Bronchogenic cysts are uncommon congenital lesions usually located in the mediastinum or lung and resulting from abnormal budding of foregut in the embryonic stage.1,2 Malignant transformation is very rare and only few well-documented cases have been reported.3–8 In these cases, histological findings were bronchioalveolar carcinoma, adenocarcinoma, squamous cell carcinoma and large cell carcinoma. To the best of our knowledge, this is the first case of enteric adenocarcinoma arising from an intrapulmonary bronchogenic cyst.
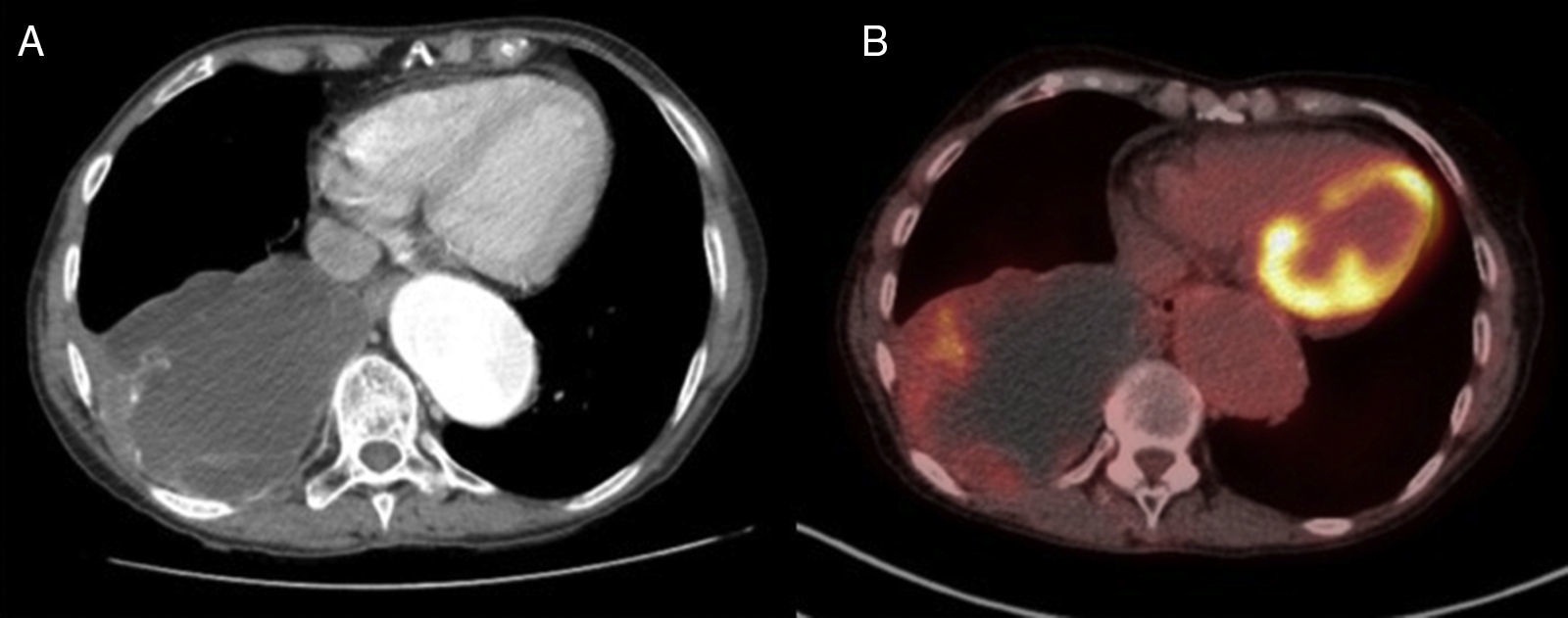
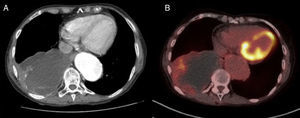
A 76-year-old woman with a medical history of hypertension, hypercholesterolemia, hypoacusis, glaucoma, rheumatic polymyalgia and bronchial asthma was referred to our centre for surgical resection of a bronchogenic cyst diagnosed 12 years previously in another hospital. The patient, a farmer, did not have any allergies or toxic habits. She was completely asymptomatic, and physical examination only revealed an absence of breath sounds in the posterior right lower hemithorax. All laboratory tests were normal. The computed tomography (CT) showed a 10.6cm mass in the right lower lobe with calcified walls, which was compatible with bronchogenic cyst (Fig. 1A). The bronchoscopy showed an irregular white endobronchial mass at the entrance of the right lower bronchus, which also affected and partially occluded the middle lobe bronchus. The histology of the endobronchial lesion was mucinous adenocarcinoma of the lung. Based on these findings, a PET-CT was performed, which showed an ametabolic mass with a mild increased uptake in the peripheral area and in mediastinal lymph nodes (Fig. 1B). The patient underwent functional pulmonary testing and was considered eligible for surgery. She underwent right lower lobectomy with lymph node dissection through muscle-sparing thoracotomy. The postoperative period was uneventful and the patient was discharged 6 days after surgery.
