality in IPF with greater accuracy than spirometry. However, a composite of both parameters, the distance-saturation product, provides slightly greater accuracy and represents a novel measure for assessing survival in these patients.20 On the other hand, DDR can be useful to assess the effects of a therapeutic intervention, such as the impact of supplementary oxygen during exercise or other.
Our study has strengths and limitations. Among the former, the description of a new method to calculate DDR in a large number of well-characterized patients with COPD, ILD, and PAH. Among the latter, its retrospective design. Additionally, we did not have information about the patient's exacerbations, which would have allowed a better characterization of the sample.
In conclusion, this study describes a new and more sensitive method to calculate DDR in patients with COPD, ILD, and PAH and shows that DLCO and resting SpO2 (plus airflow limitation in patients with COPD) were independent determinants of the new DDR. In terms of clinical implication, being new DDR a more sensitive method, it could offer information about response to drug's treatment and to rehabilitation programs.
Authors’ contributionsX. Alsina-Restoy: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. F. Burgos: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. R. Torres-Castro: Formal analysis, Writing – original draft, Writing – review & editing; Y. Torralba-García: Writing – original draft, Writing – review & editing; E. Arismendi: Writing – original draft, Writing – review & editing; J.A. Barberà: Writing – original draft, Writing – review & editing; A. Agustí: Formal analysis, Writing – original draft, Writing – review & editing; I. Blanco: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing.
FundingNone.
Conflict of interestsThe authors declare no conflict of interest directly or indirectly related to the manuscript contents except FB (which declares them in his COI).