Gastric heterotopias (GH) are clinical entity characterised by the localisation of gastric mucosa in any part of the gastrointestinal tract and has different clinical features due to the acid secreted. In the literature, no case diagnosed in the bronchial system has been encountered and here, we present a case of endobronchial gastric heterotopia mimicking lung cancer.1
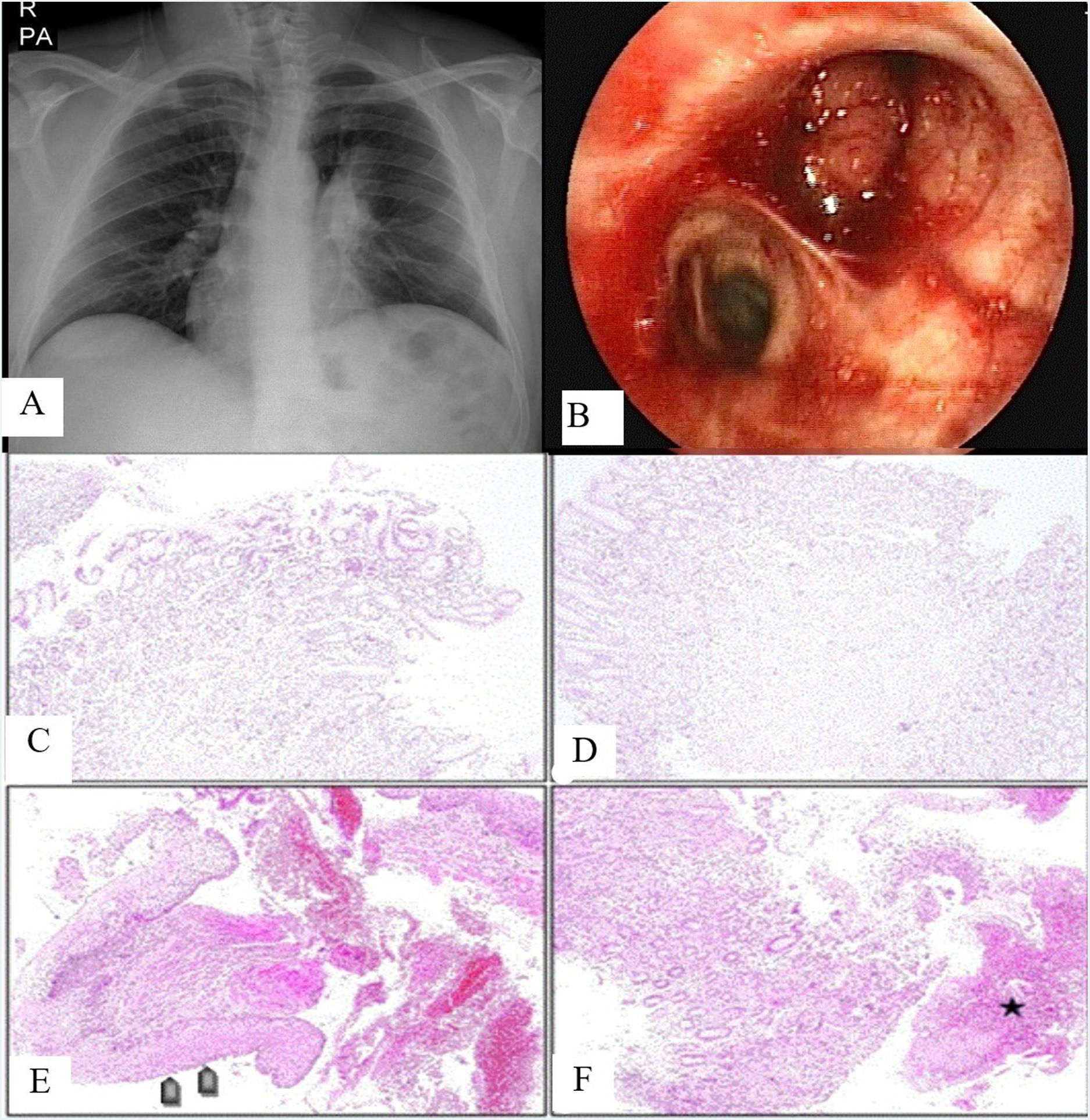
A 39-years-old male patient was admitted to our outpatient clinic with complaints of increased and progressive shortness of breath and cough for about 4 months. He hadn’t comorbidities and smoking history. Laboratory parameters were within normal limits except high C-reactive protein (56mg/l) and leukocytosis (12×109/l). There was a hilar enlargement, parahilar consolidation and elevation of diaphragm in left hemithorax in the chest X-ray (Fig. 1A). Thorax CT revealed non-specific consolidated area of 85mm×45.3mm in the left hemithorax, and atelectasis from left upper lobe anterior segment to superior and inferior segments of lingula.