Definitive histology of the specimen was infiltrating colloid adenocarcinoma with immunophenotype of enteric adenocarcinoma arising from a benign cystic mucoid lesion compatible with bronchogenic cyst. Immunohistochemical staining was positive for cytokinin 20 and CDX 2, and negative for cytokinin 20 and TTF1. Mediastinal lymph nodes were not affected.
The final diagnosis was enteric adenocarcinoma arising from a bronchogenic cyst. No additional lesions were found on colonoscopy and further abdominal exams. Because no signs of disease dissemination were found, no additional therapy was applied. The patient is alive without recurrence of disease 6 months after the surgery.
Bronchogenic cysts are congenital lesions thought to originate from the primitive ventral foregut,2 and are the result of abnormal budding that “pinches off” from the tracheal tree in the stage when bronchial buds develop into the primitive of respiratory tree.9,10 Bronchogenic cysts are relatively rare, with a prevalence of 1/68,000–1/42,000.11 Almost 90% have been reported in the mediastinum, especially in the posterior superior portion.12
Although extremely rare, malignant transformation of a bronchogenic cyst is well known and has been reported in several cases.3–8 In a systematic review13 published in 2010, the authors included 683 adult patients with a diagnosis of bronchogenic cyst; in 5 patients (0.7% of all those studied), bronchogenic cysts were associated with malignancies: 1 squamous cell, 1 adenocarcinoma, 2 bronchioalveolar carcinomas and 1 large-cell anaplastic carcinoma. It was not stated whether the indication for surgical resection was due to the detection of malignant transformation or whether malignant cells were an incidental finding, but in all cases the carcinoma was found in the cyst wall. To the best of our knowledge, this is the first case of bronchogenic cysts associated with an enteric adenocarcinoma and, in this case, malignant degeneration was the reason for surgical resection. Although there is scant evidence on carcinogenesis in a bronchogenic cyst, some studies suggests that unstable epithelial cells in the cyst wall could have malignant potential and lead to the malignant degeneration.
Surgical excision of bronchogenic cysts has historically been performed for 3 main reasons: (1) to confirm diagnosis; (2) to prevent development of symptoms and/or complications and to pre-empt the possibility of surgery on complex inflammatory lesions; and (3) to avoid any potential for malignant degeneration. However, in the reported case, no surgical treatment was requested until the malignant transformation was discovered 12 years later. Nowadays, the evidence for conservative management of asymptomatic bronchogenic cyst is very limited, and we must take into consideration that approximately 45% of patients who are asymptomatic at the moment of diagnosis will eventually develop symptoms or complications,13 and there is a risk of secondary tumours arising from a bronchogenic cyst.
In conclusion, we report the first case of a patient with an enteric adenocarcinoma arising from a longstanding bronchogenic cyst. We consider that surgical excision of bronchogenic cysts should be recommended even in asymptomatic patients, the aim being to preclude malignant degeneration, prevent complications or the development of symptoms, and to confirm diagnosis. Conservative management should be offered only if close long-term follow-up can be guaranteed.