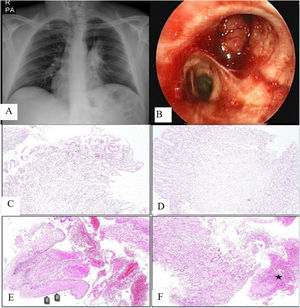
(A) Chest X-ray of the patient on admission. (B) Fibreoptic bronchoscopy revealed endobronchial lesion obstructing the upper lobe of the left lung. (C and D) Chronic inflamed pyloric type gastric mucosa in a bronchoscopic biopsy specimen (H&E, ×100). (E) Areas of focal squamous metaplasia (arrows) in a repeated biopsy sample from the same patient from the same site (H&E, ×100). (F) Samples of inflamed gastric mucosa as well as ulcer surface and floor (area marked with an asterisk) (H&E, ×100).
Fibreoptic bronchoscopy was performed and revealed an endobronchial lesion that completely obstructing the bronchi of the upper lobe of the left lung (Fig. 1B). Fine needle aspiration biopsy, forceps biopsy were performed. The histopathological assessment of forceps biopsy specimen revealed chronic inflammatory gastric mucosa and gastric heterotopia in the bronchial system. Bronchoscopy was repeated because such a disease in the bronchial system hadn’t been reported previously. And the histopathological assessment of the second forceps biopsy confirmed the previous diagnosis (Fig. 1C–F). He was considered gastric heterotopia and was referred to Department of Thoracic Surgery for operation.
Heterotopy is the presence of normal physiological tissue in an atypical location and gastric heterotopy may be found in the gastrointestinal and hepatobiliary system. It is usually seen in the proximal oesophagus but it has also been shown to be present in the small intestine, rectum and bile ducts.1,2
The pathogenesis of GH is uncertain and there’re hypotheses proposing that it's congenital or acquired. It's commonly thought to be of congenital origin and is thought to result from an error during embryogenesis or faulty differentiation of pluripotent endodermal stem cells in the intestine. On the other hand, some hypotheses suggest that chronic damage due to infectious and inflammatory processes may cause injury to the mucosa and subsequent abnormal regeneration leading to gastric heterotopia.3,4
GH is usually asymptomatic and is often recognised incidentally. Symptoms depend on the location of the GH and are related to acid secretion. It may cause chest pain, chronic cough, abdominal pain, haemorrhage.3,4
Gastric heterotopia lesions may be mucosal or submucosal. Macroscopic appearance is characteristically mucosal nodularity or polypoid lesion as in outpatient. Gastric heterotopia may be difficult to diagnose due to its rarity and non-specific clinical features and radiological findings. The gold standard for the diagnosis of GH is histology.4,5
In conclusion, as a result of our literature review, we realised that our case was the only case of gastric heterotopia of the bronchial system outside the gastrointestinal and hepatopiliary systems. Due to its location in the bronchial system, it may cause respiratory symptoms such as shortness of breath, cough, hemoptysis and may be confused with other diseases, especially malignancies.
Funding
We don’t have any source of funding.
Conflict of interestsAll authors have no, real or perceived, direct or indirect conflicts of interest that relate to this manuscript.